71 results
Section I - Perioperative Management
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 1-10
-
- Chapter
- Export citation
Section II - Screening, Prevention, and Early Diagnosis
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 11-22
-
- Chapter
- Export citation
Section VI - Vaginal and Vulvar Cancer
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 291-312
-
- Chapter
- Export citation
Section III - Ovarian Cancer
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 23-164
-
- Chapter
- Export citation
Index
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 313-320
-
- Chapter
- Export citation
Contributors
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp xiii-xxiv
-
- Chapter
- Export citation
Contents
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp v-xii
-
- Chapter
- Export citation
Section V - Cervical Cancer
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 253-290
-
- Chapter
- Export citation
Copyright page
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp iv-iv
-
- Chapter
- Export citation
Section IV - Endometrial Cancer
-
- Book:
- 50 Big Debates in Gynecologic Oncology
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023, pp 165-252
-
- Chapter
- Export citation
50 Big Debates in Gynecologic Oncology
-
- Published online:
- 20 July 2023
- Print publication:
- 03 August 2023
Unsupervised neurobiology-driven stratification of clinical heterogeneity in depression
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S614
-
- Article
-
- You have access
- Open access
- Export citation
Structural neuroimaging differentiates between depressed bipolar disorder and major depressive disorder patients: a machine learning study
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S614-S615
-
- Article
-
- You have access
- Open access
- Export citation
Resting State Functional Connectivity is Associated With Treatment Response in Major Depression: A Real World Study
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S606-S607
-
- Article
-
- You have access
- Open access
- Export citation
Identifying a predictive model of cognitive impairment in bipolar disorder patients: a machine learning study
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S612
-
- Article
-
- You have access
- Open access
- Export citation
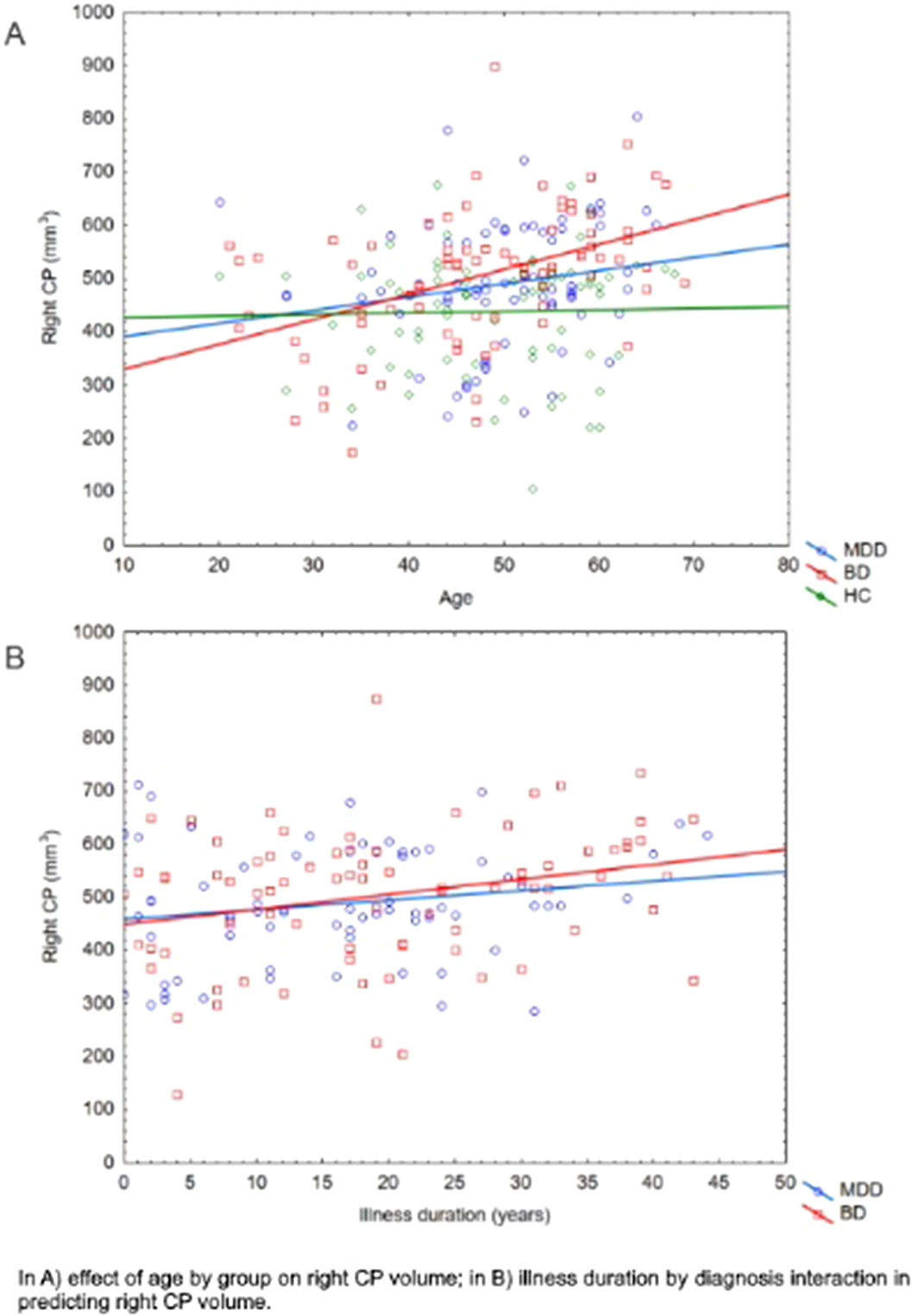
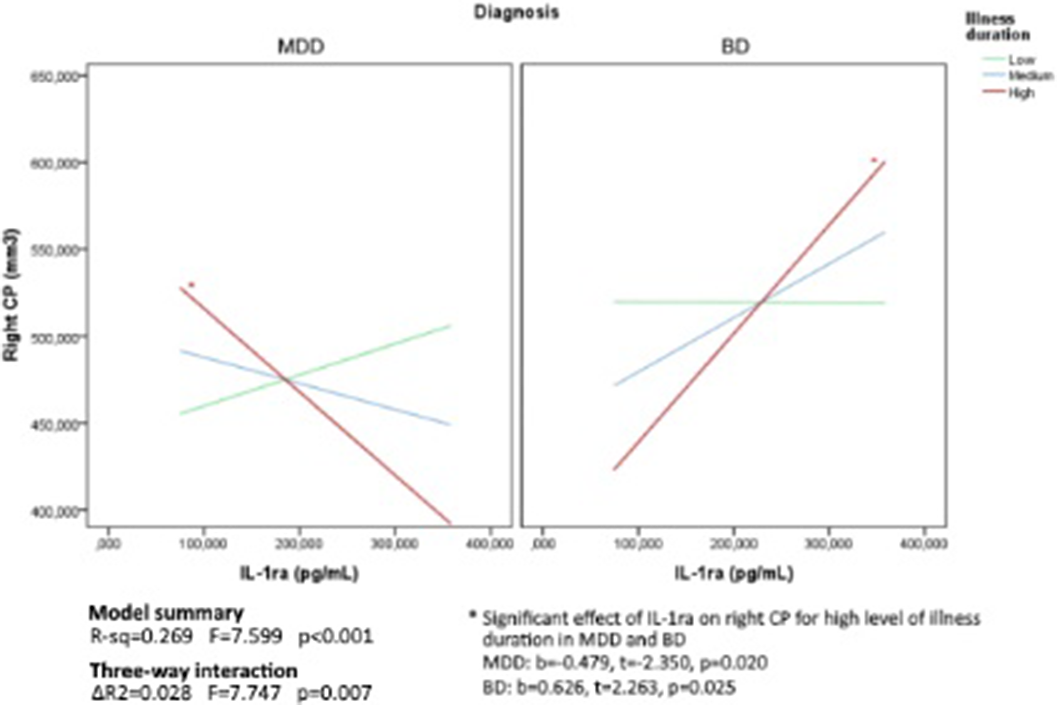
Choroid plexus volume as a proxy of neuroinflammation in depression
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S244-S245
-
- Article
-
- You have access
- Open access
- Export citation
Predicting Suicide Attempts among Major Depressive Disorder Patients with Structural Neuroimaging: A Machine Learning Approach
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1111-S1112
-
- Article
-
- You have access
- Open access
- Export citation
Predicting unipolar and bipolar depression using inflammatory markers, neuroimaging and neuropsychological data: a machine learning study
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S621
-
- Article
-
- You have access
- Open access
- Export citation
CHRONOBIOLOGY IN DIVERGENT THINKING: HOW DESIGNERS ARE AFFECTED BY TIME OF DAY
-
- Journal:
- Proceedings of the Design Society / Volume 3 / July 2023
- Published online by Cambridge University Press:
- 19 June 2023, pp. 887-896
-
- Article
-
- You have access
- Open access
- Export citation
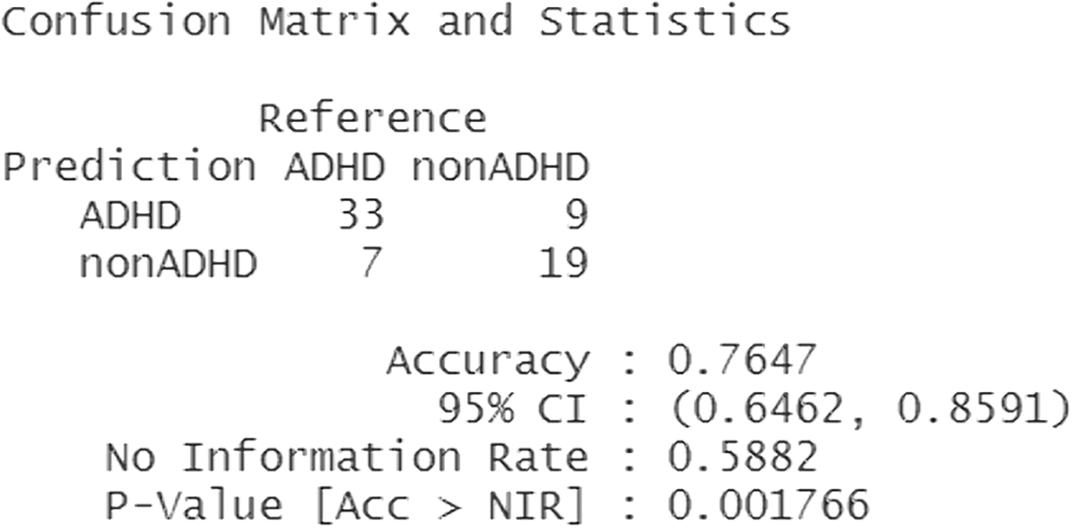
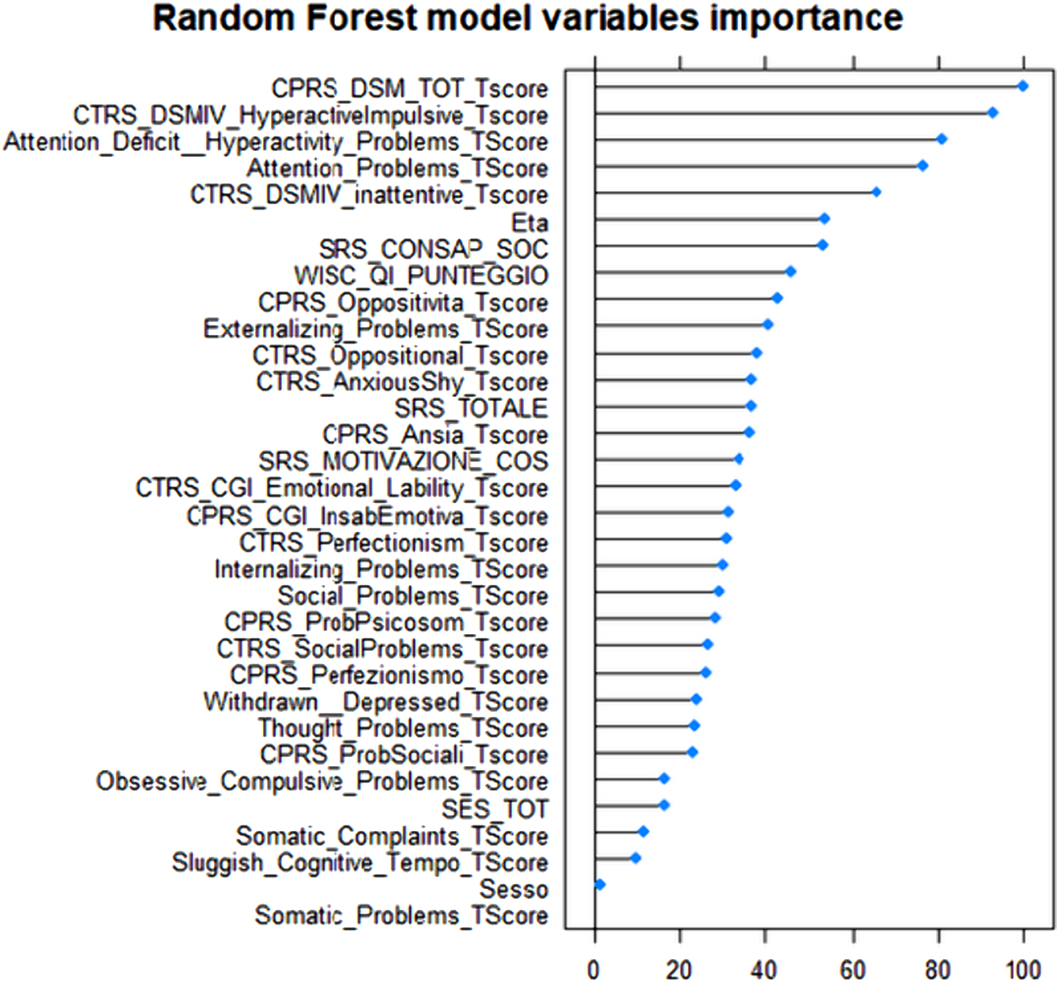
Use of machine learning on clinical questionnaires data to support the diagnostic classification of Attention DeficitHyperactivity Disorder: a personalized medicine approach
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, pp. S165-S166
-
- Article
-
- You have access
- Open access
- Export citation