Book contents
- How to Prepare the Endometrium to Maximize Implantation Rates and IVF Success
- How to Prepare the Endometrium to Maximize Implantation Rates and IVF Success
- Copyright page
- Contents
- Contributors
- Preface
- Chapter 1 Physiology of Endometrial Development through the Cycle and Implantation
- Chapter 2 Molecular and Cellular Basis of Human Embryo Implantation
- Chapter 3 Protein Biomarkers of Endometrial Receptivity
- Chapter 4 Genetic Markers of Endometrial Receptivity
- Chapter 5 Effects of Superovulation on the Endometrium
- Chapter 6 Screening the Uterine Microbiome Prior to Embryo Transfer
- Chapter 7 Estrogen and Progesterone Support in ART
- Chapter 8 The Role of Hysteroscopy and Endometrial Scratch in Improving Endometrial Receptivity
- Chapter 9 Fibroids and Polyps
- Chapter 10 Cleavage Stage or Blastocyst Transfer
- Chapter 11 Dummy Embryo Transfer
- Chapter 12 Does Catheter Type Influence Endometrial Implantation Success?
- Chapter 13 Should All Embryos Be Transferred in Unstimulated Cycles?
- Chapter 14 Rest after Embryo Transfer Is Unhelpful
- Chapter 15 Ectopic Pregnancies: Why Do They Happen?
- Chapter 16 The Role of NK Cells in Implantation after IVF and Treatment Strategies
- Chapter 17 Sex and Immune Receptivity for Embryo Transfer
- Chapter 18 Immunotherapy/IVIG, Prednisolone and Intralipid in IVF
- Chapter 19 The Role of Heparin and Aspirin to Aid Implantation
- Chapter 20 Early Pregnancy Loss
- Chapter 21 Is the Endometrium in Women with PCOS Compromised?
- Index
- References
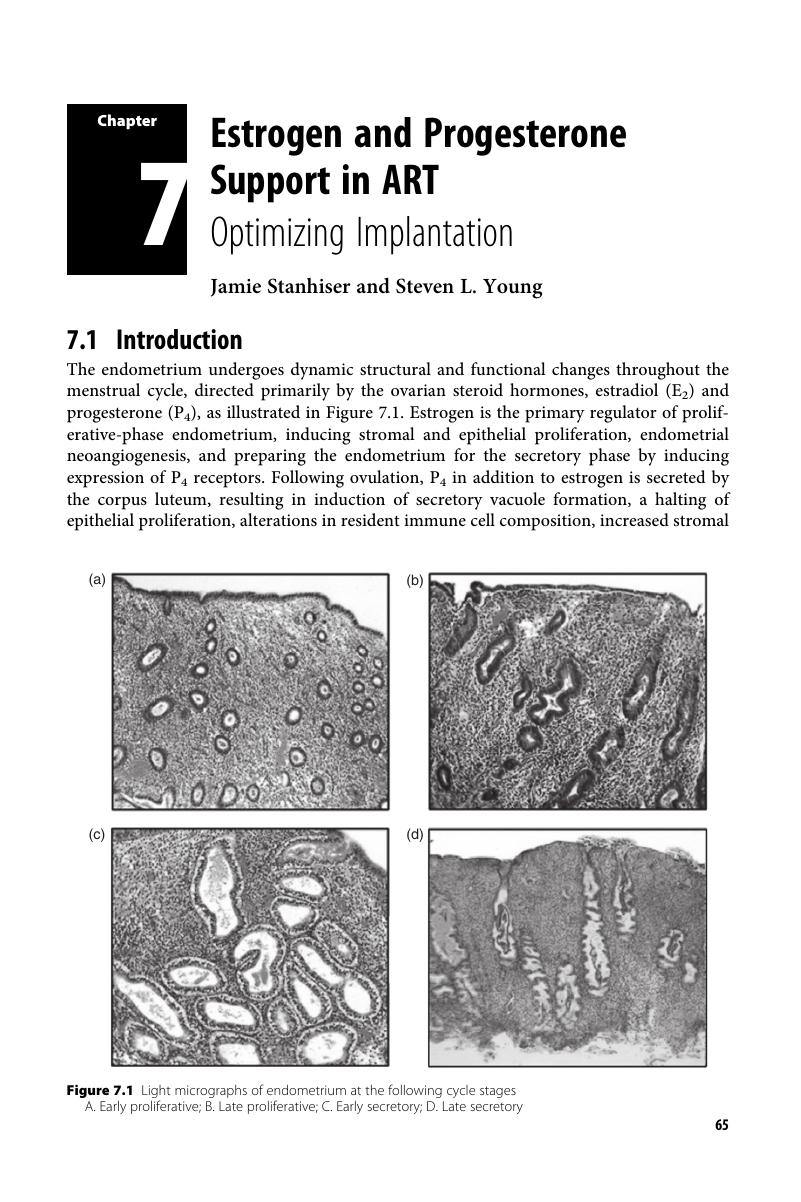
Chapter 7 - Estrogen and Progesterone Support in ART
Optimizing Implantation
Published online by Cambridge University Press: 07 January 2019
- How to Prepare the Endometrium to Maximize Implantation Rates and IVF Success
- How to Prepare the Endometrium to Maximize Implantation Rates and IVF Success
- Copyright page
- Contents
- Contributors
- Preface
- Chapter 1 Physiology of Endometrial Development through the Cycle and Implantation
- Chapter 2 Molecular and Cellular Basis of Human Embryo Implantation
- Chapter 3 Protein Biomarkers of Endometrial Receptivity
- Chapter 4 Genetic Markers of Endometrial Receptivity
- Chapter 5 Effects of Superovulation on the Endometrium
- Chapter 6 Screening the Uterine Microbiome Prior to Embryo Transfer
- Chapter 7 Estrogen and Progesterone Support in ART
- Chapter 8 The Role of Hysteroscopy and Endometrial Scratch in Improving Endometrial Receptivity
- Chapter 9 Fibroids and Polyps
- Chapter 10 Cleavage Stage or Blastocyst Transfer
- Chapter 11 Dummy Embryo Transfer
- Chapter 12 Does Catheter Type Influence Endometrial Implantation Success?
- Chapter 13 Should All Embryos Be Transferred in Unstimulated Cycles?
- Chapter 14 Rest after Embryo Transfer Is Unhelpful
- Chapter 15 Ectopic Pregnancies: Why Do They Happen?
- Chapter 16 The Role of NK Cells in Implantation after IVF and Treatment Strategies
- Chapter 17 Sex and Immune Receptivity for Embryo Transfer
- Chapter 18 Immunotherapy/IVIG, Prednisolone and Intralipid in IVF
- Chapter 19 The Role of Heparin and Aspirin to Aid Implantation
- Chapter 20 Early Pregnancy Loss
- Chapter 21 Is the Endometrium in Women with PCOS Compromised?
- Index
- References
Summary
- Type
- Chapter
- Information
- Publisher: Cambridge University PressPrint publication year: 2019