Gynecologic malignancies are among the cancers that affect most women in Latin America and the Caribbean. In 2020, the most common gynecologic cancers in the region were cervical, corpus uteri, and ovarian cancer, with age-standardized incidence rates of 14.9, 8.2, and 5.8 cases per 100 000 people, respectively. 1 In Puerto Rico (PR), gynecologic cancers represented 16% of all cancers diagnosed in women from 2016–2020. 2 The Puerto Rico Central Cancer Registry (PRCCR) 2 reported age-adjusted incidence rates (per 100 000 people) between 2016 and 2020 to be 30.0 for corpus uteri, 12.0 for cervical, and 7.8 for ovarian cancer. Considering women’s role as primary caregivers, health outcomes in women extend to families and society, directly influencing the well-being of all. Reference Onarheim, Iversen and Bloom3 This is particularly important in Puerto Rican culture, since for the period of 2017–2021, 46% of the households with children ages 0–17 years were headed by single mothers, and the median income among single mothers with children under 18 years was only US $10,077. 4 These indicators highlight the key role of women in PR’s society.
The aftermath of a natural disaster, such as a hurricane, presents great burdens and challenges, especially to those with chronic conditions. These challenges can include a disrupted health care system, communication difficulties, and loss of transportation services. Reference Man, Lack, Wyatt and Murray5 A recent study in PR documented the stressors and experiences of patients with gynecologic cancers after Hurricanes Irma and María and reported that disruptions in oncology care were common due to serious damage in the health care infrastructure, along with a lack of electricity and clean water. Reference Calo, Rivera and Mendez-Lazaro6 Certain challenges, particularly those related to accessing medical care for cancer patients, directly correlate with anxiety, perceived stress, and post-traumatic symptomatology in the context of a natural disaster. Reference Rodriguez-Rabassa, Hernandez and Rodriguez7 Previous studies have shown that lack of access to medical care lead to treatment interruptions, that can also cause psychosocial and psychological distress in cancer patients, contributing to disease progression. Reference Rodriguez-Rabassa, Hernandez and Rodriguez7
Continual and uninterrupted cancer treatment is key for better outcomes or prognoses among cancer patients. Delays in treatment can have serious consequences on survival outcomes, including for gynecological cancers, Reference Man, Lack, Wyatt and Murray5 especially if the interruption is related to a natural disaster. In 2017, within 2 weeks, PR was hit by two catastrophic hurricanes: Irma (September 7, 2017—Category 5) and María (September 20, 2017—Category 4). 8 These hurricanes affected power systems, water supply, communications systems, and health systems, among other essential services, throughout the island. 8 During the months following the aftermath of Irma and María, the health system became inoperant.
Little is known about the potential increased risk of death among cancer patients in PR following the hurricane season of 2017. We aimed to evaluate the impact of treatment interruption on the survival of women with gynecologic cancer in PR following Hurricanes Irma and María.
Methods
This retrospective cohort study included women diagnosed with gynecologic cancers before Hurricanes Irma and María hit PR, who reported receiving cancer treatment. Recruitment occurred through five gynecologic oncology clinics across the island, and physicians provided patient’s contact information. After telephone-based informed consent was obtained from eligible women, they completed a telephone interview that assessed information about demographics, clinical and lifestyle characteristics, and the impact of the hurricanes on their treatment and health outcomes. If a participant was unable to give consent or had passed away, their caregiver was interviewed as a proxy. In total, 271 women were interviewed from September 2019 until November 2020. To confirm their cancer diagnosis and vital status, we matched the study’s database with the PRCCR database. This match allowed us to confirm the date and age at the time of cancer diagnosis, type of cancer, tumor stage, vital status, and date of last contact (if a patient had passed away, this date corresponds to her death date). The PRCCR updated cancer patients’ vital status by linking its database with the PR Demographic Registry Mortality File (cutoff—2019).
Gynecologic cancer types were assessed using the International Classification of Diseases for Oncology, third revision (ICD-O-3) codes: C510-C519; C529; C530-C539; C540-C549; C569; C570-C579. Out of 271 women, 259 (95.6%) matched with a cancer diagnosis, 3 were excluded due to a diagnosis outside of the gynecologic category, resulting in a sample of 256 participants. Fifty-four women were excluded due to pre-January 2016 diagnoses (less likely to be in active treatment), and one woman reported no cancer treatment, leaving a subsample of 201 women. From these, 112 were diagnosed before the hurricanes and 89 afterwards. Given the focus of the current work, our analysis included 112 women who were receiving cancer treatment and diagnosed with gynecologic cancer before the hurricanes (January 1, 2016–September 6, 2017). In terms of treatment, we first defined those in at least one treatment before the hurricanes (i.e., receiving treatment) using the following question: “Were you on this treatment BEFORE the hurricanes hit in September 2017?” Then, we defined treatment interruption based on whether they were receiving treatment or not, through this question: “Was this treatment interrupted because of Hurricanes Irma and Maria?”
The primary outcome of the study was vital status (dead or alive). As an indicator of treatment interruption, the main predictor variable was defined as the status of treatment at the time of the hurricanes, which was defined as (1) treatment completed (only had surgery) without reported interruption; (2) receiving treatment before the hurricanes and did not have interruption; and (3) receiving treatment before the hurricanes and had an interruption. In addition, this variable was also categorized into two categories that defined treatment interruption as a binary variable (yes or no). Other covariates of interest included age at the time of diagnosis (years), stage of cancer (localized, regional, distant), and type of gynecologic cancer—vulvar (C51), vaginal (C52), cervical (C53), corpus uteri (C54), ovarian (C56), and other female genital organs (C57).
A descriptive analysis using frequencies was performed to describe the sociodemographic and clinical variables of women who received cancer treatment. Factors associated with treatment interruption and vital status were evaluated using the Pearson’s Chi-squared test or Fisher’s exact test. A survival analysis was performed following the women from their date of cancer diagnosis until December 31, 2019, to evaluate survival after diagnosis. The follow-up period was determined by whether the women had passed away or not. If the event did not happen during the follow-up period, the data was censored until December 31, 2019. Kaplan-Meier survival curves were used to describe cancer survival by relevant covariates, and the Log-Rank test was used to indicate whether there was a statistically significant difference between the curves over time. Cox proportional hazards models were used to assess the crude and covariate-adjusted association between treatment interruption and vital status (dead or alive). Statistical significance was defined as P < 0.05.
The Institutional Review Board (IRB) of the University of Puerto Rico, Medical Sciences Campus (#A1810418), approved this study.
Results
Most women had an age of diagnosis ≥ 56 years (58.0%), were unmarried (52.0%), had greater than a high school education (65.5%), earned a household family income ≤ US $19,999 (59.2%), and had public health care coverage (60.4%). Clinical variables showed that the most common gynecologic cancers in the study population were corpus uteri (58.9%), cervical (17.9%), and ovarian cancer (17.8%). On the other hand, vaginal (0.9%), vulvar (2.7%), and other gynecologic cancers (1.8%) were less common. Most women were diagnosed at localized stage (65.2%), followed by regional (25.9%) and distant (8.9%) stages. Regarding vital status, 8.9% of women diagnosed before the hurricanes died during the follow-up period (5 women with corpus uteri, 3 with cervical, and 2 with ovarian cancer) (data not shown).
With respect to treatment modalities, the most common were surgery (91.1%) and chemotherapy (44.6%), followed by brachytherapy (25.9%), radiotherapy (23.2%), and other treatments/alternative medicine (2.7%) (Table 1). Additionally, 56.3% of women received multiple or a combination of treatments. Overall, 75.9% of participants were receiving treatment before the hurricanes. However, although 21.2% of them were receiving treatment before the hurricanes and had interruptions, the treatments with more interruptions were chemotherapy (34.4%) and brachytherapy (33.3%) (see Table 1). Regarding treatment status at the time of the hurricanes for the overall study population (n = 112), 16.1% of women receiving treatment before the hurricanes had treatment interruptions, while 83.9% did not. This last group included 24.1% of women from the study population who completed treatment (only had surgery) without any reported interruption, and 59.8% who were receiving treatment before the hurricanes who were not interrupted (data not shown).
Table 1. Types of treatments and treatment interruption among women diagnosed before the hurricanes (n = 112)

* Based on the study sample (n = 112).
** Based on each individual treatment; women may have received more than 1 treatment.
*** Based on each treatment before the hurricanes.
Categories are not mutually exclusive.
On bivariate analysis, women who had treatment interruptions had higher proportions of being aged ≤ 55 years (66.7% versus 37.2%), diagnoses with regional/distant stage (55.6% versus 30.9%), and receiving more than one cancer treatment (83.3% versus 53.1%), compared to those without treatment interruptions (P < 0.05). Concerning mortality, 22.2% of women with treatment interruptions died, compared to 6.4% of women without treatment interruptions (P < 0.05) (data not shown).
Kaplan-Meier curves showed a clear overlap in the survival curves for women without treatment interruptions (those who completed treatment before the hurricanes and those receiving treatment but had no interruption) (Log-Rank test: P > 0.05) (Figure 1a). When these categories were combined and this variable was dichotomized (no treatment interruption), a decrease in survival was observed in women with treatment interruptions as compared to those without treatment interruptions (Log-Rank test: P < 0.05) (see Figure 1b). The Cox proportional model showed an increased risk of death among women with treatment interruptions (HR: 3.88, 95% CI: 1.09–13.77). Although the model adjusted by age and cancer stage was not statistically significant, the magnitude of association persisted (HR: 2.49, 95% CI: 0.69–9.01) (data not shown).
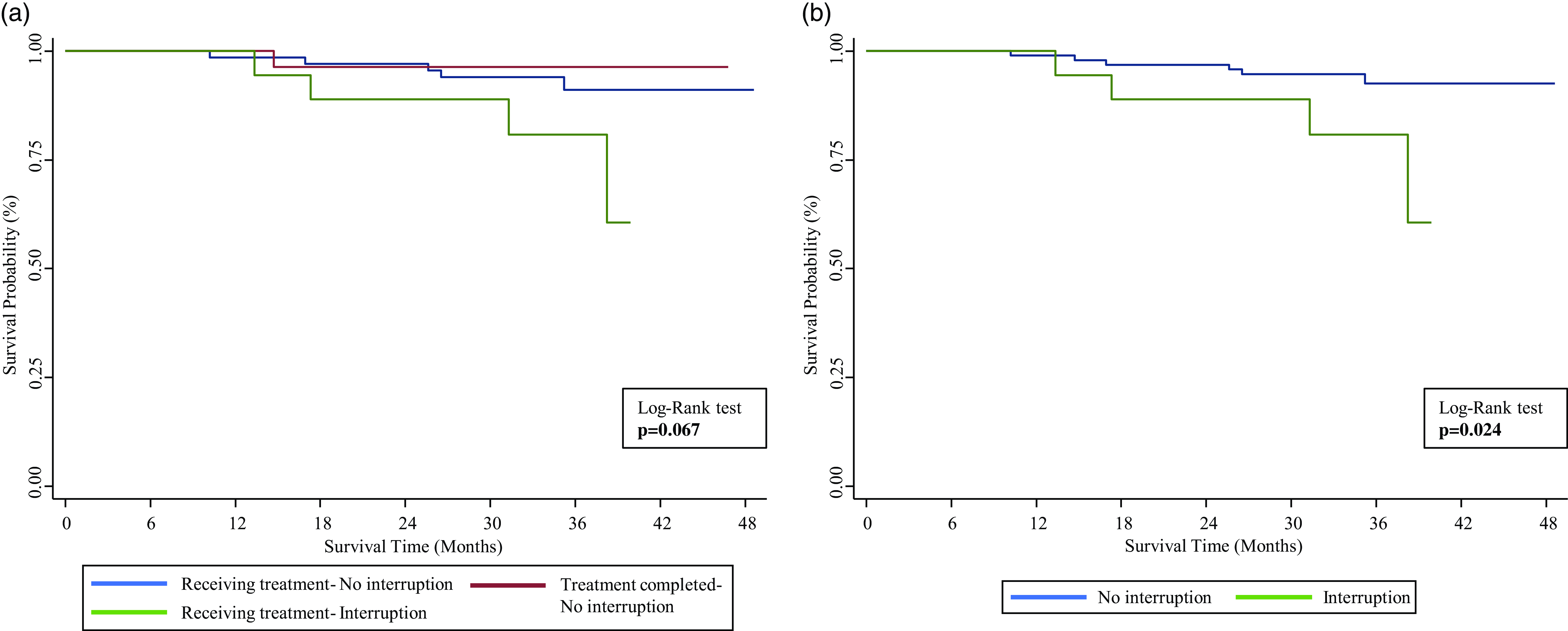
Figure 1. Kaplan-Meier Survival Estimates for Treatment Status (n = 112).
Discussion
This is the first study to document the impact of Hurricanes Irma and María on treatment interruptions among gynecologic cancer patients and their impact on disease outcomes in PR. Our study evidenced that over 16% of women in the study population had treatment interruptions due to the impact of Hurricanes Irma and María. Among specific treatments, brachytherapy and chemotherapy were the most interrupted (33%–34%). Lower interruptions in radiotherapy (19%) could be related to coordinated efforts of radiotherapy facilities in PR that aimed to reduce treatment interruptions among radiotherapy patients after the hurricanes. Reference Gay, Santiago and Gil9
Study findings also showed a two- to threefold increased risk of death among women with treatment interruptions. This result is consistent with the literature since survival worsens as treatment interruptions occur and is consistent with the evidenced detrimental effect of treatment interruptions on cancer patients, especially if the interruption occurs in the context of a natural disaster. Reference Man, Lack, Wyatt and Murray5 Future research should assess treatment delays, recognizing that the study evaluated treatment interruption exclusively in women diagnosed before the hurricanes. Such delays may substantially affect survival outcomes, Reference Man, Lack, Wyatt and Murray5 and could be linked to the damage in health care infrastructure that persisted in PR after the hurricanes. Reference Calo, Rivera and Mendez-Lazaro6 Future research should also evaluate the impact of biopsychosocial variables on both treatment interruption and survival, as these factors have previously been shown to be associated. Reference Rodriguez-Rabassa, Hernandez and Rodriguez7
Limitations
A limitation of this study is the reduced sample size, which may impact statistical power and generalizability. Additionally, information on treatment interruption was self-reported, and asked over two years after the events, posing the possibility of recall bias. Furthermore, women were interviewed once, with no follow-up interviews. However, a strength of this study was that the survival and other clinical characteristics were confirmed with the PRCCR database.
Conclusion
The increased risk of death observed among gynecologic cancer patients who experienced treatment interruptions emphasizes the critical need for effective strategies to minimize treatment delays and ensure ongoing care post-disaster in this vulnerable population. Findings support the need for more infrastructure and disaster management plans in PR that should anticipate and prevent the interruption of treatment in cancer patients. As previously recommended by Ortiz et al., Reference Ortiz, Calo and Mendez-Lazaro10 while emergency response plans should be housed within the emergency support function infrastructure of each state and territory in the United States, the Centers for Disease Control and Prevention’s Comprehensive Cancer Control Plans provide an essential mechanism to support these efforts for cancer patients. At a local level, oncology clinics and care providers should establish emergency protocols for these events, which may include patients’ contact information, alternative clinics, and access to medical information to ensure continuity of care. As the strength and frequency of natural disasters increases, emergency preparedness for cancer patients is vital.
Author contributions
Data collection: García-Camacho, Martínez-Ocasio, Ortiz, Torres-Cintrón. Methodology and design: Rivera-Gastón, Ortiz, Umpierre-Catinchi. Analysis and interpretation of data: Rivera-Gastón, Ramos-Cartagena, Ortiz-Ortiz, Ortiz. Drafting of the manuscript: Rivera-Gastón, Ortiz, Umpierre-Catinchi, Ramos-Cartagena. Critical revision of the manuscript: All authors. Statistical analysis: Rivera-Gastón, Ramos-Cartagena, Ortiz-Ortiz, Torres-Cintrón. Supervision: Umpierre-Catinchi, Ortiz.
Funding statement
This project was fully funded by the National Cancer Institute (NCI) Grant # 1R21CA239457-02 and supported by the Cancer Prevention and Control (CAPAC) Research Training Program (NCI Award Number R25CA240120) and a grant from the National Program of Cancer Registries (Grant #NU58DP007164) given to the Puerto Rico Central Cancer Registry (PRCCR) at the UPR Comprehensive Cancer Center.
Competing interests
The authors declare no conflicts of interest within the scope of this work.




