259 results
Evidence of transmission of New Delhi metallo-β-lactamase-producing Klebsiella pneumoniae through a gastrointestinal endoscope without an elevator channel
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 02 April 2024, pp. 1-6
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Efficacy and safety of a 4-week course of repeated subcutaneous ketamine injections for treatment-resistant depression (KADS study): randomised double-blind active-controlled trial
-
- Journal:
- The British Journal of Psychiatry / Volume 223 / Issue 6 / December 2023
- Published online by Cambridge University Press:
- 14 July 2023, pp. 533-541
- Print publication:
- December 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Epidemiology of resistant gram-negative bacteria in nursing homes
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 9 / September 2023
- Published online by Cambridge University Press:
- 14 March 2023, pp. 1423-1428
- Print publication:
- September 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
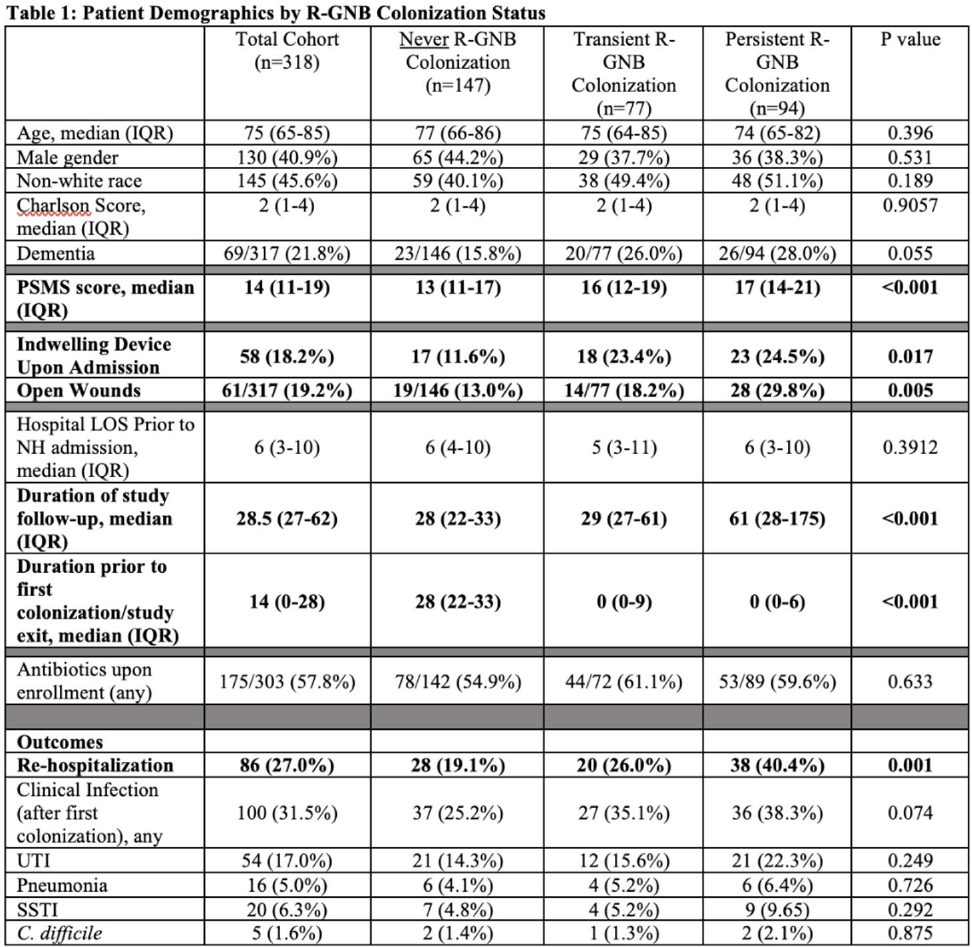
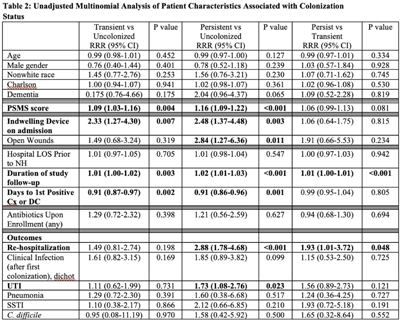
Low function and frequent readmission in nursing home patients with persistent resistant gram-negative bacterial colonization
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, pp. s53-s54
-
- Article
-
- You have access
- Open access
- Export citation
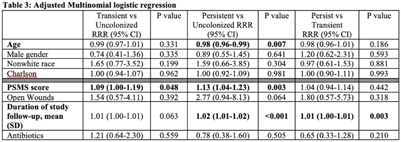
Comparison of fidaxomicin to oral vancomycin for the treatment of Clostridioides difficile infection in hospitalized patients
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, pp. s72-s73
-
- Article
-
- You have access
- Open access
- Export citation
8 - Response to Russell Foster
-
-
- Book:
- The Limits of EUrope
- Published by:
- Bristol University Press
- Published online:
- 13 October 2022
- Print publication:
- 05 April 2022, pp 91-94
-
- Chapter
- Export citation
Optimizing chloroacetamide application timing in dicamba-resistant cotton production systems for control of glyphosate-resistant Palmer amaranth (Amaranthus palmeri)
-
- Journal:
- Weed Technology / Volume 35 / Issue 6 / December 2021
- Published online by Cambridge University Press:
- 09 September 2021, pp. 1007-1013
-
- Article
- Export citation
Multidrug-resistant organism (MDRO) contamination of privacy curtains in nursing homes
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 43 / Issue 5 / May 2022
- Published online by Cambridge University Press:
- 31 May 2021, pp. 666-668
- Print publication:
- May 2022
-
- Article
-
- You have access
- HTML
- Export citation
Native tungsten from the Bol'shaya Pol'ya river valley and Mt Neroyka, Russia
- Part of
-
- Journal:
- Mineralogical Magazine / Volume 85 / Issue 1 / February 2021
- Published online by Cambridge University Press:
- 26 January 2021, pp. 76-81
-
- Article
- Export citation
Preparing nursing homes for a second wave of coronavirus disease 2019 (COVID-19)
- Part of
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 42 / Issue 10 / October 2021
- Published online by Cambridge University Press:
- 20 October 2020, pp. 1251-1254
- Print publication:
- October 2021
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
CHG Skin Application in Non-ICU Patients with Central Venous Catheters: Impact on CLABSI, MRSA Bacteremia, and LabID Rates
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 41 / Issue S1 / October 2020
- Published online by Cambridge University Press:
- 02 November 2020, pp. s164-s165
- Print publication:
- October 2020
-
- Article
-
- You have access
- Export citation
Profile of Nursing Homes Enrolled in the National Health Safety Network: Focus on Interfacility Communication
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 41 / Issue S1 / October 2020
- Published online by Cambridge University Press:
- 02 November 2020, pp. s523-s524
- Print publication:
- October 2020
-
- Article
-
- You have access
- Export citation
Incorporating preauthorization into antimicrobial stewardship pharmacist workflow reduces Clostridioides difficile and gastrointestinal panel testing
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 41 / Issue 10 / October 2020
- Published online by Cambridge University Press:
- 03 June 2020, pp. 1136-1141
- Print publication:
- October 2020
-
- Article
- Export citation
Psychotic experiences, psychiatric comorbidity and mental health need in the general population: a cross-sectional and cohort study in Southeast London
-
- Journal:
- Psychological Medicine / Volume 51 / Issue 1 / January 2021
- Published online by Cambridge University Press:
- 12 November 2019, pp. 147-157
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The devil is in the details: Factors influencing hand hygiene adherence and contamination with antibiotic-resistant organisms among healthcare providers in nursing facilities
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 40 / Issue 12 / December 2019
- Published online by Cambridge University Press:
- 24 October 2019, pp. 1394-1399
- Print publication:
- December 2019
-
- Article
- Export citation
Testing and application of a model for snow redistribution (Snow_Blow) in the Ellsworth Mountains, Antarctica
-
- Journal:
- Journal of Glaciology / Volume 65 / Issue 254 / December 2019
- Published online by Cambridge University Press:
- 07 October 2019, pp. 957-970
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The discreditation of oboyerite and a note on the crystal structure of plumbotellurite
-
- Journal:
- Mineralogical Magazine / Volume 83 / Issue 6 / December 2019
- Published online by Cambridge University Press:
- 04 October 2019, pp. 791-797
-
- Article
- Export citation
Hope in Dirt: Report of the Fort Apache Workshop on Forensic Sedimentology Applications to Cultural Property Crime, 15—19 October 2018
-
- Journal:
- International Journal of Cultural Property / Volume 26 / Issue 2 / May 2019
- Published online by Cambridge University Press:
- 20 August 2019, pp. 197-210
-
- Article
- Export citation
Identification of four patients with colistin-resistant Escherichia coli containing the mobile colistin resistance mcr-1 gene from a single health system in Michigan
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 40 / Issue 9 / September 2019
- Published online by Cambridge University Press:
- 10 July 2019, pp. 1059-1062
- Print publication:
- September 2019
-
- Article
- Export citation
The effect of cotton growth stage on response to a sublethal concentration of 2,4-D
-
- Journal:
- Weed Technology / Volume 33 / Issue 2 / April 2019
- Published online by Cambridge University Press:
- 14 May 2019, pp. 321-328
-
- Article
- Export citation