Chronic non-communicable diseases, including CVD, cancer and diabetes mellitus, are the leading cause of morbidity and mortality worldwide(1–3). Obesity, defined by the WHO as excessive fat accumulation, is an important risk factor for these diseases(4). The number of overweight adolescents is increasing worldwide, and according to the WHO, more than one in six adolescents worldwide were overweight in 2016(5).
The BMI is a simple index, which considers weight and height, commonly used to classify overweight and obesity(4). Although it is widely used as a measure that characterises obesity, BMI does not provide information about the amount of body fat, as it does not differentiate lean tissue from adipose(6). In this context, a specific phenotype of obesity was defined: normal-weight obesity (NWO)(Reference Lorenzo, Martinoli and Vaia7), which is used to classify individuals with BMI considered healthy, but with excess body fat(Reference Lorenzo, Martinoli and Vaia7).
Most studies conducted with NWO are with adults, and the presence of the phenotype is associated with a low-grade pro-inflammatory state, insulin resistance, dyslipidemia and increased risk of CVD(Reference Lorenzo, Martinoli and Vaia7–Reference Kapoor, Lotfaliany and Sathish13). In adolescents, a recent systematic review conducted by our research group(Reference Cota, Suhett and Leite14) points out that, as for adults, NWO is associated with the presence of cardiometabolic risk factors, such as increased waist circumference, dyslipidemia and unfavourable glycid profile.
Although information is available on the potential of NWO to impact cardiometabolic health in adolescence, few studies have examined the factors associated with NWO occurrence, especially in early life(Reference Cota, Suhett and Leite14). Thus, evidence on how sociodemographic and behavioural characteristics, including food consumption, are associated with this phenotype is scarce(Reference Cota, Suhett and Leite14). The identification of the factors associated with NWO in adolescents is necessary, since it will provide evidence for the implementation of preventive strategies. This is particularly important when considering that NWO in this age group is often neglected, because they present normal weight and young age. Therefore, it is intended to help fill the existing gap on the subject with this study that aims to investigate the sociodemographic factors, family history of chronic non-communicable diseases, body perception, lifestyle and food consumption associated with NWO in adolescents.
Materials and methods
This study is an integral part of the ‘Comparative study between the three phases of adolescence, in relation to excess body fat and cardiovascular risk factors for metabolic syndrome’, already detailed in other publications(Reference Pereira15,Reference Faria16) . All stages of data collection were carried out at the Health Division of the Federal University of Viçosa, by three previously trained nutritionists. The adolescents were instructed to attend the data collection steps accompanied by their parents/guardians.
Population, design and sampling
A cross-sectional, population-based epidemiological study was conducted with adolescents aged 10–19 years, of both sexes, selected from the rural and urban, public and private school population of the municipality of Viçosa, state of Minas Gerais (MG), Brazil, between the years 2010 and 2013. The sample size was calculated using the StatCalc, Epi Info software, version 6.04, from a specific formula for cross-sectional studies, considering the total population of 11 898 adolescents in the municipality of Viçosa/MG(17), expected prevalence of 50·0 %(Reference Luiz, Magnanini, Medronho, Carvalho and Block18), acceptable variability of 5 % and 95 % confidence level, totalling a minimum sample of 372 adolescents. When 20 % was added to this for possible losses and control of confounding factors, a minimum total of 447 was required. The adolescents were selected by simple random sampling, using a random device to draw the participants. A total of 506 adolescents with adequate nutritional status (normal weight) according to BMI/age(19) were included in this study.
The inclusion criteria were: not making regular use of medications that alter blood glycemia, insulinemia, lipid metabolism and/or blood pressure levels, not participating in weight reduction and control programme, not making regular use of diuretics/laxatives, not being pregnant or have already been pregnant, not having deformities in the neck, not having been diagnosed with infections, acute inflammations and thyroid diseases.
All participants and their parents/guardians, in the case of volunteers under the age of 18 years, signed the Informed Consent Form, according to the Helsinki Declaration. The study was approved by the Ethics Committee in Human Research of the Federal University of Viçosa (Of. Ref. No. 0140/2010).
At the end of the study, all participants were informed about the results of anthropometric, body composition, nutritional and clinical evaluations and were oriented about healthy eating. In addition, the volunteers who presented altered nutritional status, as well as those who were interested, received individualised nutritional care according to their needs and at no cost.
Socio-economic and demographic aspects
A questionnaire was applied to assess the profile of adolescents, such as age and sex. In addition, the socio-economic condition was investigated through the application of a questionnaire that collects a diversity of social and economic themes at the household level, using the same methodology adopted by the Pesquisa sobre Padrões de Vida (PPV) – Research on Living Standards(20), which was classified as ‘adequate’ or ‘precarious and intermediate’.
Family history of diseases
Adolescents were asked (accompanied by parents/guardians) about the family history of diseases, based on information regarding family background – parents, siblings, maternal and paternal uncles and grandparents – who have some chronic non-communicable disease or who had died due to some chronic non-communicable disease: obesity, dyslipidemia, arterial hypertension, diabetes and CVD. When at least one of the family members had any of these diseases, a positive family history for the respective disease was considered.
Body perception
Adolescents were asked about self-perception of body image through a question. They had to answer whether they were satisfied with their body or not.
Physical activity
The level of physical activity was evaluated using the International Physical Activity Questionnaire (IPAQ), short version, validated for this population group(Reference Guedes, Lopes and Guedes21). The questionnaire consists of seven items that assess the number of days the participant practices vigorous, moderate activities or walking; and the time allocated to these activities. In addition, the questionnaire investigates the time spent sitting at home, in front of the TV, video game, cell phone or other electronic equipment, at school or at work. Sitting time is assessed both on weekdays and on weekends. Based on this information, adolescents are classified as sedentary, irregularly active, active and very active(22). We chose to group sedentary and irregularly active individuals into insufficiently active; and those considered active and very active were grouped into physically active.
Food consumption
The dietary analysis was performed through the application of the qualitative FFQ in order to know the frequency of consumption of food groups. The FFQ was applied individually, and adolescents were instructed to report on the frequency of food consumption in the month prior to the date of application of the questionnaire(Reference Serra-Majem, Aracenta-Bartrina, Serra-Majem, Aracenta-Bartrina and Mataix-Verdú23). The list of foods that made up the FFQ was determined considering the foods that are part of the eating habits of adolescents in the municipality of Viçosa, based on data regarding the application of 24-h Recall in adolescents assisted by the Programa de Atenção à Saúde do Adolescente (PROASA) – Adolescent Health Care Program – of Federal University of Viçosa. The FFQ was tested before collection with other adolescents from Viçosa, reproducing the same methodology of this study, in a pilot study. This procedure was performed in order to verify whether the list of foods in the FFQ was adequate for the study group. In this test, foods that were not included were observed, and these were added to the FFQ. Finally, the FFQ in this study consisted of 106 items, divided into 9 food groups (Table 1 – Supplementary Material). For each food item, the participant could answer, in relation to the frequency of weekly consumption, the options: < 1 d; 1 d; 2 d; 3 d; 4 d; 5 d; 6 d; 7 d; or never. Information regarding food items was grouped and analysed according to the nine food groups: cereals (such as rice, bread, cakes, potatoes and noodles); vegetables (such as lettuce, tomatoes, cauliflower and onions); fruits (such as bananas, apples, papaya and avocado); legumes (such as beans and lentils); meats, sausages and eggs (such as beef and pork, fish, ham, sausages and eggs); milk and derivatives (including cheese, curd and yogurt); sugars and sweets (such as chocolate, ice cream and soft drinks); oils and fats (as margarine, butter and oil for the preparation of fried foods); industrialised condiments (such as mustard, ketchup, meat broths and other industrialised ready-made seasonings). The frequency of weekly consumption was categorised as < 4 or ≥ 4 times per week(Reference Olafsdottir, Torfadottir and Arngrimsson24), and the frequency ≥ 4 was referred to as regular consumption.
Table 1. Characterisation of adolescents in total sample and according to the sex

FH, family history.
The results were expressed as absolute and (relative) frequency for categorical variables. Quantitative variables were expressed as mean and (standard deviation) when analysed by Student’s t test or as median and (interquartile range) when analysed by Mann–Whitney test.
* Student’s t test.
† Pearson’s χ 2.
In addition, through a questionnaire, the volunteers were asked about their eating habits, including the use of sweeteners (sugar substitutes) (yes or not) and the consumption of breakfast (yes or not) and substitute snack for dinner (yes or not). We also investigated the number of daily meals, habit of alcohol consumption (yes or not) and whether the participants have ever tried cigarettes (due to the low prevalence of smokers in our sample (n 4), we considered both smokers and those who had tried cigarettes).
Anthropometry and body fat assessment
The participants were barefoot, wearing light clothing, without metallic ornaments and fasting for 12 h, for the anthropometric and body composition analysis.
Weight and height were measured using standardised international techniques(Reference Lohman, Roche and Martorell25), using electronic digital scale (LC 200pp, Marte®, São Paulo, Brazil) and portable stadiometer (Alturexata®, Belo Horizonte, Brazil). Height was measured twice, by two different nutritionists, and a maximum variation of 0·5 cm was admitted between the two measurements, using the mean as the final result. If the measurement exceeded the variation of 0·5 cm, the measurement was repeated.
For total body fat analysis, the equipment dual-energy X-ray absorptiometry (Lunar Prodigy Advance DXA System – analysis version: 13.31, GE Healthcare, Madison, WI, USA) was used. The evaluation was performed with each individual in dorsal decubitus, through a series of transverse scans from head to feet, with a duration of full body screening of approximately 10 min.
Definition of normal-weight obesity
NWO is defined by the presence of normal weight, but excess body fat(Reference Lorenzo, Martinoli and Vaia7). To evaluate the nutritional status of adolescents and classify them as normal weight, BMI was used, obtained by dividing the weight by the square of height, analysed according to sex and age, in agreement to the WHO(19). Those with Z-score values between ≥ –2SD and < +1SD were classified as normal weight(19).
Body composition analysis was performed by dual-energy X-ray absorptiometry and to classify the body fat percentage, values equal to or greater than 25 % and 30 % in males and females sex, respectively, were considered high(Reference Williams, Going and Lohman26).
Thus, the 506 adolescents with normal BMI/age in this study were divided into two groups:
(a) With NWO: represents adolescents with normal weight, according to BMI/age(19), and with excess body fat (body fat values equal to or greater than 25 % and 30 % in males and females, respectively(Reference Williams, Going and Lohman26)).
(b) Without NWO: represents adolescents with normal weight, according to BMI/age(19), and without excess body fat (body fat values < 25 % and < 30 % in males and females, respectively(Reference Williams, Going and Lohman26)).
Statistical analysis
The database was prepared with double typing, in Microsoft Office Excel 2007. Statistical analysis was performed using STATA software, version 14. The consistency and distribution of quantitative variables were evaluated by histograms, asymmetry coefficient and kurtosis, as well as by Shapiro–Wilk normality test. According to the normality and homogeneity of the variances, quantitative variables were analysed by Student’s t test or Mann–Whitney test. Statistical differences in categorical variables were analysed by Pearson’s χ 2 test or Fisher’s exact test. Categorical variables were expressed as absolute and (relative) frequency, and quantitative variables as mean and standard deviation or median and interquartile range.
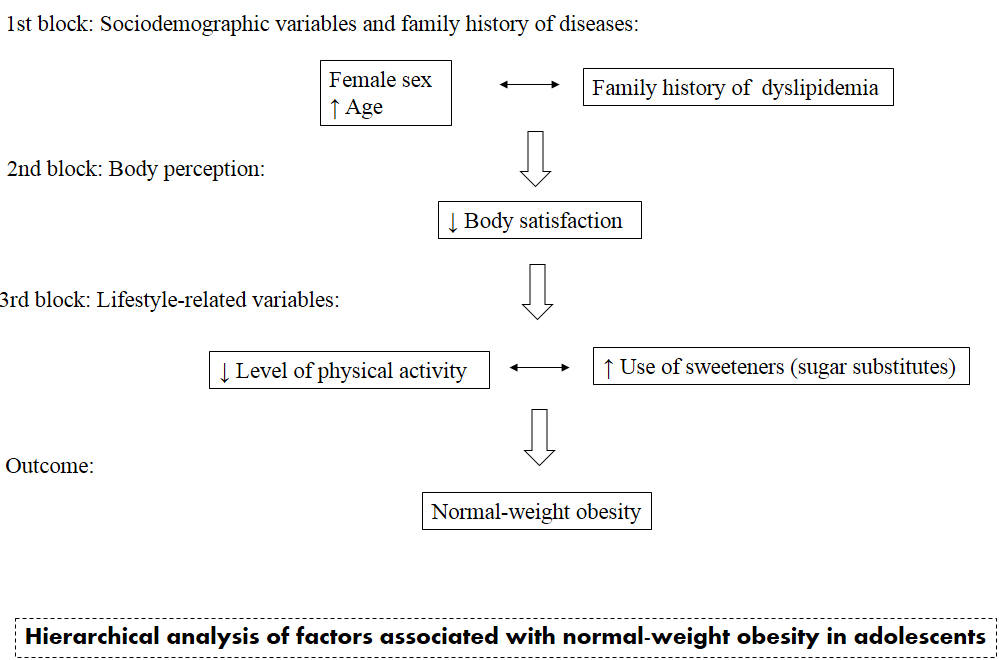
To evaluate the factors associated with NWO, a hierarchical approach was used,(Reference Victora, Huttly and Fuchs27) based on a theoretical model on the relationships between the variables studied, which were grouped into four blocks. In the first, sociodemographic characteristics were included: sex, age and socio-economic status, as well as family history of diseases. In the second block, body satisfaction and, in the third block, variables related to lifestyle. In the fourth block, the food consumption variables assessed by the FFQ were inserted (Fig. 1 – Supplementary Material).
From the established theoretical model, simple and multiple binary logistic regression models were estimated. For the multiple analysis, in each block, an internal analysis was performed. This intra-block analysis consisted in the estimation of a logistic regression model considering NWO as an outcome variable and the other variables of the block as explanatory. All the variables of a block were used as adjustments in the following blocks and, thus, began to compose the group of variables of the next block. This procedure was repeated until the final block (block 4). The Hosmer–Lemeshow test was used to evaluate the quality of the models in each block. The association measure used was the OR with CI of 95 %. The significance level adopted in all analyses was 5 %.
Results
Among the 506 adolescents with normal weight by BMI/age, 54·5 % were female and the median age was equal to 14·2 (interquartile range = 3·02) years. It was observed that 93·9 % of adolescents had a family member with one or more chronic diseases (obesity, diabetes, dyslipidemia, hypertension or CVD). In addition, unhealthy habits such as alcohol intake (27·5 %), have tried cigarettes at least once in life (10·3 %), not having breakfast (27·5 %) and insufficient levels of physical activity (26·5 %) were observed in a considerable proportion of adolescents (Table 1). Analysis of the population stratified by sex indicated that girls had a higher frequency of family members with diabetes (female: 56·1 % v. male: 46·9 %; P < 0·05) and were more dissatisfied with their own body (female: 56·9 % v. male: 33·9 %; P < 0·05). A higher percentage of girls did not eat breakfast (female: 32·6 % v. male: 21·3 %; P < 0·05) and replaced dinner with snacks (female: 28·6 % v. male: 16·5 %; P < 0·05) was also observed. On the other hand, regular consumption of vegetables (female: 73·6 % v. male: 64·3 %; P < 0·05) was higher among female participants. Consumption of legumes (female: 86·6 % v. male: 93·5 %; P < 0·05) was more frequent among males. A borderline significance was also observed for physical activity level, in which boys were more physically active (female: 69·9 % v. male: 77·8 %; P = 0·045) (Table 1).
The prevalence of NWO phenotype in the studied group was 13·8 % (n 70) (95 % CI = 10·8, 17·0). It is observed (Table 2) that the frequency of female adolescents among those with NWO is 82·9 %, while 50·0 % of adolescents who do not have NWO are female (P < 0·05). In addition, adolescents with NWO are older (with NWO: 15·93 (4·48) years v. without NWO: 13·95 (6·06) years; P < 0·05), have a higher frequency of family members with dyslipidemia (with NWO: 68·6 % v. without NWO: 52·3 %; P < 0·05), are less satisfied with their body (with NWO: 22·9 % v. without NWO: 58·5 %; P < 0·05) and are more physically inactive (with NWO: 37·1 % v. without NWO: 24·8 %; P < 0·05). Adolescents with NWO were also observed to consume fewer meals per d (with NWO: 4·17 (0·96) meals v. without NWO: 4·45 (0·97) meals; P < 0·05), use more sweeteners (with NWO: 17·1 % v. without NWO: 9·2 %; P < 0·05) and have a higher frequency of having tried cigarettes (with NWO: 24·3 % v. without NWO: 7·3 %; P < 0·05) (Table 2).
Table 2. Characterisation of adolescents according to the absence or presence of normal-weight obesity (NWO)

NWO, normal-weight obesity; FH, family history.
The results were expressed as absolute and (relative) frequency for categorical variables. Quantitative variables were expressed as mean and standard deviation when analysed by Student’s t test or as median and interquartile range when analysed by Mann–Whitney test.
* Pearson’s χ 2.
† Mann–Whitney.
‡ Student’s t test.
§ Fisher’s exact test.
In the logistic regression analyses, in the crude model (Table 3) it is observed that with each increase in the consumption of one meal per d, the odds of having NWO reduces by 25 % (OR = 0·75; 95 % CI 0·58, 0·97). However, after adjustments for lifestyle variables, family history of disease, and sociodemographic variables, this association disappeared. Similar to the number of meals per d, it is noted, in the crude model, that the odds of having NWO among adolescents who have ever tried cigarettes is 2·05 times the odds compared with those who have never tried (OR = 2·05; 95 % CI 1·02, 4·13) (Table 3). Moreover, in the crude model, the phenotype was associated with sex, age, family history of dyslipidemia, body satisfaction, level of physical activity and use of sweeteners, which maintained significant associations in the analysis of factors associated with the phenotype (adjusted model) (Table 3).
Table 3. Crude and adjusted OR (or) and 95 % CI for factors associated with normal-weight obesity (n 506)

* Statistical significance.
† This model represents the analysis of the factors associated with the NWO phenotype using a hierarchical approach. First block: adjustment made for the variables of this block; second block: adjustment made for the variables of this block and for the variables of the previous blocks (first block); third block: adjustment made for the variables of this block and for the variables of the previous blocks (first and second block); fourth block: adjustment made for the variables of this block and for the variables of the previous blocks (first, second and third block).
‡ The results express the odds of the phenotype in the male sex, compared with the female sex.
§ The results express the odds of the phenotype in adolescents with precarious or intermediate socio-economic condition, compared with the adequate one.
|| The results express the odds of the phenotype in physically active adolescents, compared with insufficiently active adolescents.
¶ Variables categorised as yes or no. The results express the consumption of breakfast and substitute snack for dinner, use of sweeteners, alcohol intake and those who have tried a cigarette (yes), in relation to those who do not consume breakfast and substitute snack for dinner, do not use sweeteners, do not consume alcohol and who have never tried a cigarette (no).
** The food groups were categorised as consumption ≥ 4 times per week and < 4 times per week. The results express regular consumption (≥ 4 times/week), compared with non-regular (< 4 times/week).
†† NA, not assessed, as all participants consume cereals ≥ 4 times a week.
In this sense, in the adjusted model, when investigating the factors associated with NWO phenotype (Table 3), it is noted that the odds of having NWO in male participants is 79 % lower (OR = 0·21; 95 % CI 0·11, 0·41) compared with female participants; and that the odds of the NWO phenotype is greater in adolescents with a positive family history of dyslipidemia (OR = 1·81; 95 % CI 1·01, 3·28). In addition, the 1-year increase in age is associated with a 14 % increase (OR = 1·14; 95 % CI 1·04, 1·26) in the odds of having NWO. In block 2, an inverse association was observed with body satisfaction, that is, the odds of having NWO among adolescents satisfied with their body was 70 % lower compared with those dissatisfied (OR = 0·30; 95 % CI 0·16, 0·56). At block 3, it was observed that the odds of having NWO in physically active individuals is 56 % lower compared with insufficiently active individuals (OR = 0·44; 95 % CI 0·24, 0·81). In addition, it was found that the odds of having NWO in adolescents who use sweeteners (sugar substitutes) is higher, compared with those who do not (OR = 3·84; 95 % CI 1·70, 8·65) (Table 3). The different factors associated with NWO are represented in Fig. 2 in the supplementary material.
Furthermore, as a secondary analysis, we investigated whether the factors associated with the NWO phenotype differed between sexes by means of a stratified analysis. For this, we used the same hierarchical approach as the adjusted model with the total sample. It was observed, for males, that the odds of the NWO phenotype is higher among adolescents with family history of dyslipidemia (OR = 4·76; 95 % CI 1·07, 20·94), who used sweeteners (OR = 16·33; 95 % CI 1·64, 62·38) and among those who had already tried cigarettes (OR = 14·12; 95 % CI 1·06, 88·70). In addition, an inverse association of the phenotype was observed with body satisfaction (OR = 0·19; 95 % CI 0·05, 0·75) and use of processed condiments (OR = 0·03; 95 % CI 0·01, 0·60). For female adolescents, it was observed a positive association of the NWO phenotype with age (OR = 1·23; 95 % CI 1·10, 1·37) and use of sweeteners (OR = 3·42; 95 % CI 1·32, 8·80), and an inverse association of the phenotype with body satisfaction (OR = 0·37; 95 % CI 0·18, 0·77) and practice of physical activity (OR = 0·48; 95 % CI 0·24, 0·96) (data not shown).
Discussion
The prevalence of NWO in adolescents is not uncommon and can vary from 6·8 % to 55·6 %(Reference Cota, Suhett and Leite14), depending on the population, age group and diagnostic criteria used. The presence of this phenotype is associated with increased cardiometabolic risk, which can persist until adulthood(Reference Cheng and Wiklund28,Reference Wiklund, Törmäkangas and Shi29) . Thus, understanding the factors associated with NWO becomes important for the development of prevention and control strategies. According to our knowledge, this is the first study that investigated, through hierarchical analysis, the factors associated with NWO in a representative sample of adolescents of both sexes. We observed a prevalence of NWO in 13·8 % among the participants and that the factors associated with the phenotype were sex, age, family history of dyslipidemia, body satisfaction, level of physical activity and use of sweeteners. Therefore, our study brings relevant contributions on the topic, especially considering that studies with adolescents with NWO are scarce.
In accordance with the findings of other studies(Reference Lorenzo, Martinoli and Vaia7,Reference Marques-Vidal, Pécoud and Hayoz9,Reference Kim, Han and Yang30) , there was a predominance of NWO in females. In addition, also in accordance with what we observed, there is a positive association of the phenotype with age(Reference Marques-Vidal, Chiolero and Paccaud31,Reference Zhang, Schumann and Huang32) , which can be explained because of the fact that body fat increases over the years(Reference Gallagher, Heymsfield and Heo33–Reference Leone, Battezzati and Bedogni36). We also found higher odds of having NWO in adolescents who had a family history of dyslipidemia. The family history of diseases, such as dyslipidemias, can help in the tracking of various cardiometabolic changes(Reference Wiegman, Rodenburg and de Jongh37,Reference Strufaldi, Souza and Puccini38) , since it is based on heredity, eating habits and shared lifestyle(39). In this way, the investigation of family history for chronic diseases can be useful in assessing the cardiometabolic risk of adolescents.
In addition, we found that the odds of having NWO was lower among those who are satisfied with their body, compared with those who are not satisfied. In a cross-sectional study with male adolescents, Fortes et al. (2015) observed that participants who were not satisfied with the body had a higher percentage of body fat than those who were satisfied(Reference Fortes, Ribeiro Junior and Paes40). In another study conducted with university students, it was observed that body adiposity, evaluated by the sum of the thickness of five skin folds, was associated with dissatisfaction with body image (OR = 2·56; 95 % CI 1·36, 4·80)(Reference Coqueiro, Petroski and Pelegrini41). Hence, our findings corroborate those of other authors, highlighting that body dissatisfaction may be associated with excess body fat, even among normal-weight individuals, as found in this study.
High body adiposity, regardless of BMI, is a factor associated with increased risk for CVD, cardiometabolic dysregulation, coronary artery disease and cardiovascular mortality(Reference Jia, Xu and Xing42). Cardiometabolic disorders are one of the leading causes of death worldwide(43,44) , and excess fat exerts an important influence for the evolution of these disorders. The conventionally described risk factors for excess body adiposity include unhealthy eating patterns and physical inactivity that are also partly responsible for the increase in obesity(45,46) . In this sense, it is valid to consider that several chronic diseases manifested in adulthood originate from modifiable lifestyle factors practiced in childhood and adolescence(45), and the adoption of good life habits is important for the prevention and control of these diseases.
In this sense, the results of other studies indicated an association of the NWO phenotype with modifiable lifestyle factors, such as low levels of physical activity in adolescents and adults(Reference Madeira, Silva and Veloso11,Reference Cota, Suhett and Leite14,Reference Männistö, Harald and Kontto47) . In line with these studies, we found lower odds of having NWO among adolescents who are physically active. Regular physical activity has been associated with several benefits, such as lowering cholesterol, blood pressure and obesity(48,Reference Morelli, Avolio and Galluccio49) . In addition, physical inactivity is an important risk factor for CVD(50) and the increase in the adoption of sedentary behaviours in adolescents, such as watching TV, playing video games and using the computer, is a cause for concern, since it has contributed to reduce the promotion of a physically active lifestyle(Reference Alves, Silva and Assis51). In this context, encouraging the practice of physical activity is of great importance, given the beneficial role that exercising plays in health, including in adolescence.
The adoption of practices aimed at weight reduction is common in adolescence, highlighting the use of sugar substitute products, such as sweeteners. In a cross-sectional study with 118 female normal-weight adolescents, the use of sweeteners was the factor most associated with excess adiposity in the established risk model(Reference Ribeiro Vieira, de Faria and de Faria52). In accordance with these findings, we observed in this study that adolescents with NWO consume more sweeteners than normal-weight individuals without excess body fat. Considering the cross-sectional design of this study, it is important to consider that this result can be explained by reverse causality. This is because the practice of using sweeteners among individuals with NWO, combined with the high frequency of body dissatisfaction also observed in this group, can be a way to reduce energy consumption in order to reduce weight and body fat. In addition, it should be highlighted the possibility of this restriction of energy consumption, through the use of sweeteners, be compensated by the increase in the intake of other foods, such as fast food, which could cause greater deposition of body fat(Reference Rosado and Monteiro53).
Different methods and instruments are used for dietary analysis, which is challenging, given the complexity of qualitatively and quantitatively assessing food intake(Reference Cavalcante, Priore and Franceschini54). In this study, we did not find any association of food consumption due to FFQ with NWO. The simplicity in the administration of FFQ and its cost-effectiveness are great advantages(Reference Ratelle, Skinner and Packull-McCormick55), in addition to the ease of coding and processing(Reference Henríquez-Sánchez, Sánchez-Villegas and Doreste-Alonso56). However, the performance of the FFQ in the accurate assessment of food intake varies between populations and environments. Differences can be due to a variety of reasons: the number and variety of food items used; ordering of questions; and whether the questionnaires were self-applicable or interview-guided(Reference Ortiz-Andrellucchi, Henríquez-Sánchez and Sánchez-Villegas57,Reference Cade, Burley and Warm58) . In addition, a FFQ can be non-quantitative, asking only the frequency of food consumed(Reference Sugianto, Chan and Wong59), which was the case of the one used in this study. It is also important to consider that in this study we did not adjust the models by total energy intake, as we did not obtain this information from the qualitative FFQ. This may justify, in part, the absence of association of food items evaluated by the qualitative FFQ with the NWO phenotype.
This research presented other limitations that deserve to be highlighted. A questionnaire was used by the interviewers, with a single question, to evaluate body self-perception, without using a validated method. In addition, the cross-sectional design makes it impossible to ensure the temporality of the observed associations between the factors and NWO, besides the possibility of the reverse causality bias already mentioned. Despite these limitations, this population-based study contributes to filling important gaps on the subject in the adolescent public and has as positive points the methodological robustness in data collection, use of validated methods, such as dual-energy X-ray absorptiometry, in addition to the large set of covariates that allowed a more thorough evaluation of the factors associated with the phenotype.
Conclusion
The odds of having NWO increases with age, is lower in male adolescents and is higher in those with family history of dyslipidemia. Adolescents satisfied with their body and physically active have lower odds of having NWO. In addition, those with NWO have higher odds of using sweeteners. Given this, the importance of adopting a healthy lifestyle in adolescence to minimise the present and future health risks related to excess fat observed in those with NWO is emphasised.
Furthermore, it is highlighted that further studies are needed to investigate the eating habits of individuals with NWO, as well as longitudinal studies that can establish causal relationships between this phenotype and its risk factors.
Acknowledgements
The authors thank all adolescents who participated in this study and their parents/guardians and the Coordination for the Improvement of Higher Education Personnel (CAPES, Brazil, funding code 001) for the scholarship granted to B. C. C.
This study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (grant number 485986/2011-6) and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) (grant number APQ-01618-10). The CNPq and FAPEMIG had no role in the design, analysis or writing of this article.
B. C. C. was responsible for the analysis and interpretation of the data, conducted the literature search, as well as wrote the manuscript. F. R. C. participated in the analysis and interpretation of data and writing of the article. L. L. J. and S. A. V. R. participated in the analysis and interpretation of data, as well as the critical review of the paper. S. E. P. acted in the conception and design of the study, as well as the critical review of the paper. P. F. F. participated in the conception of the study design, data collection and writing of the article. E. R. F. and F. R. F. participated in the conception of the study design, data collection, as well as the critical review of the paper. All authors have read and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114522000307