Introduction
Rhinovirus is an single-stranded Ribunucleic acid (RNA) virus recognised as one of the most common viruses causing human upper respiratory tract infections worldwide. The common clinical presentations include rhinorrhea, cough, nasal congestion, headache, malaise, and fever. These symptoms are typically mild and self-limited. Reference Vandini, Biagi, Fischer and Lanari1 Viral infection is one of the common causes of acute myocarditis. The common viral infections that can cause acute myocarditis are adenovirus, enterovirus, herpes viruses, influenza, and coronavirus. Reference Ammirati and Moslehi2 Cardiac arrhythmia can be found in 3-40% of acute myocarditis cases that commonly present with tachyarrhythmia. Reference Pruitt, Menon and Lal3
We report a rare clinical presentation of acute myocarditis in a child who presented with rhinovirus infection associated with acute myocarditis with complete heart block, highlighting an important case from tertiary care hospital in northern Thailand.
Case presentation
The case involves a previously healthy 9-year-old Thai boy who presented to the outpatient clinic with a two-day history of low-grade fever, rhinorrhea, cough, diarrhoea, and vomiting. Viral respiratory polymerase chain reaction testing confirmed rhinovirus infection, prompting admission due to moderate dehydration. During hospitalisation, he complained of chest pain and experienced a generalised tonic-clonic seizure. Physical examination revealed an irregular heart rate, with vital signs indicating a temperature of 36.6 degrees celsius, pulse ranging from 40 to 200 beats per minute, respiratory rate of 24 per minute, and blood pressure of 90/60 mmHg. He appeared fatigued with pallor. Electrocardiogram showed a complete heart block and ST-segment elevation in V1 and V2 (Figure 1). Chest X-ray displayed cardiomegaly with increased perihilar interstitial infiltration. Echocardiogram revealed a pericardial effusion measuring 0.44 cm in diameter, mildly decreased left ventricular systolic ejection fraction (left ventricular ejection fraction (LVEF) 42%), and trivial tricuspid and mitral regurgitation. The cardiac index was 3.5 L/m2/min. Laboratory investigations demonstrated a haemoglobin level of 10.5 g/dL, leukocytosis with a white blood cell count of 8200 per cubic millimetre, serum total bicarbonate of 10.0 mmol/L, elevated C-reactive protein of 23.7 mg/L, and markedly elevated Troponin T level of 619.7 pg/mL. Treatment commenced with pulse methylprednisolone and adrenaline for myocarditis with heart block. The patient was then referred to a tertiary care hospital and admitted to the paediatric cardiac ICU.
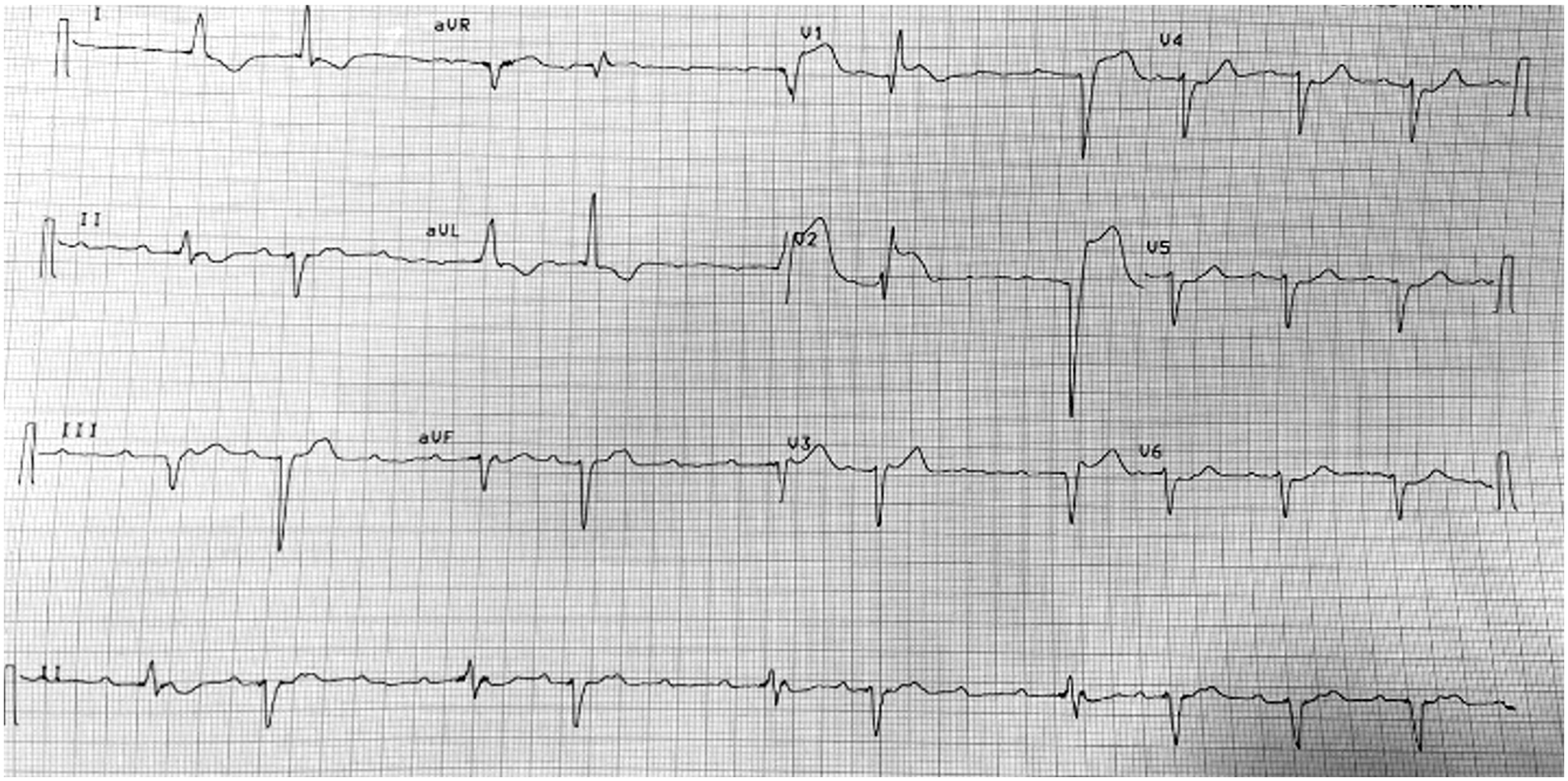
Figure 1. Electrocardiogram on admission. A complete heart block and ST-segment elevation was observed.
Despite treatment, the patient’s cardiovascular status remained unstable, with heart rate fluctuations between 60 and 110 beats per minute. Electrocardiography still revealed a complete heart block and ST-segment elevation. Follow-up of the echocardiogram showed a reduced LVEF of 48%. Temporary cardiac pacing was performed. Treatment included supportive care, intravenous methylprednisolone, adrenaline infusion, and intravenous immunoglobulin. Over five days, the patient’s condition improved, and he was weaned off inotropic support and the pacemaker. Following pacemaker removal, his pulse ranged between 50 and 60 beats per minute, with an electrocardiogram revealing a first-degree atrioventricular block. Echocardiogram follow-up indicated left ventricular hypertrophy with LVEF of 73.9% and a small pericardial effusion. The Troponin I level decreased to 324 pg/mL.
Cardiac MRI performed ten days after admission confirmed acute myocarditis based on the Lake Louise criteria of 2018. Evidence of myocardial oedema, fibrosis, and small bilateral pleural effusion was noted. Six months later, clinical and cardiac MRI follow-up demonstrated complete recovery, with normal biventricular size and function, improved myocardial oedema, and no pericardial effusion (Figure 2).

Figure 2. Cardiovascular magnetic resonance (CMR) of patient. (left column) CMR, at day 10 after admission, demonstrated global oedema in T2-based imaging, the left ventricle (LV) global T2 was 58.7 ms (Abnormal findings: T2 ≥ 52.18 ± 3.4 ms), and extracellular volume (ECV) was 34% ms (Abnormal finding: ECV>30.4%). (Right column) CMR, at 6 months after onset of illness, demonstrated improvement of myocardial oedema and CMR parameters.
Discussion
Rhinovirus infection in children commonly causes upper respiratory tract infection, and most do not cause severe symptoms. We present atypical clinical manifestations of acute myocarditis along with complete heart block in a young patient who was diagnosed with rhinovirus infection.
Acute myocarditis can be caused by infection, with viral infection being the most common. The pathophysiological mechanisms of viral myocarditis are injury and death of cardiomyocytes by infiltration of the tissue with immune cells and viral damage. Reference Law, Lal and Chen4 Cardiac arrhythmia is a common clinical manifestation in patients with acute myocarditis, accounting for 3–40% of cases. Tachyarrhythmia is common. Cathalee et al. reported a prevalence of complete heart block in 8.6% of patients diagnosed with acute myocarditis. Reference Pruitt, Menon and Lal3 The pathogenesis of atrioventricular conduction disturbance is an inflammatory change of the conduction system, mainly in right bundle branches and left bundle branches, especially in the terminal portions. Reference Wu5 We reported here an unusual clinical presentation of rhinovirus infection in a child presenting with seizure and complete heart block. The precise reasons for arrhythmias and heart blocks stemming from viral-induced acute myocarditis are not fully understood. Acute myocarditis is still a leading cause of atrioventricular (AV) block in young people. Bhasin V et al. described a patient with coronavirus disease 2019 myocarditis who experienced a reversible complete heart block following high-dose steroid treatment, Reference Bhasin, Carrillo, Ghosh, Moin, Maglione and Kassotis6 similar to the case we presented. Following treatment, there was a rapid alleviation of the systemic inflammatory response, which provided a resolution for the complete heart block.
Myocarditis can cause myocardium degeneration and dysfunction, leading to myocardial hypertrophy, enlargement of cardiac chambers, and progression to dilated cardiomyopathy. Reference Lei, Cao, Wu, Lu, Ni and Hu7 Chow et al. reported a case of a 27-year-old female who presented with acute onset of dyspnoea and polymerase chain reaction (PCR) testing for rhinovirus was positive. This patient was then found to have dilated cardiomyopathy. Reference Chow, Murphy, Subedi and Jyothidasan8 Agen et al. reported a case of 4.5-year-old boy with breathlessness, severe dilatation and decreased left ventricular systolic function, and molecular tests were positive for rhinovirus infection. Conversely, our case did not undergo progression to dilated cardiomyopathy.
Our study has several limitations. We did not perform a myocardial biopsy to confirm the diagnosis of myocarditis. However, cardiac MRI was used to diagnose myocarditis and follow-up on this patient. We could not identify the subtype of rhinovirus, whereas some studies reported the specific subtype of rhinovirus that causes dilated cardiomyopathy. We suggest long-term follow-up of the progression of disease in this patient.
In conclusion, we reported atypical manifestation of rhinovirus in a child with acute myocarditis presenting with seizure and complete heart block. Although rhinovirus is a common cause of upper respiratory tract infection, it can also cause viral myocarditis and dilated cardiomyopathy.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951124036059.
Acknowledgements
Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
Author contribution
Rattakarn Yuwattana: drafted the initial version of this paper, and reviewed and revised this paper; Kunthika Singhasee: drafted the initial version of this paper, and reviewed and revised this paper; Kwannapas Saengsin: reviewed and revised this paper; All authors contributed to the article and approved the submitted version.
Financial support
None.
Competing interests
None.
Ethical standard
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for his images and other clinical information to be reported in the journal. The patient’s parents understand that the patient’s name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.





