Book contents
- Renal Disease in Pregnancy
- Renal Disease in Pregnancy
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 Physiology
- Section 2 Prepregnancy Care
- Section 3 Antenatal Care
- Chapter 5 CKD and Pregnancy
- Chapter 6 Midwifery Issues
- Chapter 7 Drugs in Women with Renal Disease and Transplant Recipients in Pregnancy
- Chapter 8 Management of Hypertension in Renal Disease in Pregnancy
- Section 4 Postpartum
- Section 5 Special Conditions
- Section 6 Acute Kidney Injury
- Appendix: Consensus Statements 2017
- Index
- References
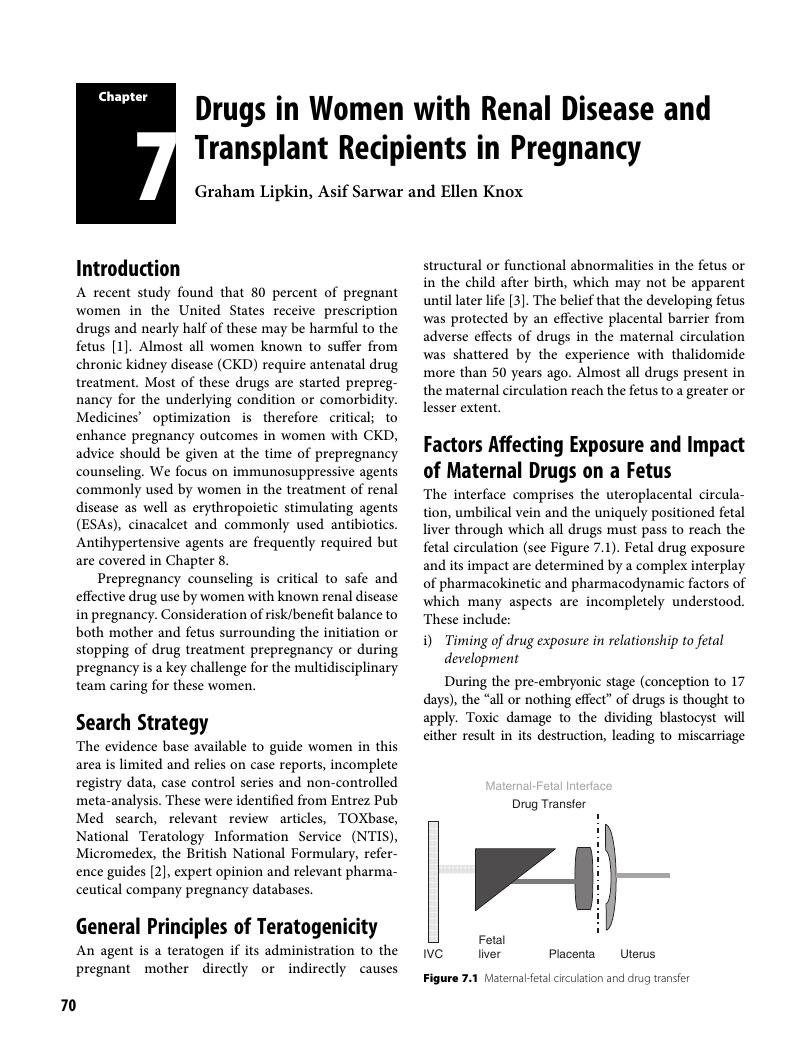
Chapter 7 - Drugs in Women with Renal Disease and Transplant Recipients in Pregnancy
from Section 3 - Antenatal Care
Published online by Cambridge University Press: 19 May 2018
- Renal Disease in Pregnancy
- Renal Disease in Pregnancy
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 Physiology
- Section 2 Prepregnancy Care
- Section 3 Antenatal Care
- Chapter 5 CKD and Pregnancy
- Chapter 6 Midwifery Issues
- Chapter 7 Drugs in Women with Renal Disease and Transplant Recipients in Pregnancy
- Chapter 8 Management of Hypertension in Renal Disease in Pregnancy
- Section 4 Postpartum
- Section 5 Special Conditions
- Section 6 Acute Kidney Injury
- Appendix: Consensus Statements 2017
- Index
- References
Summary
- Type
- Chapter
- Information
- Renal Disease in Pregnancy , pp. 70 - 86Publisher: Cambridge University PressPrint publication year: 2018