Book contents
- Frontmatter
- Contents
- List of Contributors
- Preface
- Section I Pathophysiology of pediatric liver disease
- Section II Cholestatic liver disease
- Section III Hepatitis and immune disorders
- Section IV Metabolic liver disease
- Chapter 24 Laboratory diagnosis of inborn errors of metabolism
- Chapter 25 α1-Antitrypsin deficiency
- Chapter 26 Cystic fibrosis liver disease
- Chapter 27 Inborn errors of carbohydrate metabolism
- Chapter 28 Copper metabolism and copper storage disorders
- Chapter 29 Iron storage disorders
- Chapter 30 Heme biosynthesis and the porphyrias
- Chapter 31 Tyrosinemia
- Chapter 32 Lysosomal storage disorders
- Chapter 33 Disorders of bile acid synthesis and metabolism
- Chapter 34 Inborn errors of fatty acid oxidation
- Chapter 35 Mitochondrial hepatopathies
- Chapter 36 Non-alcoholic fatty liver disease in children
- Chapter 37 Peroxisomal diseases
- Chapter 38 Urea cycle disorders
- Section V Other considerations and issues in pediatric hepatology
- Index
- References
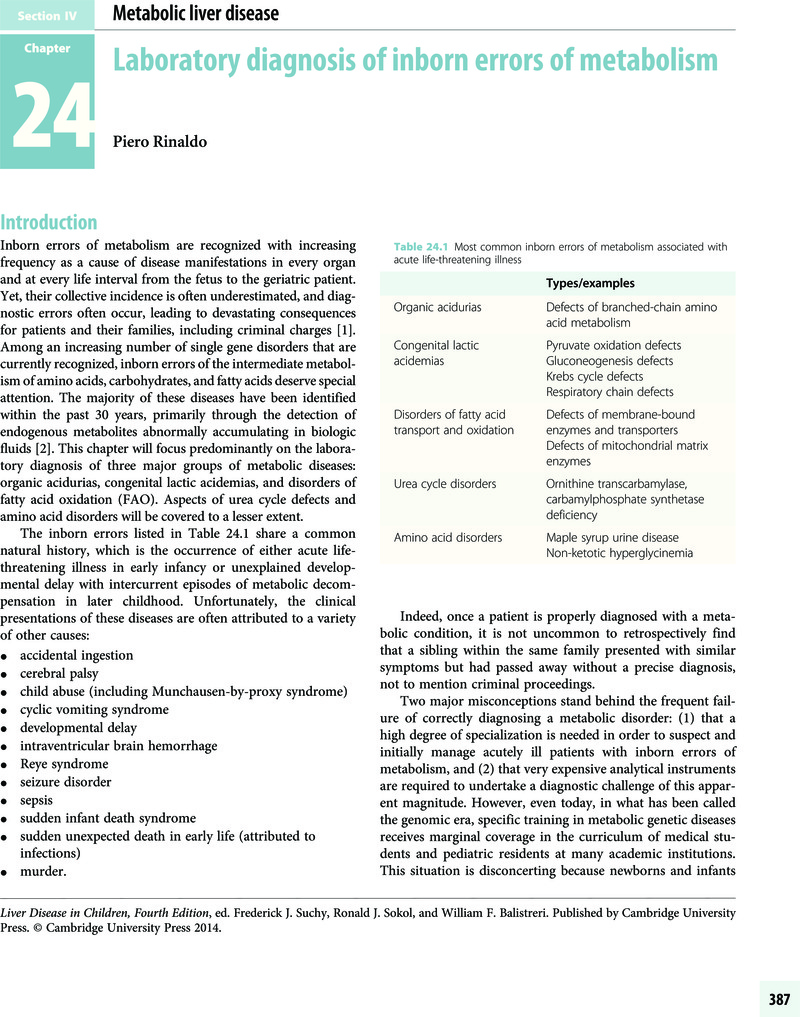
Chapter 24 - Laboratory diagnosis of inborn errors of metabolism
from Section IV - Metabolic liver disease
Published online by Cambridge University Press: 05 March 2014
- Frontmatter
- Contents
- List of Contributors
- Preface
- Section I Pathophysiology of pediatric liver disease
- Section II Cholestatic liver disease
- Section III Hepatitis and immune disorders
- Section IV Metabolic liver disease
- Chapter 24 Laboratory diagnosis of inborn errors of metabolism
- Chapter 25 α1-Antitrypsin deficiency
- Chapter 26 Cystic fibrosis liver disease
- Chapter 27 Inborn errors of carbohydrate metabolism
- Chapter 28 Copper metabolism and copper storage disorders
- Chapter 29 Iron storage disorders
- Chapter 30 Heme biosynthesis and the porphyrias
- Chapter 31 Tyrosinemia
- Chapter 32 Lysosomal storage disorders
- Chapter 33 Disorders of bile acid synthesis and metabolism
- Chapter 34 Inborn errors of fatty acid oxidation
- Chapter 35 Mitochondrial hepatopathies
- Chapter 36 Non-alcoholic fatty liver disease in children
- Chapter 37 Peroxisomal diseases
- Chapter 38 Urea cycle disorders
- Section V Other considerations and issues in pediatric hepatology
- Index
- References
Summary
- Type
- Chapter
- Information
- Liver Disease in Children , pp. 387 - 399Publisher: Cambridge University PressPrint publication year: 2014