69 results
Implementing nasal povidone-iodine decolonization to reduce infections in hemodialysis units: a qualitative assessment
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 23 May 2024, pp. 1-6
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Dr. Loreen Herwaldt on research, writing, sabbaticals, and planks
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 4 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 11 March 2024, e30
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Alcohol-based decontamination of gloved hands: A randomized controlled trial
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 4 / April 2024
- Published online by Cambridge University Press:
- 23 November 2023, pp. 467-473
- Print publication:
- April 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Examining barriers to implementing a surgical-site infection bundle
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 1 / January 2024
- Published online by Cambridge University Press:
- 26 July 2023, pp. 13-20
- Print publication:
- January 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Unfamiliar personal protective equipment: The role of routine practice and other factors affecting healthcare personnel doffing strategies
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 12 / December 2023
- Published online by Cambridge University Press:
- 12 April 2023, pp. 1979-1986
- Print publication:
- December 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
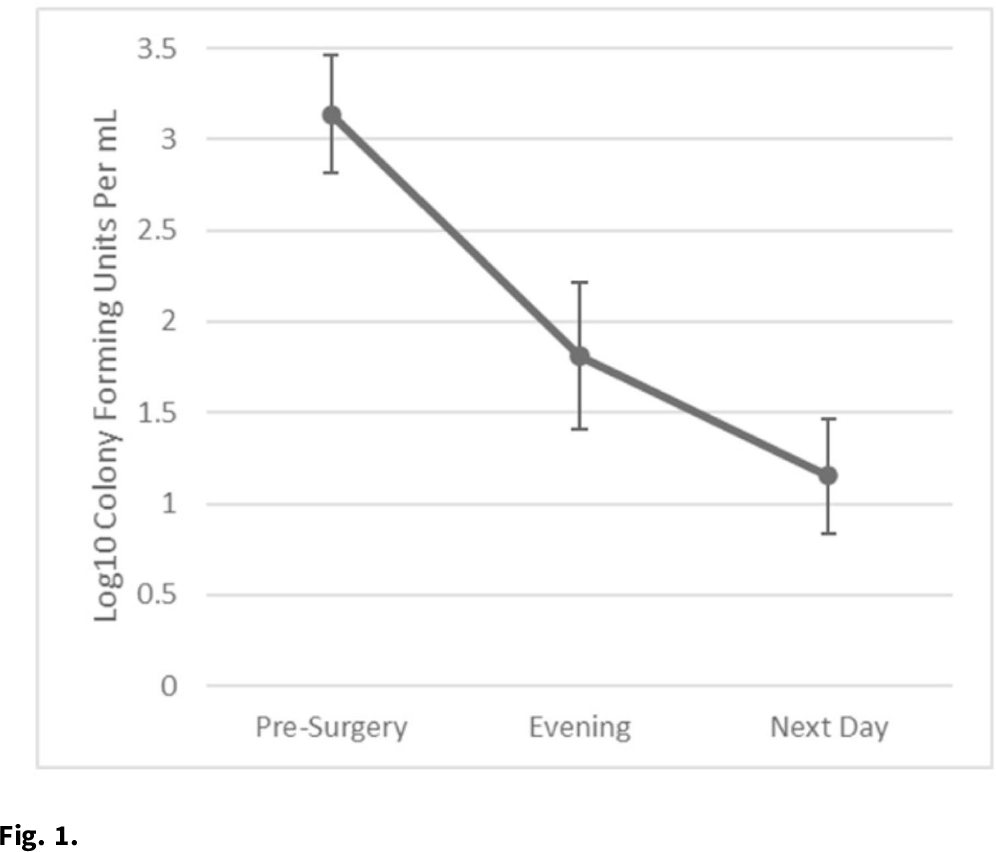
Effectiveness and acceptability of intranasal povidone-iodine decolonization among fracture fixation surgery patients to reduce Staphylococcus aureus nasal colonization
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 6 / June 2023
- Published online by Cambridge University Press:
- 15 June 2022, pp. 982-984
- Print publication:
- June 2023
-
- Article
- Export citation
Feasibility and acceptability of intranasal povidone iodine decolonization among orthopedic trauma surgery patients
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, pp. s62-s63
-
- Article
-
- You have access
- Open access
- Export citation
Implementation of a surgical site infection prevention bundle: Patient adherence and experience
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 1 / Issue 1 / 2021
- Published online by Cambridge University Press:
- 10 December 2021, e63
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The impact of workload on hand hygiene compliance: Is 100% compliance achievable?
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 43 / Issue 9 / September 2022
- Published online by Cambridge University Press:
- 14 May 2021, pp. 1259-1261
- Print publication:
- September 2022
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Hand hygiene and the sequence of patient care
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 43 / Issue 2 / February 2022
- Published online by Cambridge University Press:
- 06 April 2021, pp. 218-223
- Print publication:
- February 2022
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The Role of Routine Practice in Healthcare Worker Strategies when Doffing Unfamiliar Personal Protective Equipment
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 41 / Issue S1 / October 2020
- Published online by Cambridge University Press:
- 02 November 2020, p. s410
- Print publication:
- October 2020
-
- Article
-
- You have access
- Export citation
Self-Contamination While Doffing Personal Protective Equipment
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 41 / Issue S1 / October 2020
- Published online by Cambridge University Press:
- 02 November 2020, pp. s385-s386
- Print publication:
- October 2020
-
- Article
-
- You have access
- Export citation
Impact of 2018 Changes in National Healthcare Safety Network Surveillance for Clostridium difficile Laboratory-Identified Event Reporting
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 39 / Issue 7 / July 2018
- Published online by Cambridge University Press:
- 30 April 2018, pp. 886-888
- Print publication:
- July 2018
-
- Article
-
- You have access
- HTML
- Export citation
Chapter 1 - Ethical Aspects of Infection Prevention
- from Section 1 - Getting Started
-
-
- Book:
- Practical Healthcare Epidemiology
- Published online:
- 02 April 2018
- Print publication:
- 19 April 2018, pp 1-12
-
- Chapter
- Export citation
Chapter 29 - Infection Prevention in Design, Renovation, and Construction
- from Section 6 - Special Topics
-
-
- Book:
- Practical Healthcare Epidemiology
- Published online:
- 02 April 2018
- Print publication:
- 19 April 2018, pp 387-410
-
- Chapter
- Export citation
Research Agenda for Microbiome Based Research for Multidrug-resistant Organism Prevention in the Veterans Health Administration System
- Part of
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 39 / Issue 2 / February 2018
- Published online by Cambridge University Press:
- 08 February 2018, pp. 202-209
- Print publication:
- February 2018
-
- Article
-
- You have access
- HTML
- Export citation
The Iowa Disinfection Cleaning Project: Opportunities, Successes, and Challenges of a Structured Intervention Program in 56 Hospitals
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 38 / Issue 8 / August 2017
- Published online by Cambridge University Press:
- 31 July 2017, pp. 960-965
- Print publication:
- August 2017
-
- Article
- Export citation
Screening Patients Undergoing Total Hip or Knee Arthroplasty with Perioperative Urinalysis and the Effect of a Practice Change on Antimicrobial Use
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 38 / Issue 3 / March 2017
- Published online by Cambridge University Press:
- 21 November 2016, pp. 281-286
- Print publication:
- March 2017
-
- Article
- Export citation
Incidence and Outcomes Associated With Infections Caused by Vancomycin-Resistant Enterococci in the United States: Systematic Literature Review and Meta-Analysis
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 38 / Issue 2 / February 2017
- Published online by Cambridge University Press:
- 09 November 2016, pp. 203-215
- Print publication:
- February 2017
-
- Article
- Export citation
Failure of Risk-Adjustment by Test Method for C. difficile Laboratory-Identified Event Reporting
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 38 / Issue 1 / January 2017
- Published online by Cambridge University Press:
- 17 October 2016, pp. 109-111
- Print publication:
- January 2017
-
- Article
- Export citation