102 results
Implementing a continuous quality-improvement framework for tuberculosis infection prevention and control in healthcare facilities in China, 2017–2019
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 5 / May 2024
- Published online by Cambridge University Press:
- 25 January 2024, pp. 651-657
- Print publication:
- May 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Northward migration of Red Knots Calidris canutus rufa and environment connectivity of southern Brazil to Canada
-
- Journal:
- Bird Conservation International / Volume 34 / 2024
- Published online by Cambridge University Press:
- 16 January 2024, e2
-
- Article
- Export citation
Severe and common mental disorders and risk of emergency hospital admissions for ambulatory care sensitive conditions among the UK Biobank cohort
-
- Journal:
- BJPsych Open / Volume 9 / Issue 6 / November 2023
- Published online by Cambridge University Press:
- 07 November 2023, e211
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Radiofrequency ice dielectric measurements at Summit Station, Greenland
-
- Journal:
- Journal of Glaciology , First View
- Published online by Cambridge University Press:
- 09 October 2023, pp. 1-12
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
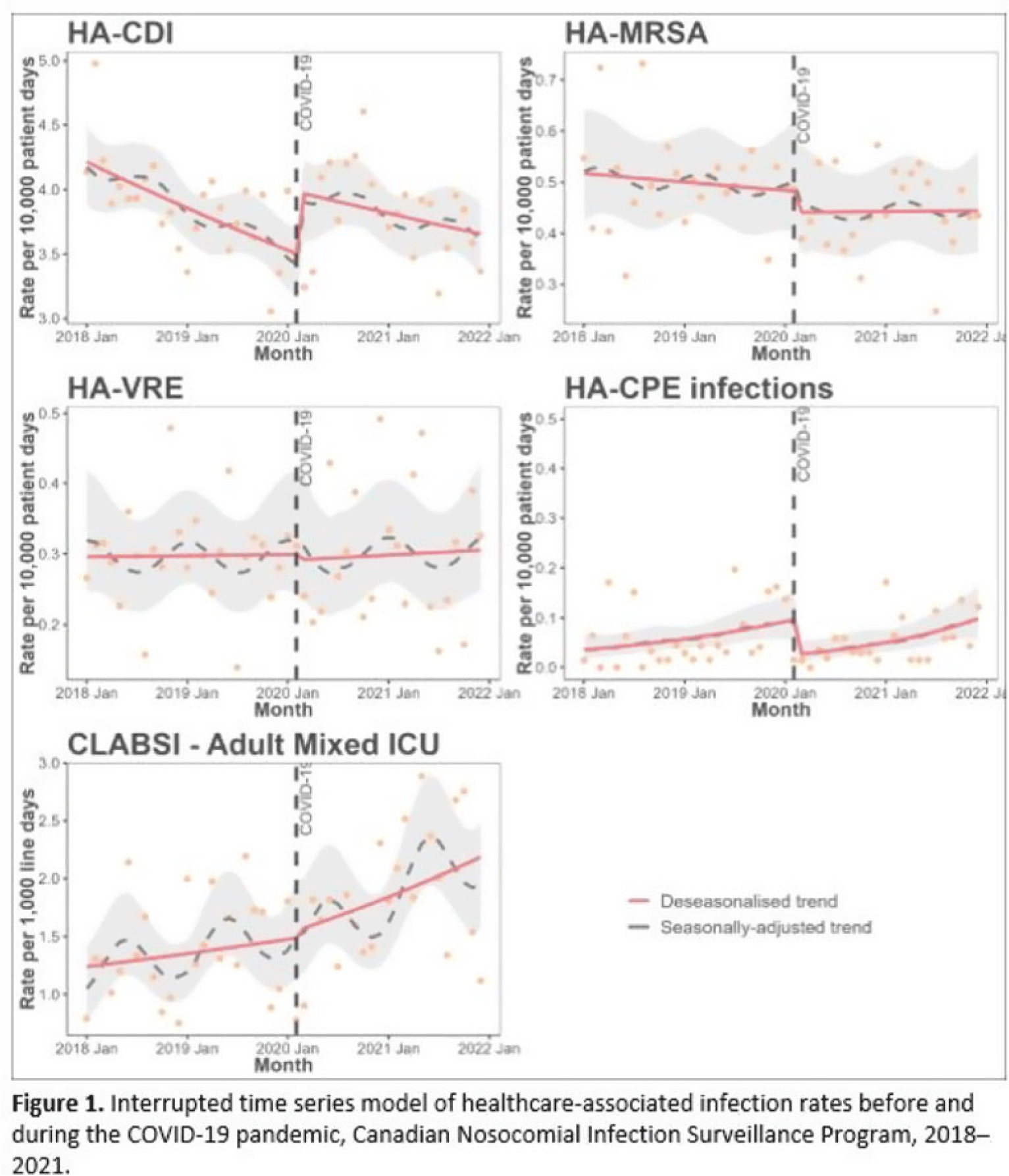
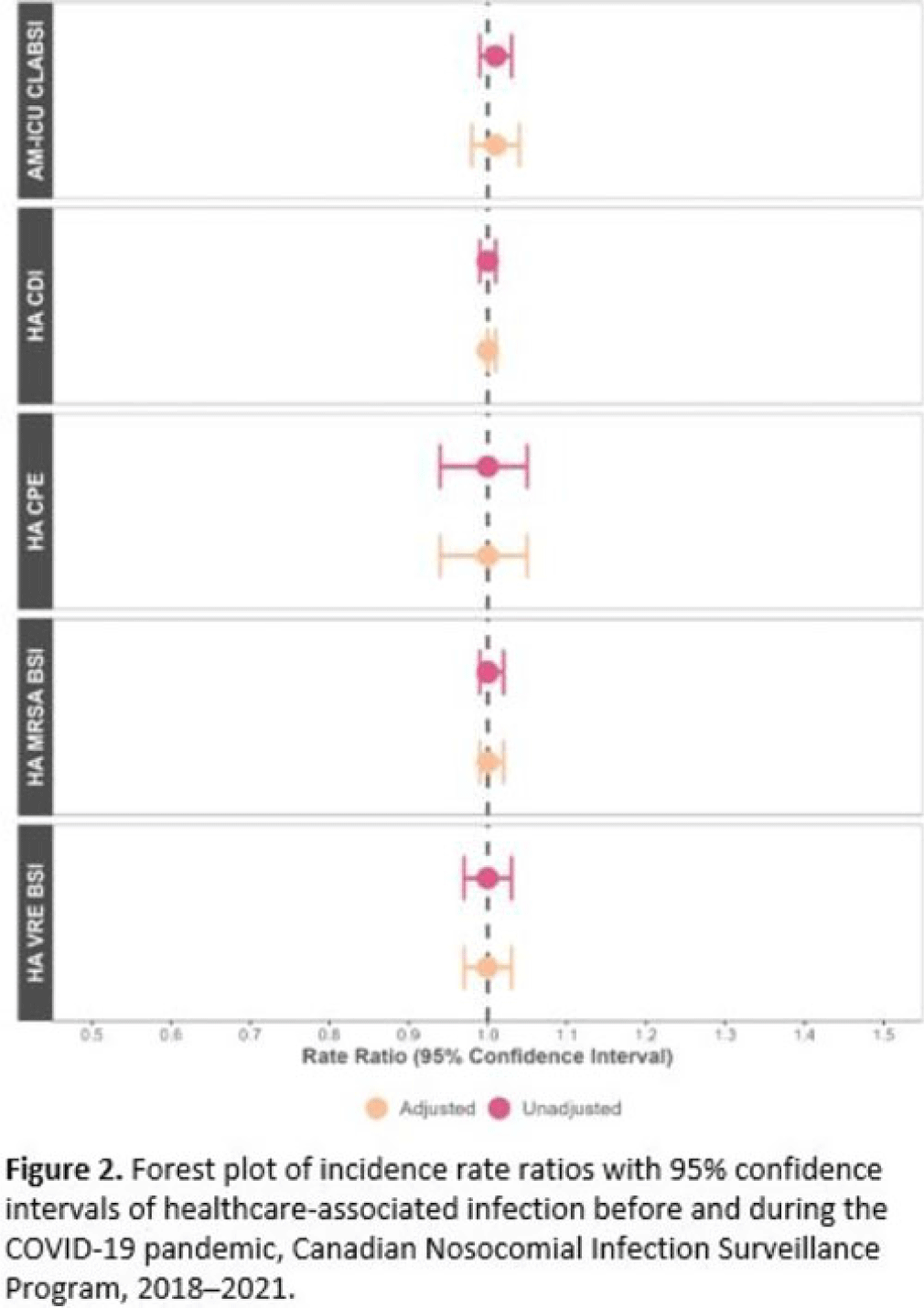
Impact of COVID-19 on healthcare-associated infections in Canadian acute-care hospitals: Interrupted time series (2018–2021)
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, pp. s112-s113
-
- Article
-
- You have access
- Open access
- Export citation
Epidemiology of central-line–associated bloodstream infection mortality in Canadian NICUs before and after 2017
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, p. s48
-
- Article
-
- You have access
- Open access
- Export citation
How does the antimicrobial stewardship provider role affect prospective audit and feedback acceptance for restricted antibiotics in a Canadian tertiary-care center?
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 2 / February 2024
- Published online by Cambridge University Press:
- 18 August 2023, pp. 234-236
- Print publication:
- February 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
19 - Temperament, Family Context, and the Development of Coping
- from Part V - Social Contexts and the Development of Coping
-
-
- Book:
- The Cambridge Handbook of the Development of Coping
- Published online:
- 22 June 2023
- Print publication:
- 06 July 2023, pp 468-488
-
- Chapter
- Export citation
Complex cardiac implantable electronic device infections in Alberta, Canada: An epidemiologic cohort study of validated administrative data
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 10 / October 2023
- Published online by Cambridge University Press:
- 15 May 2023, pp. 1607-1613
- Print publication:
- October 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
294 Identification of MCAK Inhibitors that Induce Aneuploidy in Triple Negative Breast Cancer Models
- Part of
-
- Journal:
- Journal of Clinical and Translational Science / Volume 7 / Issue s1 / April 2023
- Published online by Cambridge University Press:
- 24 April 2023, p. 88
-
- Article
-
- You have access
- Open access
- Export citation
What Do You Do When You Can Do No More? Limited Resources, Unimaginable Environments, Personal Danger: What Have Previous Disasters Taught Us About Moral and Ethical Challenges?
-
- Journal:
- Disaster Medicine and Public Health Preparedness / Volume 17 / 2023
- Published online by Cambridge University Press:
- 11 April 2023, e373
-
- Article
- Export citation
Developmental care pathway for hospitalised infants with CHD: on behalf of the Cardiac Newborn Neuroprotective Network, a Special Interest Group of the Cardiac Neurodevelopmental Outcome Collaborative
-
- Journal:
- Cardiology in the Young / Volume 33 / Issue 12 / December 2023
- Published online by Cambridge University Press:
- 30 March 2023, pp. 2521-2538
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Expanding mental health services in low- and middle-income countries: A task-shifting framework for delivery of comprehensive, collaborative, and community-based care
-
- Journal:
- Cambridge Prisms: Global Mental Health / Volume 10 / 2023
- Published online by Cambridge University Press:
- 27 February 2023, e16
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
10 - Parenting That Promotes Positive Social, Emotional and Behavioral Development in Middle Childhood
- from Part II - Parenting across Development: Social, Emotional, and Cognitive Influences
-
-
- Book:
- The Cambridge Handbook of Parenting
- Published online:
- 01 December 2022
- Print publication:
- 15 December 2022, pp 213-235
-
- Chapter
- Export citation
Relationship building in pediatric research recruitment: Insights from qualitative interviews with research staff
-
- Journal:
- Journal of Clinical and Translational Science / Volume 6 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 03 October 2022, e138
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Mobilizing digital technology to implement a population-based psychological support response during the COVID-19 pandemic in Lima, Peru
-
- Journal:
- Global Mental Health / Volume 9 / 2022
- Published online by Cambridge University Press:
- 28 July 2022, pp. 355-365
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Participation in cost-offset community-supported agriculture by low-income households in the USA is associated with community characteristics and operational practices
-
- Journal:
- Public Health Nutrition / Volume 25 / Issue 8 / August 2022
- Published online by Cambridge University Press:
- 13 April 2022, pp. 2277-2287
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Acceptability and experience of a personalised proteomic risk intervention for type 2 diabetes in primary care: qualitative interview study with patients and healthcare providers
-
- Journal:
- Primary Health Care Research & Development / Volume 23 / 2022
- Published online by Cambridge University Press:
- 01 April 2022, e24
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Vancomycin-resistant Enterococcus sequence type 1478 spread across hospitals participating in the Canadian Nosocomial Infection Surveillance Program from 2013 to 2018
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 1 / January 2023
- Published online by Cambridge University Press:
- 10 March 2022, pp. 17-23
- Print publication:
- January 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Comparison of the performance of a clinical classification tree versus clinical gestalt in predicting sepsis with extended-spectrum beta-lactamase–producing gram-negative rods
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 07 March 2022, e35
-
- Article
-
- You have access
- Open access
- HTML
- Export citation