71 results
Associations between disturbed sleep and attenuated psychotic experiences in people at clinical high risk for psychosis
-
- Journal:
- Psychological Medicine , First View
- Published online by Cambridge University Press:
- 07 March 2024, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Endocannabinoid levels in plasma and neurotransmitters in the brain: a preliminary report on patients with a psychotic disorder and healthy individuals
-
- Journal:
- Psychological Medicine , First View
- Published online by Cambridge University Press:
- 23 February 2024, pp. 1-11
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Cannabis use as a potential mediator between childhood adversity and first-episode psychosis: results from the EU-GEI case–control study
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 15 / November 2023
- Published online by Cambridge University Press:
- 04 May 2023, pp. 7375-7384
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Tobacco use in first-episode psychosis, a multinational EU-GEI study
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 15 / November 2023
- Published online by Cambridge University Press:
- 26 April 2023, pp. 7265-7276
-
- Article
- Export citation
Genetic and psychosocial stressors have independent effects on the level of subclinical psychosis: findings from the multinational EU-GEI study
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 31 / 2022
- Published online by Cambridge University Press:
- 27 September 2022, e68
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
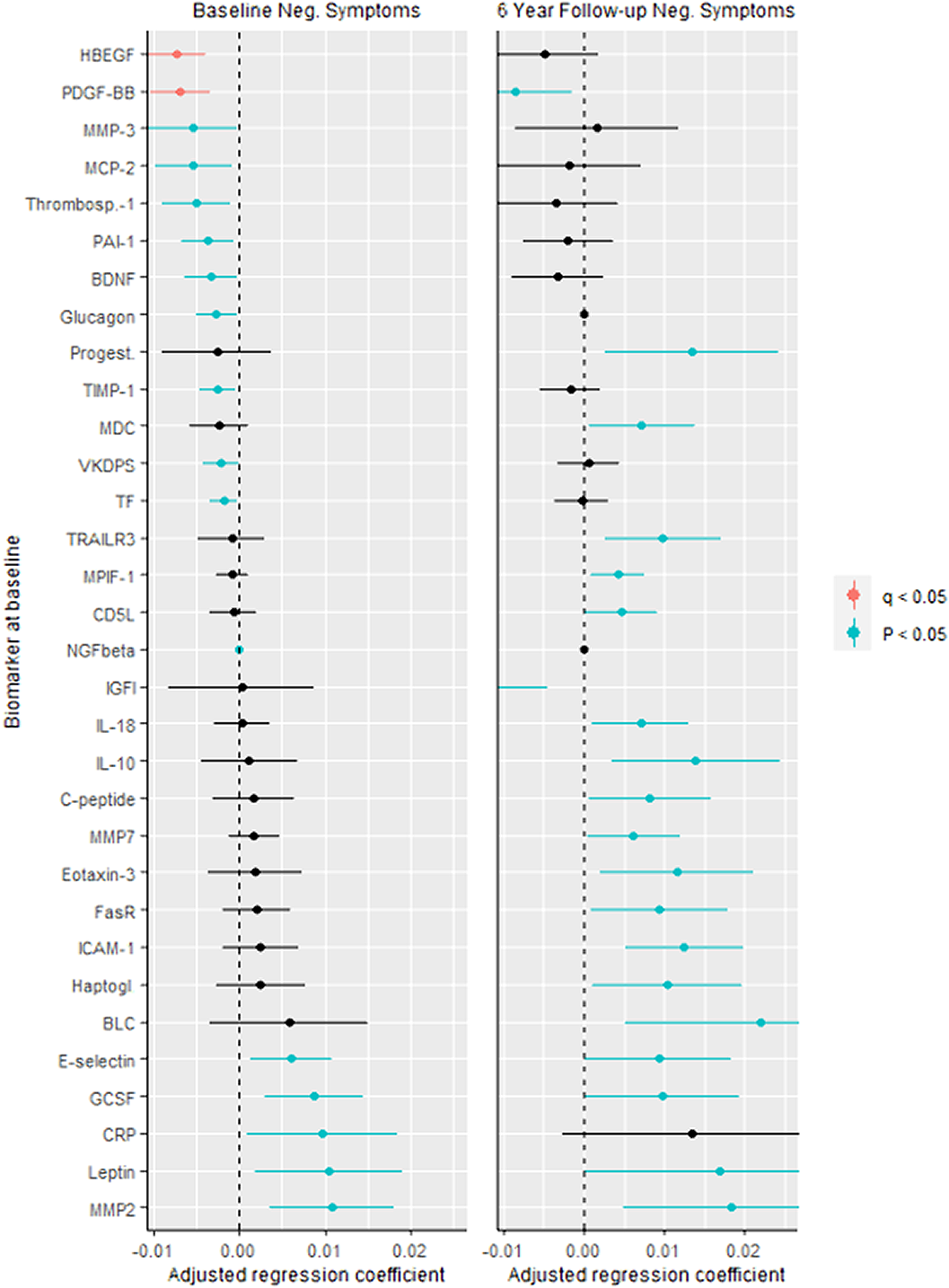
Predictive biomarkers for negative symptoms in schizophrenia
-
- Journal:
- European Psychiatry / Volume 64 / Issue S1 / April 2021
- Published online by Cambridge University Press:
- 13 August 2021, pp. S132-S133
-
- Article
-
- You have access
- Open access
- Export citation
Stress reactivity as a putative mechanism linking childhood trauma with clinical outcomes in individuals at ultra-high-risk for psychosis: Findings from the EU-GEI High Risk Study
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 30 / 2021
- Published online by Cambridge University Press:
- 28 May 2021, e40
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Changes in peripheral blood compounds following psychopharmacological treatment in drug-naïve first-episode patients with either schizophrenia or major depressive disorder: a meta-analysis
-
- Journal:
- Psychological Medicine / Volume 51 / Issue 4 / March 2021
- Published online by Cambridge University Press:
- 03 March 2021, pp. 538-549
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Imagery rescripting and eye movement desensitisation and reprocessing as treatment for adults with post-traumatic stress disorder from childhood trauma: randomised clinical trial
-
- Journal:
- The British Journal of Psychiatry / Volume 217 / Issue 5 / November 2020
- Published online by Cambridge University Press:
- 07 September 2020, pp. 609-615
- Print publication:
- November 2020
-
- Article
-
- You have access
- HTML
- Export citation
Verbal fluency as a possible predictor for psychosis
-
- Journal:
- European Psychiatry / Volume 25 / Issue 2 / March 2010
- Published online by Cambridge University Press:
- 16 April 2020, pp. 105-110
-
- Article
- Export citation
Priorities and satisfaction on the help needed and provided in a first episode of psychosis. A survey in five European Family Associations☆
-
- Journal:
- European Psychiatry / Volume 17 / Issue 8 / December 2002
- Published online by Cambridge University Press:
- 16 April 2020, pp. 425-433
-
- Article
- Export citation
Duration of untreated psychosis and the long-term course of schizophrenia
-
- Journal:
- European Psychiatry / Volume 15 / Issue 4 / June 2000
- Published online by Cambridge University Press:
- 16 April 2020, pp. 264-267
-
- Article
- Export citation
Preferences for treatment during a first psychotic episode
-
- Journal:
- European Psychiatry / Volume 16 / Issue 2 / March 2001
- Published online by Cambridge University Press:
- 16 April 2020, pp. 83-89
-
- Article
- Export citation
Opinions of mothers on the first psychotic episode and the start of treatment of their child
-
- Journal:
- European Psychiatry / Volume 19 / Issue 4 / June 2004
- Published online by Cambridge University Press:
- 16 April 2020, pp. 226-229
-
- Article
- Export citation
Long-term Outcome in Schizophrenia: a Six-year Follow-up in over 1000 Patients
-
- Journal:
- European Psychiatry / Volume 30 / Issue S1 / March 2015
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
1595 – The Effects Of Mixing Alcohol With Caffeinated Beverages On Subjective Intoxication
-
- Journal:
- European Psychiatry / Volume 28 / Issue S1 / 2013
- Published online by Cambridge University Press:
- 15 April 2020, 28-E881
-
- Article
-
- You have access
- Export citation
Interventions to improve adherence to antipsychotic medication in patients with schizophrenia–A review of the past decade
-
- Journal:
- European Psychiatry / Volume 27 / Issue 1 / January 2012
- Published online by Cambridge University Press:
- 15 April 2020, pp. 9-18
-
- Article
- Export citation
EPA-0767 – Plasma Oxytocin and Testosterone Levels in Patients with Psychotic Disorder, Their Unaffected Siblings and Healthy Controls: Results from the EU-GEI Project
-
- Journal:
- European Psychiatry / Volume 29 / Issue S1 / 2014
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
Transdiagnostic Exploration of the Association of Toxoplasma Gondii with Psychiatric Disorders. a Systematic Review and Meta Analysis
-
- Journal:
- European Psychiatry / Volume 30 / Issue S1 / March 2015
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
Association of treatment delay, migration and urbanicity in psychosis
-
- Journal:
- European Psychiatry / Volume 27 / Issue 7 / October 2012
- Published online by Cambridge University Press:
- 15 April 2020, pp. 500-505
-
- Article
- Export citation