90 results
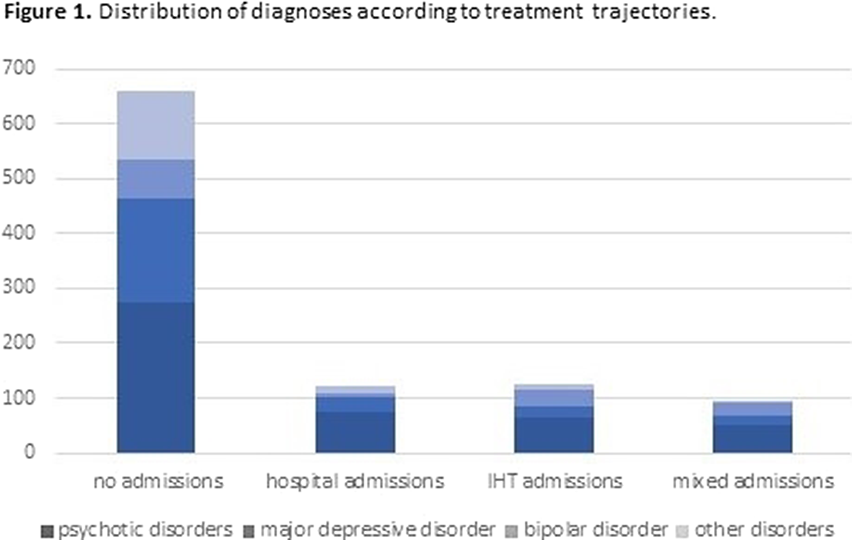
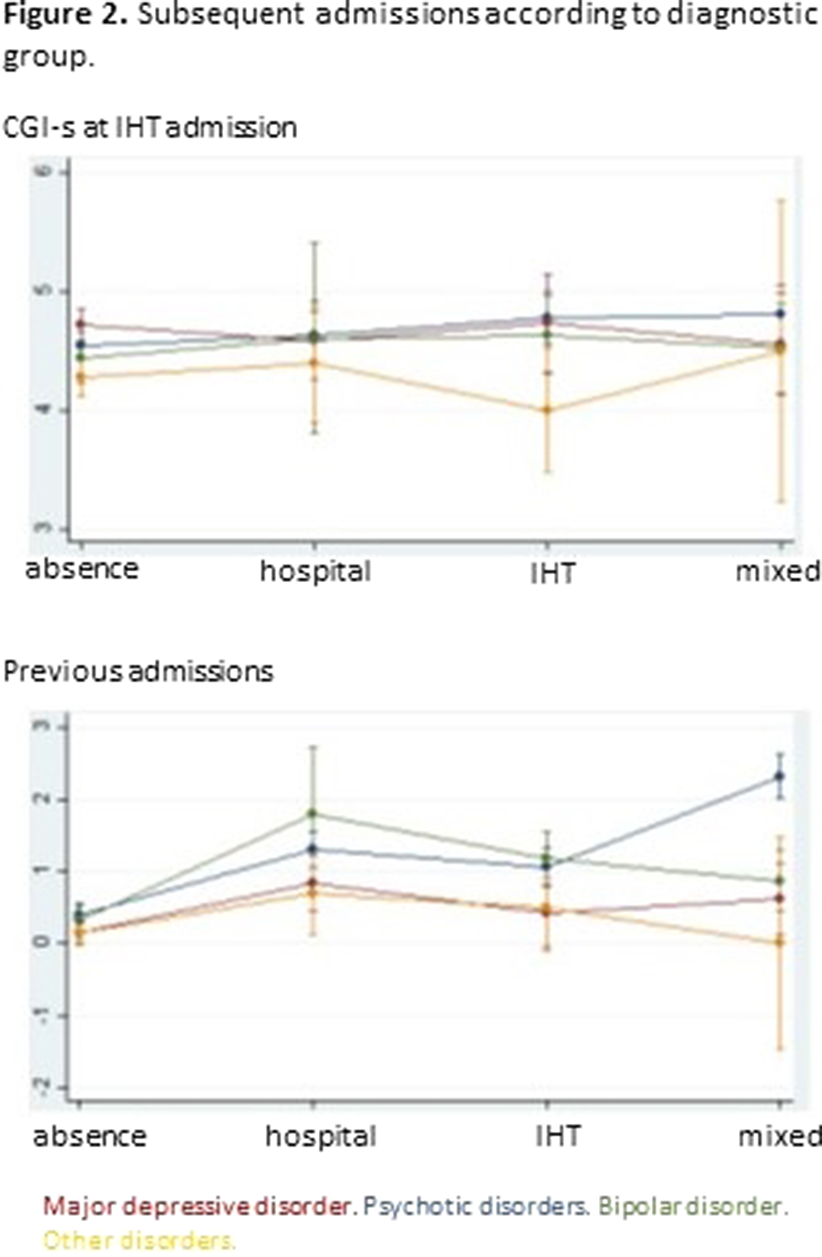
Does intensive home treatment change treatment trajectories of psychiatric disorders?
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S167-S168
-
- Article
-
- You have access
- Open access
- Export citation
Off-label use of atypical antipsychotics- Where are we?
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S305
-
- Article
-
- You have access
- Open access
- Export citation
Knocking on the Doors of Perception: the role of psilocybin in substance use disorder treatment
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S270
-
- Article
-
- You have access
- Open access
- Export citation
Suicide among physicians: what do we know about it?
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1115-S1116
-
- Article
-
- You have access
- Open access
- Export citation
Psychosis in Parkinson’s Disease: a Case Report of Diagnosis and Management
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S1085
-
- Article
-
- You have access
- Open access
- Export citation
Postpartum Delirium: A Psychosis Born in the 18th Century
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S1128
-
- Article
-
- You have access
- Open access
- Export citation
Target-site and non–target site mechanisms of pronamide resistance in annual bluegrass (Poa annua) populations from Mississippi golf courses
-
- Journal:
- Weed Science / Volume 71 / Issue 3 / May 2023
- Published online by Cambridge University Press:
- 28 April 2023, pp. 206-216
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The impact of maternal SARS-COV-2 infection in early stages of newborn neurodevelopment: preliminary results in a multicenter Spanish study
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S103
-
- Article
-
- You have access
- Open access
- Export citation
Children and adolescents exposed to maltreatment already exhibit epigenetic patterns suggestive of heightened low-grade inflammation
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S71
-
- Article
-
- You have access
- Open access
- Export citation
Childhood and recent maternal adverse experiences and mother-infant attachment influence early newborns’ neurobehavioural profiles
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S144
-
- Article
-
- You have access
- Open access
- Export citation
Adsorption of cetyltrimethyl ammonium bromide surfactant for organophilization of palygorskite clay
-
- Journal:
- Clay Minerals / Volume 56 / Issue 2 / June 2021
- Published online by Cambridge University Press:
- 07 September 2021, pp. 140-147
-
- Article
- Export citation
An fMRI study of cognitive reappraisal in major depressive disorder and borderline personality disorder
-
- Journal:
- European Psychiatry / Volume 64 / Issue 1 / 2021
- Published online by Cambridge University Press:
- 01 September 2021, e56
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Multiple burdens of malnutrition and relative remoteness in rural Ecuadorian communities
-
- Journal:
- Public Health Nutrition / Volume 24 / Issue 14 / October 2021
- Published online by Cambridge University Press:
- 06 November 2020, pp. 4591-4602
-
- Article
-
- You have access
- HTML
- Export citation
Structural brain abnormalities in schizophrenia in adverse environments: examining the effect of poverty and violence in six Latin American cities
-
- Journal:
- The British Journal of Psychiatry / Volume 218 / Issue 2 / February 2021
- Published online by Cambridge University Press:
- 18 August 2020, pp. 112-118
- Print publication:
- February 2021
-
- Article
-
- You have access
- HTML
- Export citation
A prospective investigation of dietary prebiotic intake and colorectal cancer risk in the EPIC-Oxford cohort
-
- Journal:
- Proceedings of the Nutrition Society / Volume 79 / Issue OCE2 / 2020
- Published online by Cambridge University Press:
- 10 June 2020, E612
-
- Article
-
- You have access
- Export citation
Maternal BMI at the time of birth and selected risk factors associated with severe neonatal outcomes: a secondary analysis of the WHO Better Outcomes in Labour Difficulty (BOLD) project
-
- Journal:
- British Journal of Nutrition / Volume 124 / Issue 10 / 28 November 2020
- Published online by Cambridge University Press:
- 09 June 2020, pp. 1086-1092
- Print publication:
- 28 November 2020
-
- Article
-
- You have access
- HTML
- Export citation
2091 – Brain Activation In Patients With Schizophrenia During Psychological Stress
-
- Journal:
- European Psychiatry / Volume 28 / Issue S1 / 2013
- Published online by Cambridge University Press:
- 15 April 2020, 28-E1281
-
- Article
-
- You have access
- Export citation
EPA-1458 – Impulsivity and Adolescence : Evolution and Treatment of a Teenager with an Eating Disorder and Comorbidity with Attention Deficit Disorder with Hyperactivity, in the Context of a Dysfunctional Family
-
- Journal:
- European Psychiatry / Volume 29 / Issue S1 / 2014
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
Functional Profile People with Intellectual Disability in Aging Process of Specialized Service in the City of São Paulo - SP, Brazil.
-
- Journal:
- European Psychiatry / Volume 30 / Issue S1 / March 2015
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
Multidisciplinary Expertise in Consulting Program for People with Eating Disorders Hospitalized in PisiquiÁtrica Ward Behaviour Food
-
- Journal:
- European Psychiatry / Volume 30 / Issue S1 / March 2015
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation