Double burden of malnutrition has been known as a global problem. Around 88 % of countries face the overlapping burden of malnutrition (under- and overnutrition), while low-middle income countries are the most affected(1). Nutrition transition, characterised by the population shifts in dietary and physical activity patterns as the consequence of rapid economic development and urbanisation, may explain the double burden problem. The clustering of stunting and overweight is an indication of individual-level double burden of malnutrition(2). In Indonesia, among stunted children (under 5 years old), prevalence of overweight was 6·8 %, slightly higher than the prevalence of overweight among children who were not stunted (5·1 %)(Reference Rachmi, Agho and Li3). Concurrent stunting and overweight in young children has been described in other countries. Stunting is a chronic undernutrition which the process of its development begins at birth, or even earlier during the fetus stage. Fetal metabolic adaptation to intra-uterine nutrient-deficient environment would continue to effect after the fetus is born(Reference Shrimpton and Rokx4). When they grow up under favourable environmental conditions which provide adequate foods, their body failed to adapt to this mismatch between two different environments which may lead to overweight(Reference Hoffman, Roberts and Verreschi5). It is a puzzle why malnutrition coexists with economic growth and nutrition transition. Socio-economic status, maternal education level, living in a larger household, and living in rural areas are well-known risk factors of children’s concurrent stunting and overweight(Reference Rachmi, Agho and Li3,Reference Fernald and Neufeld6–Reference Said-Mohamed, Allirot and Sobgui12) . Recently, household structure has been suggested to be an important factor which might play a role on children’s nutritional status(Reference Kumar and Ram13,Reference Novak and Muniagurria14) .
Previous studies have shown that household structure, such as nuclear and extended family, was associated with children’s nutritional status(Reference Kumar and Ram13–Reference Annim, Awusabo-Asare and Amo-Adjei15). Other studies have demonstrated that child’s nutritional status was associated with the household size as well as the number and type of adults residing in the household(Reference Annim, Awusabo-Asare and Amo-Adjei15). Family environment in which individuals interact daily has a significant impact on individuals’ physical and mental growth, particularly for young children who are not yet in school(Reference Schmeer16), since parents and other adults living in the family become role models of health behaviours, such as food choices and physical activity(Reference Formisano, Hunsberger and Bammann17). Household human capital is important for young children’s health, since it can be translated into either economic support or caregiving, which directly related to the living condition of the children(Reference Kumar and Ram13). The distribution of household resources could happen in various ways depends on the household context, their size and composition(Reference Annim, Awusabo-Asare and Amo-Adjei15), such as number of children and adults, the presence of parents, as well as the presence of other relatives or even non-relative members in the households.
In Indonesia, family and household structure is changing with the wider process of demographic transformation. The change in the household arrangement is both an outcome and a basis of household economic change(Reference Qibthiyyah and Utomo18). The average household size in Indonesia has dropped gradually during the last four decades, from 4·9 in 1971 to 3·9 in 2013(Reference Qibthiyyah and Utomo18). Nuclear family which consists of parent(s) and their children is becoming the model of society and quickly replacing the conventional extended family. Such trend might create a challenge of family support for young children and elderly(Reference De Silva19). In 1991, the proportion of extended family was 27·4 %(Reference Effendi and Sukamdi20) and in 2013, it decreased to 14·8 %(21). However, the proportion of nuclear family was also decreased, 68·4 % in 1991(Reference Effendi and Sukamdi20) to 53·8 % in 2013(21). This situation could be explained by the increasing share of other types of household, including single-parent household and single-headed household since the era of 90s(Reference Effendi and Sukamdi20). The patterns in the changes of household structure differed between urban and rural areas because the pattern of demographic and social changes also differed between the two regions(Reference Effendi and Sukamdi20). Migration of productive age population from rural to urban is one of the reasons that result in differences in the patterns of change between rural and urban. Grandfamily is a novel social phenomenon in rural area where the children’s parents migrate to the city for work, so that grandparents take care of these left-behind children(Reference Qibthiyyah and Utomo18).
However, few studies have explored the relationship between household structure and children’s nutritional status. The purposes of the present study were to: (i) estimate the prevalence of concurrent stunting and overweight in Indonesian children aged 2–5 years and (ii) examine the association of household structure (household type and composition) with concurrent stunting and overweight in young children in urban and rural Indonesia.
Methods
Study design
The study was based on the data of Indonesia Basic Health Research (Riset Kesehatan Dasar/Riskesdas) conducted in year 2013. This health survey is a periodic, population-based, cross-sectional, nationally representative survey that was initiated since 2007 by the National Institute of Health Research Development (NIHRD), Ministry of Health, Indonesia. This survey pointed to collect basic data and health indicators describing the health conditions at nationwide, province and district levels. Riskesdas 2013 managed to cover households from all provinces (33 provinces) in Indonesia with response rate of 98·3 % (household) and 93 % (individual). A multistage systematic random sampling method consisting of four stages sampling was applied in this survey. First, groups of census blocks were identified and designated as primary sampling units. Second, a census block from each primary sampling unit was identified using a probability proportional to size design. Third, systematic random sampling of 25 census buildings from each census block was done. The final stage was choosing one household from each census building randomly. All household members, defined as those staying in the household for the past half-year or more and having the same financial source for foods(22), of every selected household were asked to participate in the survey. The sampling and methods have been described in detail elsewhere(2).
The household and individual information were collected by face-to-face interviews using questionnaire with the household head or housewives or other household member who were able to provide information. Meanwhile, direct measurements of various data, such as anthropometric data and physical examinations, were also done for the participants.
Study population
The 1 027 763 participants were aged from 0 months to 75 years in the national survey. This study only focused on 51 733 children aged 2–5 years. Out of those, 6245 children were excluded (were not provided by NIHRD because of 5817 data with incomplete information and 428 not matched to any household data). Additionally, 438 participants were excluded because they were not the children or grandchildren of the household head, so that the focal child’s household type cannot be defined. Finally, 45 050 children were included into the analysis. The minimum age was chosen at 2 years (24 months), since rapid growth faltering including the stunting process is more salient before the age of 2 years(Reference Victora, de Onis and Hallal23).
Outcome measures
Children nutritional status was measured using the indicator of WHO child growth standard(24). Children’s body weight was directly measured by well-trained interviewers using digital weight scale with a capacity of 150 kg and precision of 0·1 kg and calibrated on daily basis. Height was also directly measured using a multi-function brand stadiometer with a capacity of 2 m and a precision of 0·1 cm. Stunting was defined by height-for-age Z-score <–2, while overweight was defined by body weight/height Z-score >+2. Concurrent stunting and overweight was defined as the presence of both stunting and overweight in individual.
Exposure measures
Household structure variables were constructed using the information of household member. Head of household was used as a reference to define the relationship of each household member. Household structure was investigated by six components: (i) household type; (ii) household size; (iii) number of working adults in the household; (iv) number of dependent adults (non-working adults); (v) number of dependent children; and (vi) gender of the head of the household.
Household type was categorised as follows: (i) nuclear two-parent household; (ii) nuclear one-parent household; (iii) extended household and (iv) grandfamilies. Nuclear household was defined as household which consist of parent(s) and children, no differentiation was made between biological and non-biological children. Extended household consisted of parent(s), their children, and the presence of one or more relatives. Grandfamilies were defined as household which consist of grandparent(s) and their grandchildren. Household size was calculated by summing the number of people who usually resided in the household but did not include those who have left for 6 months or more. Number of working adults was defined as total number of household member aged 15 years and older who had occupation, while number of dependent adults is the total number of household member aged 15 years and older who were unemployed. These two variables did not include household member who did not have family relation to the children, such as housemaid, gardener, driver, etc. Number of dependent children was calculated by summing the number of household members aged less than 15 years. Gender of household head was defined as male-headed and female-headed households.
Confounders
The potential confounders of the association between household structure and concurrent stunting and overweight in children include child’s gender, age of the head of the household as well as their education level, socio-economic status as measured by household wealth index (1 to 5 meaning from poorest to richest) and residency area (urban/rural). Data on household wealth index were available from the survey. It was measured from the possession of durable items using principal component analysis (PCA) to produce single indicator for economic status. Detail methods on wealth index determination were described elsewhere(2).
Statistical analysis
The statistical analysis was performed using STATA version 15. The statistical significance was considered at P-value ≤ 0·05. Descriptive statistics were presented as proportion for the categorical variables, and mean and standard deviation for continuous variables. Pearson’s chi-squared test and ANOVA (one-way ANOVA) were performed to assess the difference of children’s characteristics and nutritional status between the groups of household type. Taking into account of the clustering effect at household level, univariate and multivariable logistic regressions with cluster-adjusted robust standard error were run separately for urban and rural areas to assess the relationship between household structure variables and the concurrent stunting and overweight in children. Additional clustering at district level is already accounted for in the sampling. We treated the continuous variables of household size, number of working adults, number of dependent adults and number of dependent children as categorical in the logistic regression model, due to the non-linear relationship between those variables and the outcome of interest. All of the analyses were weighted to reflect national estimates. Multivariable models were adjusted for important confounding variables: age and education level of the head of the household, household wealth index, residency area, and child’s gender. Additionally, the analysis for household composition (household size, number of working adults, number of dependent adults and number of dependent children) and gender of the household head was further adjusted for the household type. Children’s gender did not show any modification effect on the hypothesised association, so all the analyses pooled boys’ and girls’ data.
Results
Characteristics of participants
Characteristics of participants according to the household type are shown separately for urban and rural areas in Tables 1 and 2, respectively. The majority of children from both urban and rural areas lived in nuclear two-parent households. Household head’s characteristics (age, gender and education level) and socio-economic status were significantly different between the four household type categories. In both residency areas, nuclear households mostly were leaded by younger household head, with higher proportion of secondary and higher degree of education level in nuclear two-parent households when compared with the other household type groups. Meanwhile, the household heads in the grandfamilies were older and had higher proportion of lower education level. Generally, the proportion of low education level of the household head and lower socio-economic status were higher among rural households than their urban counterparts. The majority of households were male-headed. However, this was not the case for nuclear one-parent households where the majority of this household type were female-headed, 87 % and 79·3 % in urban and rural areas, respectively.
Table 1 Comparison of household and children’s characteristics by household structure in urban areas (weighted analysis)
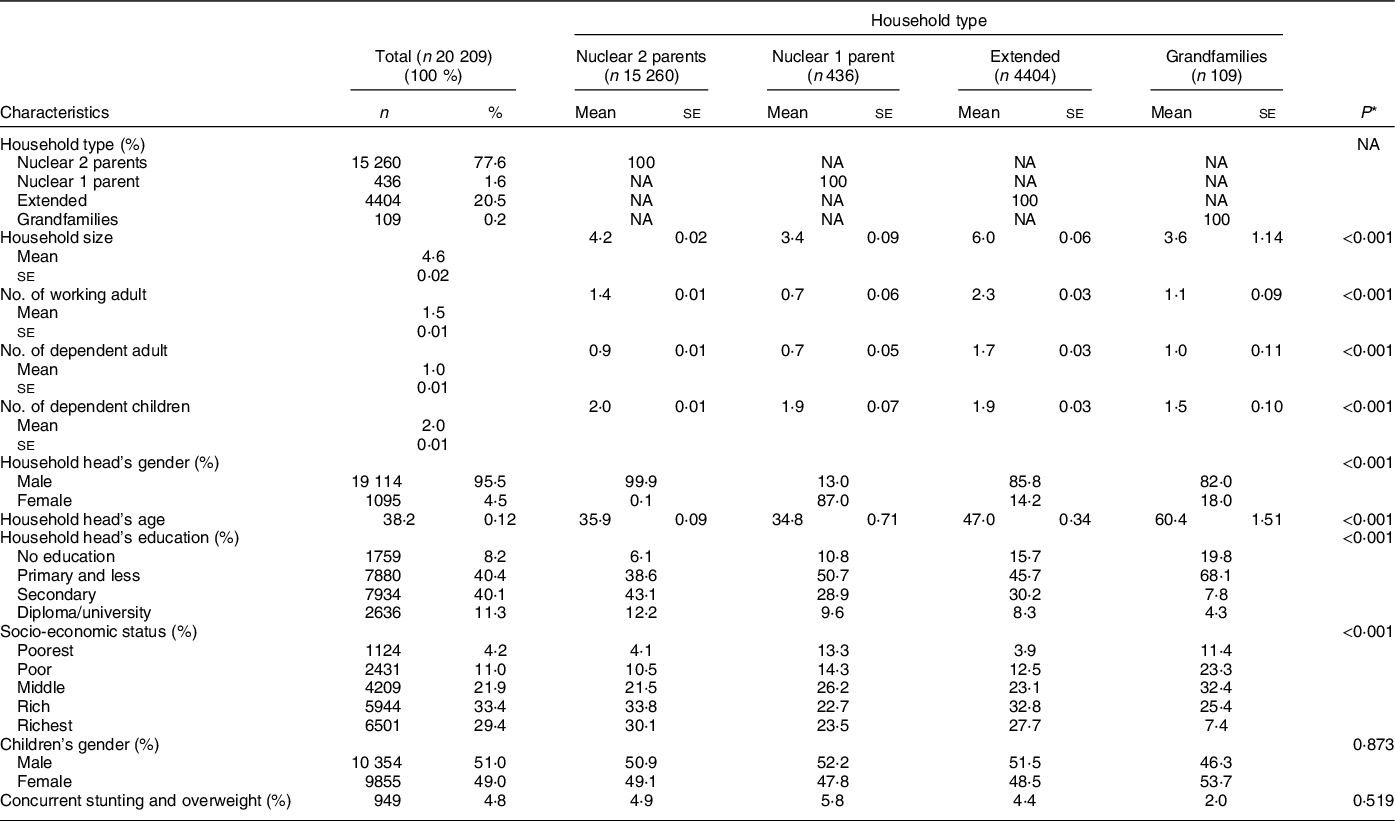
NA, not applicable.
* P values from χ 2 tests (for categorical variables) or ANOVA (for continuous variables) for comparisons between the groups of household type.
Table 2 Comparison of household and children’s characteristics by household structure in rural areas (weighted analysis)

NA, not applicable.
* P values from χ 2 tests (for categorical variables) or ANOVA (for continuous variables) for comparisons between the groups of household type.
Household compositions differed significantly by household type. Extended households tended to have more people as shown with the higher mean of household size, and also greater mean of number of working adults and dependent adults when compared to nuclear households and grandfamilies. However, nuclear households had slightly higher mean of number of dependent children when compared to the other household types.
Figure 1 shows that the prevalence of concurrent stunting and overweight in children aged 2–5 years is 5·6 % in the study population. Fig. 1 also suggests that the prevalence of this outcome is significantly higher among children from rural regions than children from urban regions (P < 0·001). There is evidence of differentials in children nutritional status by household type, particularly in rural areas, as we can see in the last row of Table 2, the prevalence of concurrent stunting and overweight was higher among children lived in nuclear two-parent households, then nuclear one-parent households, followed by children from grandfamilies and the lowest was among children from extended households (P < 0·001).
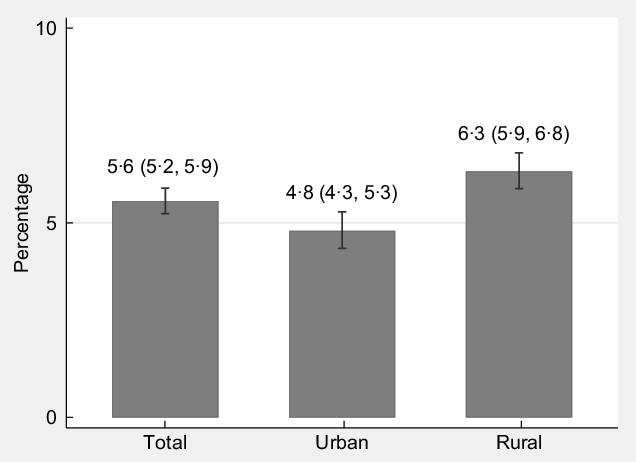
Fig. 1 Prevalence of concurrent stunting and overweight in Indonesian children aged 2 to 5 years (weighted percentage with 95 % CI)
Association between household structure and concurrent stunting and overweight
Tables 3 and 4 present the results separately for urban and rural areas, respectively. In rural areas, the result after adjusting for confounders in model 2 suggested that children from extended households were significantly less likely to be concurrently stunted and overweight when compared to those from nuclear two-parent households. Surprisingly, household type did not have a significant association on the concurrent stunting and overweight in children from urban areas (Table 3). The finding also revealed no significant different in the OR of concurrent stunting and overweight when comparing children from nuclear one-parent households or grandfamilies to those from nuclear two-parent households.
Table 3 Association between household structure and concurrent stunting and overweight in children in urban areas (weighted analysis)
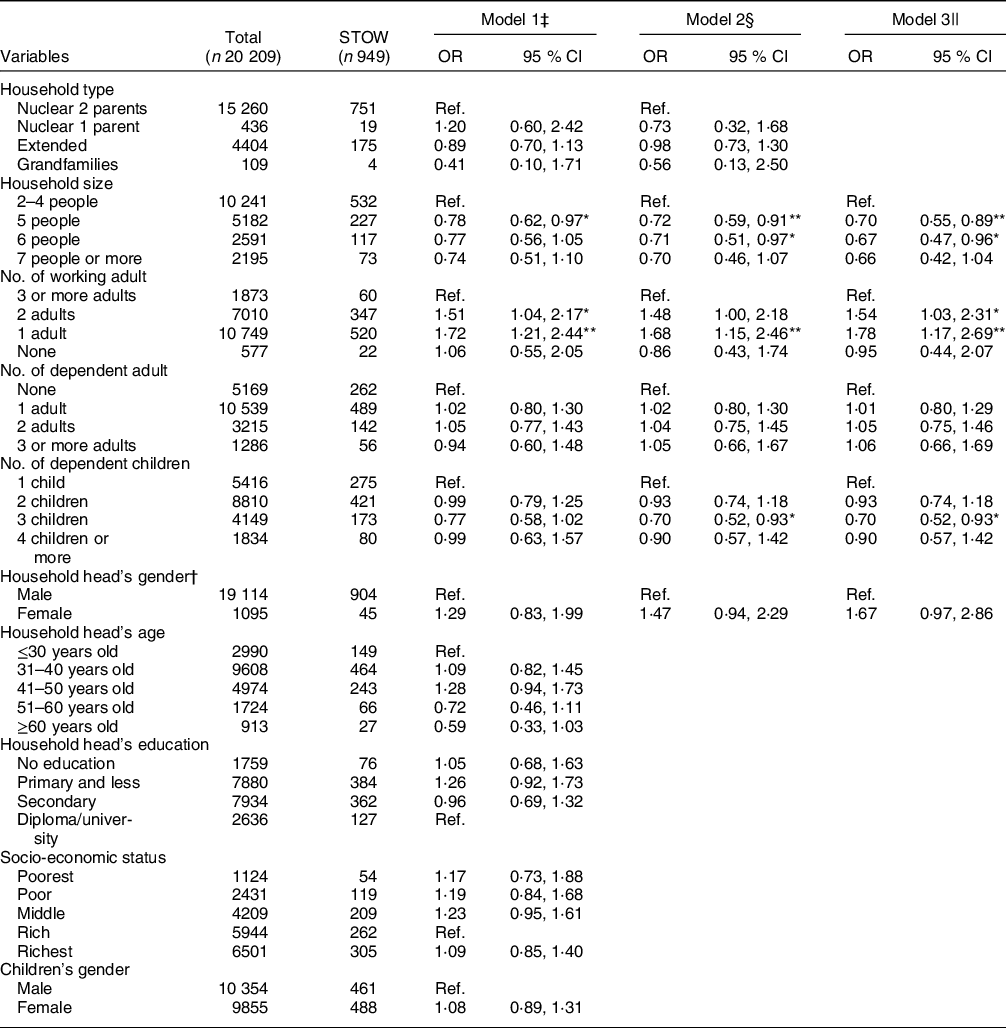
STOW, concurrent stunting and overweight; Ref. reference category.
* P-value <0·05.
† For variable household head’s gender, model 2 is adjusted for confounders (residency area, household wealth index, household head’s age, household head’s education level and children’s gender), model 3 is model 2 and further adjusted for household type.
‡ Model 1, univariate analysis.
§ Model 2, adjusted for confounders (residency area, household wealth index, household head’s age, household head’s education level and children’s gender) and household head’s gender.
|| Model 3, model 2 and further adjusted for household type.
** P-value <0·01.
Table 4 Association between household structure and concurrent stunting and overweight in children in rural areas (weighted analysis)

STOW, concurrent stunting and overweight; Ref. reference category.
* P-value <0·05.
† For variable household head’s gender, model 2 is adjusted for confounders (residency area, household wealth index, household head’s age, household head’s education level and children’s gender), model 3 is model 2 and further adjusted for household type.
‡ Model 1, univariate analysis.
§ Model 2, adjusted for confounders (residency area, household wealth index, household head’s age, household head’s education level and children’s gender) and household head’s gender.
|| Model 3, model 2 and further adjusted for household type.
** P-value <0·01.
Another important finding from this study was that the association between household size and concurrent stunting and overweight in children differed for urban and rural areas. The results observed in urban areas suggested that larger household size was associated with lower odds of concurrent stunting and overweight in children. Stronger association was observed in the multivariable models. On the contrary, the aforementioned association was not really consistent in rural areas and it went to different direction. A marginally significant positive association between household size and the odds of concurrent stunting and overweight in children was observed in the final model (Table 4, model 3).
Along with that finding, we found that in urban areas, lower number of working adults was associated with a higher likelihood of being concurrently stunted and overweight in children. However, such association was not observed in their rural counterparts. Instead, number of dependent adults showed an association with the concurrent stunting and overweight in children from rural areas. As shown in Table 4, children from a household with the presence of three or more dependent adults were significantly less likely to be concurrently stunted and overweight than those from a household without the presence of dependent adult. Although adjusting for other covariates eliminated the statistical significance of the association, however the direction of the association remained. Another interesting finding from this study was that in rural areas, children from female-headed households were significantly more likely to be concurrently stunted and overweight when compared to those living in male-headed households after adjusting for household type.
The results in urban and rural areas showed a different pattern of the association. The relationship of some household composition variables and the outcome went into the opposite direction, such as household size. Notwithstanding, we did not find any significant interaction terms between urban–rural residency and categorical household composition variables.
Discussion
The present study demonstrated that household structure, as household type and household composition, was associated with concurrent stunting and overweight in children. This study found evidence to support the existing literature regarding the association between household type and children’s nutritional status, as this study suggested that children living in extended households had lower odds to be concurrently stunted and overweight than those living in nuclear households. This association was observed in rural areas but not in urban areas.
The favourable effect of children living in extended households is consistent with previous studies of preschool children that found children from a non-nuclear or extended family had better nutritional status than those in nuclear families(Reference Kumar and Ram13,Reference Novak and Muniagurria14) . Such a relationship might be because the extended households provide better social care for its member and therefore is more likely to offer important resources, that is, food and health care. In extended households, the presence of other adult in the household could provide material assistance such as child care as well as increase the chance of health care utilisation(Reference Kumar and Ram13). This is important for child’s wellbeing, especially when the parents are absent due to their engagement in domestic duties or economic activity(Reference Griffiths, Matthews and Hinde25). Some authors also highlighted the importance of extended household as an important mechanism for pooling economic resources and distributing domestic labour(Reference Madhavan and Townsend26). Another study provides evidence that extended family resources matter for child development outcomes and that in Indonesian context, extended family appear to be able to allocate resources efficiently(Reference LaFave and Thomas27). However, in this study, the pooling economic resources in extended households might not be the explanation for the finding, since we controlled for the household wealth index in the analysis. Therefore, the observed result in regard to the favourable influence of extended household for children’s nutritional status could be explained by other pathways which is the availability of household non-financial resources or the social dimension of household type.
The different finding regarding the association between household type and the odds of concurrent stunting and overweight among children from urban and rural might be due to the difference in the household composition and the differences in the availability of time to care or the presence of additional caregivers between urban and rural households. A study from Ivory Coast could illustrate these differences. This study found that the percentage of dependent adults in extended households is relatively high in urban zones, whereas it was not the case in rural extended households. In such cases, the dependent extended household members become a burden for those households in urban areas(Reference de Laiglesia and Morrison28). In contrast, the presence of relatives in extended households in rural areas does not create any burden relatively to nuclear households. Instead, their presence could support the need of household members, including the care for young children.
This study also suggested that the association between household size and concurrent stunting and overweight differed for urban and rural. Larger household size was associated with lower odds of concurrent stunting and overweight in children from urban regions, while in rural regions, it was associated with the higher odds of outcome. These findings show how the relationship between household size and children’s nutritional status varies by residency area within a country. The unfavourable influence of larger household size on child’s outcome often explained that there is more competition for available household resources, and that this resource dilution will be more severe under finite resources(Reference Henry-Unaeze and Ibe29). Resources need to be divided among several members and less wealth can be invested per person in large families(Reference Suomalainen30).
In this study, the results obtained in urban regions illustrated that in some settings, the quality–quantity trade-off pathway, which refers to an increasing marginal cost of quality (child outcome) with respect to quantity (number of children or family size) leads to a trade-off between quantity and quality(Reference Becker and Lewis31), may not hold. In certain context, having more household members might have advantages, to share household works and to provide care for young children in the household, which may influence child development in a desired way(Reference Maralani32). Young age is a period when the presence of parents or caregiver at home is the most in need. Age under 5 years is critical time for child development, a period when environmental influences from the outside could be mitigated by family(33). Optimal care that household member could offer to young children will become the foundation for lifelong health and wellbeing for children throughout their life course(33). Thus, larger household size is beneficial when the household member could support and promote the development of young children.
In addition to that, specific context factors such as family organisation and cultural roles determine how parents allocate wealth to their children, and whether the burden of raising children is limited to the nuclear family or it is also borne by extended family networks(Reference Maralani32). In a traditional Indonesian context, extended household usually represents a form of familism which means family members are interdependent in both moral and material supports(Reference French, Rianasari and Pidada34), and the responsibility of child rearing would be shared among extended family members(Reference Schroder-Butterfill35). Another reason which might explain this finding is the different household composition that more number of people residing in the households in urban areas usually means that the household has more working adults who are contributing to child’s support(Reference Madhavan and Townsend26). Thus, in urban setting, the negative effect of larger household size based on resources dilution theory could be compensated by the number of working adults in the household.
Another important finding from this study is that the odds of concurrent stunting and overweight were higher among children living in a household with lower number of working adults, and it was only found in urban but not in rural regions. Working adults in the households present itself on different sides of a spectrum in terms of household resources which are directly related to children wellbeing. Firstly, increased number of working adults results in greater economic resources for the household; secondly and consequently, increased number of working adults results in loss of adult presence in the household(Reference Ng36). Loss of adult presence in the household is a drawback and outweighs the economic benefits provided by the increase in working adults as this is a reduction in the availability of time to care for children, thus, directly influencing health outcomes which may be the case in rural areas.
In urban regions, it is also noted that more number of working adults in a household is related to higher wealth, meanwhile in rural regions, more number of working adults is not necessarily reflecting better economic condition of the household. This is possibly due to the difference in job type and earnings for people living in urban and rural areas. Existing literature suggests that there is a gap of welfares between urban and rural households. In addition, there is a different social and economic opportunities for people who live in urban and rural regions(Reference Shedenova and Beimisheva37). Therefore, the influence of working adults on children nutritional status will be differed by household context.
The results of this study also revealed that gender of the household head had a significant association with children’s nutritional status only after adjusting for household type, particularly in rural areas. Previous studies in Ethiopia found that female headship increased the likelihood of stunting and underweight among preschoolers(Reference Haidar and Kogi-Makau38) and also increased the vulnerability to household food insecurity(Reference Negesse, Jara and Habtamu39). In most developing countries, female-headed households are prone to poverty, and they have less access to both job opportunities and government services which then will affect child’s outcome(Reference Haidar and Kogi-Makau38,Reference Dungumaro40) .
In addition, the aforementioned association was only significant in rural areas after controlling for household type. Further exploring the data of this study, among female-headed households, we found a significant difference in the distribution of household type in urban and rural areas (results are not shown in table): there was a higher proportion of nuclear one-parent households and grandfamilies in rural than urban. Female head in nuclear one-parent families and grandfamilies means that these households are single-mother households and grandmother–grandchildren households, respectively. Children living in these household types may be particularly vulnerable to malnutrition because the household head may have time constraint to take care of their children(Reference Dungumaro40), may own less health-related knowledge, particularly for grandmother in rural areas(Reference Young, Duncanson and Burrows41), or may have lower social and emotional support(Reference Dungumaro40).
To the best of our knowledge, this is the first study focusing on household type and composition in relation to concurrent stunting and overweight in Indonesia, thus providing new insights on this association. Another strength of our study include the big sample size from a nationally representative data that make the finding generalisable to wider population. In addition to that, the direct measurement of body weight and height in the survey to determine children’s nutritional status could minimise the possibility of measurement error.
The study has several limitations. First, it was the cross-sectional design of this study which limits the ability to draw causal relationship. The results of this study should be viewed under the assumption that household structure and household characteristics have been constant throughout each child’s life. In Indonesia, the reduction in household size was modest, from 4·0 in 2000 to 3·9 in 2013(Reference Qibthiyyah and Utomo18). In addition, research suggested that family structures tend to be more stable during child’s early life; for example, a study from China revealed that the lower the child’s age, the lower the divorce risk(Reference Xu, Yu and Qiu42). Although it is more likely that household structure affects child’s health than that child’s health affects household structure, the observed associations in the present study were not necessarily causation.
Second limitation was the potential misclassification of household structure. Based on the operational definition applied in the Riskesdas, household member did not include those who have left the house for at least 6 months. If the household member lived separately with the family because they worked in a different place, they actually still made some contribution to household resources, then our variable on household composition (household size and number of working adults) might not reflect the true situation, in other words, it opens the possibility of misclassification of household composition variables. Nevertheless, we adjusted for household wealth index to account for the influence of economic contributions from the family members living outside the household. Third, due to data availability, this study could only examine the status of concurrent stunting and overweight v. other and could not determine the prevalence of overweight and prevalence of stunting separately. Based on the latest Indonesian national survey in 2018, the prevalence of stunting among children under 5 years of age was 30·8 %, while the prevalence of overweight in the same age group was 8 %(43). Future research is needed to investigate the association between family structure and each of these nutritional status. Fourth, child’s age was not able to be linked in the dataset, so the study could not adjust for child’s age. Since child’s age is not likely to affect household structure, it is not a confounder to be adjusted for. Fifth, for 438 children who were not directly related to household head, we cannot determine the household type. Despite the very small percentage in the sample, this group could be particularly vulnerable for malnutrition.
Despite the large sample size and representativeness of the national survey, longitudinal follow-up study design is required to elucidate the temporality. Furthermore, as stunting is a national health challenge in Indonesia, it is imperative to design effective interventions for eradicating stunting while preventing the risk of overweight for different types of families.
In summary, this study provides evidence of the relationship between household structure and concurrent stunting and overweight in children. We observed some differences in the aforementioned associations between urban and rural regions, although the interaction term between household structure variables and urban–rural residency was not significant. Nevertheless, it is still important to take into account of urban and rural context in understanding how household type and composition are associated with child’s nutritional status. The present study also delivers an important message regarding the higher risk group of children to double burden of malnutrition at individual level, based on their household structure, both in urban and rural areas of Indonesia. Therefore, household structure should be considered in designing socio-economic intervention to address double burden of malnutrition in young children in both urban and rural regions.
Acknowledgements
Acknowledgements: The authors would like to thank the National Institute of Health Research and Development (NIHRD), Ministry of Health Republic of Indonesia for providing the 2013 Riskesdas data. Financial support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Conflict of interest: There are no conflicts of interest. Authorship: C.C. conceived the research question, reviewed literature, designed the study, obtained data, analysed data and wrote the manuscript. H.J.C. refined the research question formulation, designed variable definition and data analysis, supervised the data analysis and refined the analysis, reviewed the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Health Research Ethics Commission (KEPK), National Institute of Health Research and Development (Balitbangkes), Ministry of Health Republic of Indonesia. Written informed consent was obtained from all subjects/patients.










