A 52-year-old man with known Waldenstrom macroglobulinemia (WM) presented with acute psychosis and hallucinations. His neurologic examination was intact aside from abnormal mental status. He was initially admitted to psychiatry department for management of psychosis and hallucinations. Neurology was consulted to rule out organic cause of his persistent psychosis.
MRI showed extensive leptomeningeal enhancement of the entire brain, spinal cord and cauda equina (Figure 1). In addition, enhancing longitudinally extensive intramedullary T2 hyperintensity in the thoracic cord was noted (Figure 2). CSF showed markedly elevated protein (6.5 g/L) and lymphocytic pleocytosis, and flow cytometry was positive for central nervous system (CNS) lymphoplasmacytic lymphoma consistent with Bing-Neel syndrome.
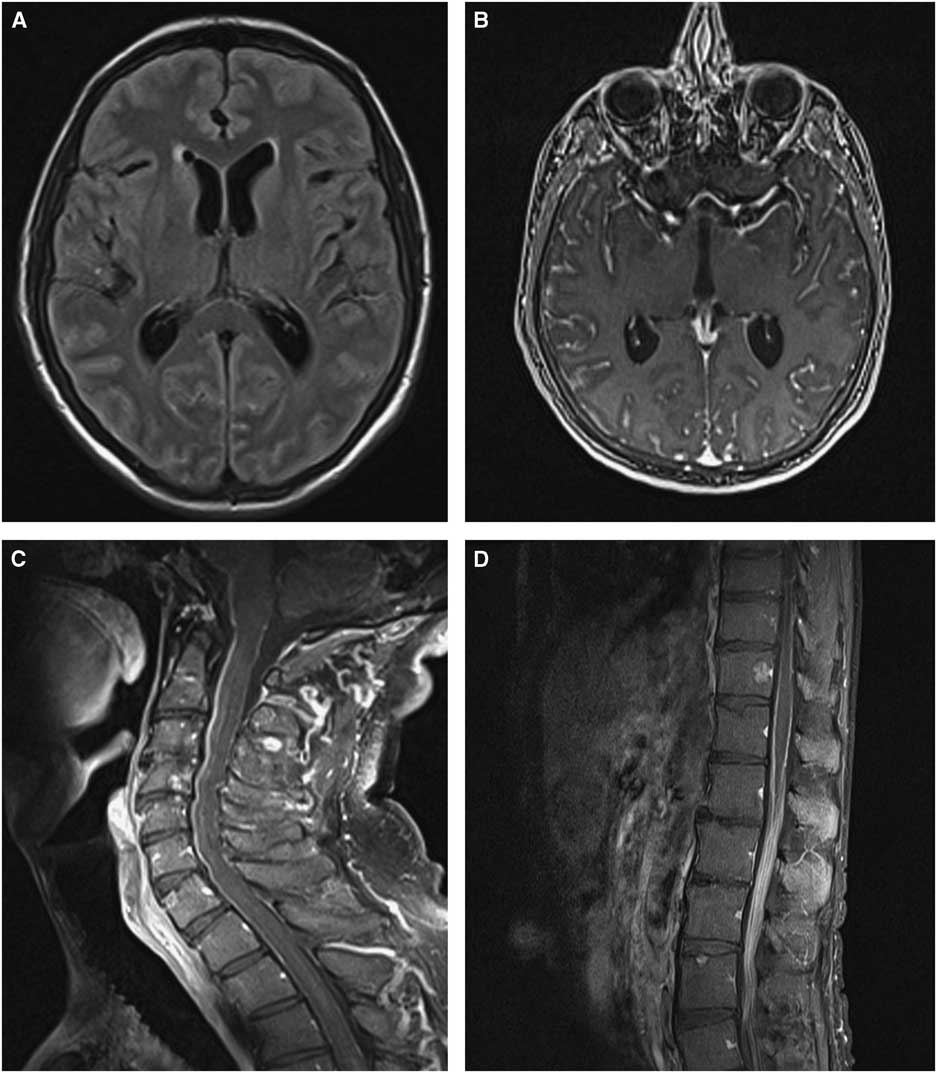
Figure 1 (A) Diffuse sulcal hyperintensities on FLAIR. (B) After gadolinium administration, there is extensive leptomeningeal enhancement in the brain, (C) cervical spine and (D) cauda equina.

Figure 2 (A, C) MRI of the spine showing longitudinally extensive intramedullary hyperintensity on T2. (B, D) This lesion enhances with gadolinium.
Bing-Neel syndrome is a rare presentation of WM. Waldenstrom macroglobulinemia is a rare B-cell-mediated immunoglobulin M-producing lymphoproliferative disorder accounting for 1-2% of non-Hodgkin’s lymphoma.Reference Castillo, D’Sa and Lunn 1 Bing-Neel syndrome is caused by infiltration of malignant B cells into the CNS, sometimes in the absence of systemic progression.Reference Minnema, Kimby and D’Sa 2 Patients present with progressive symptoms over weeks or months, including headache, seizures, cognitive changes or cranial neuropathies from leptomeningeal involvement.Reference Minnema, Kimby and D’Sa 2 They can also present with hyperviscosity syndrome leading to visual loss (retinal hemorrhage) or epistaxis. Treatment is similar to primary CNS lymphoma, with steroid therapy as induction, followed by blood–brain barrier penetrating chemotherapy (e.g., methotrexate, cytarabine and ibrutinib).Reference Minnema, Kimby and D’Sa 2 Median survival for WM is estimated to be 7-12 years.Reference Minnema, Kimby and D’Sa 2 The survival rate for Bing-Neel syndrome is reported as 71% at 5 years and 59% at 10 years.Reference Simon, Fitsiori and Lemal 3
Clinicians should remember that malignant B-cell infiltration to the CNS may lead to isolated psychiatric symptoms and should have low threshold for work-up of new psychosis or hallucinations in WM patients. In addition to leptomeningeal and intraparenchymal brain lesions, intramedullary spinal lesions may also be seen in Bing-Neel syndrome.
Acknowledgments
None.
Disclosures
JZD, RG and SC have nothing to disclose.
Statement of Authorship
JZD contributed to clinical care of the patient, case concept and drafting and revising the manuscript. RG was involved in drafting and revising the manuscript. SC was involved in imaging acquisition and drafting and revising the manuscript.






