Book contents
- Violence in Psychiatry
- Violence in Psychiatry
- Copyright page
- Contents
- Contributors
- Section 1 Statement of the problem
- Section 2 Assessment
- Chapter 3 The evolution of violence risk assessment
- Chapter 4 Assessment of aggression in inpatient settings
- Chapter 5 Clinical assessment of psychotic and mood disorder symptoms for risk of future violence
- Chapter 6 Inpatient aggression in community hospitals
- Chapter 7 Prevalence of physical violence in a forensic psychiatric hospital system during 2011–2013: patient assaults, staff assaults, and repeatedly violent patients
- Chapter 8 The psychiatrist’s duty to protect
- Section 3 Neurobiology
- Section 4 Guidelines
- Section 5 Psychopharmacology
- Section 6 Treatment interventions
- Index
- References
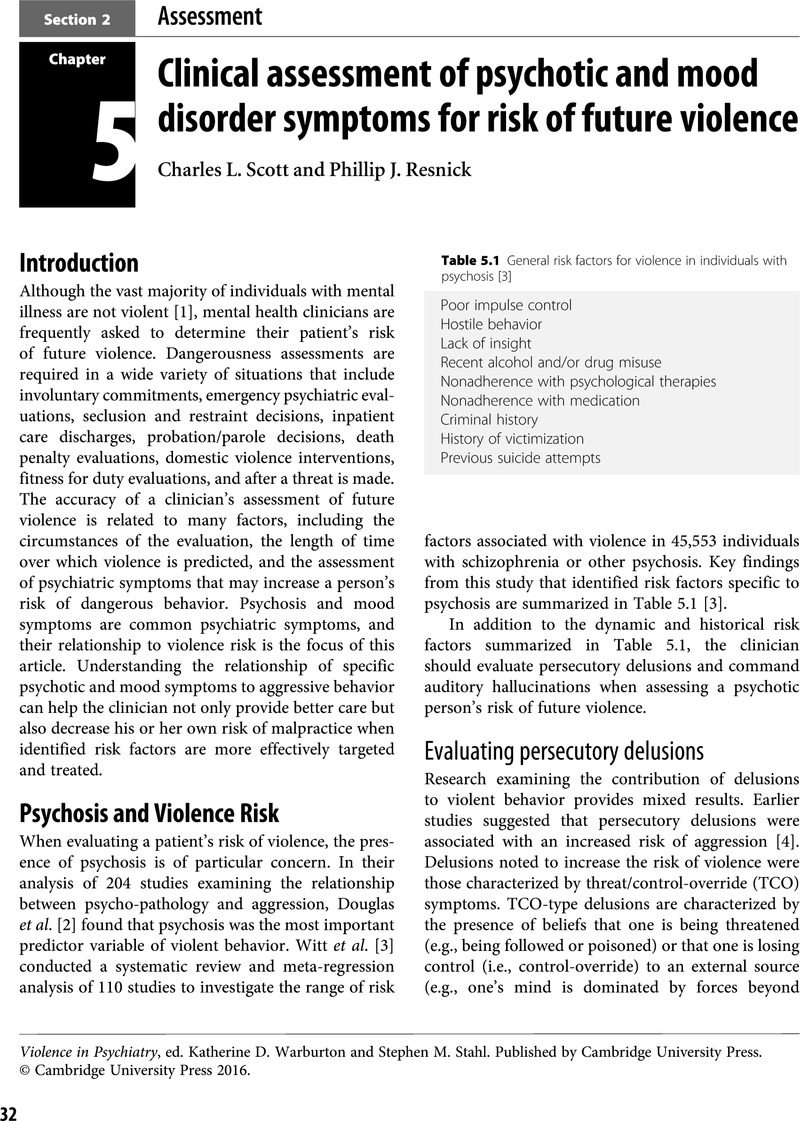
Chapter 5 - Clinical assessment of psychotic and mood disorder symptoms for risk of future violence
from Section 2 - Assessment
Published online by Cambridge University Press: 19 October 2021
- Violence in Psychiatry
- Violence in Psychiatry
- Copyright page
- Contents
- Contributors
- Section 1 Statement of the problem
- Section 2 Assessment
- Chapter 3 The evolution of violence risk assessment
- Chapter 4 Assessment of aggression in inpatient settings
- Chapter 5 Clinical assessment of psychotic and mood disorder symptoms for risk of future violence
- Chapter 6 Inpatient aggression in community hospitals
- Chapter 7 Prevalence of physical violence in a forensic psychiatric hospital system during 2011–2013: patient assaults, staff assaults, and repeatedly violent patients
- Chapter 8 The psychiatrist’s duty to protect
- Section 3 Neurobiology
- Section 4 Guidelines
- Section 5 Psychopharmacology
- Section 6 Treatment interventions
- Index
- References
Summary
- Type
- Chapter
- Information
- Violence in Psychiatry , pp. 32 - 38Publisher: Cambridge University PressPrint publication year: 2016