Book contents
- Basic Physiology for Anaesthetists
- Basic Physiology for Anaesthetists
- Copyright page
- Dedication
- Contents
- Foreword
- Preface to the Second Edition
- Preface to the First Edition
- Abbreviations
- Section 1 The Basics
- Section 2 Respiratory Physiology
- Section 3 Cardiovascular Physiology
- Section 4 Neurophysiology
- Section 5 Gastrointestinal Tract
- Section 6 Kidney and Body Fluids
- Section 7 Blood and Immune System
- Section 8 Energy Balance
- Section 9 Endocrine Physiology
- Section 10 Developmental Physiology
- Section 11 Environmental Physiology
- Index
- References
Section 3 - Cardiovascular Physiology
Published online by Cambridge University Press: 31 July 2019
- Basic Physiology for Anaesthetists
- Basic Physiology for Anaesthetists
- Copyright page
- Dedication
- Contents
- Foreword
- Preface to the Second Edition
- Preface to the First Edition
- Abbreviations
- Section 1 The Basics
- Section 2 Respiratory Physiology
- Section 3 Cardiovascular Physiology
- Section 4 Neurophysiology
- Section 5 Gastrointestinal Tract
- Section 6 Kidney and Body Fluids
- Section 7 Blood and Immune System
- Section 8 Energy Balance
- Section 9 Endocrine Physiology
- Section 10 Developmental Physiology
- Section 11 Environmental Physiology
- Index
- References
Summary
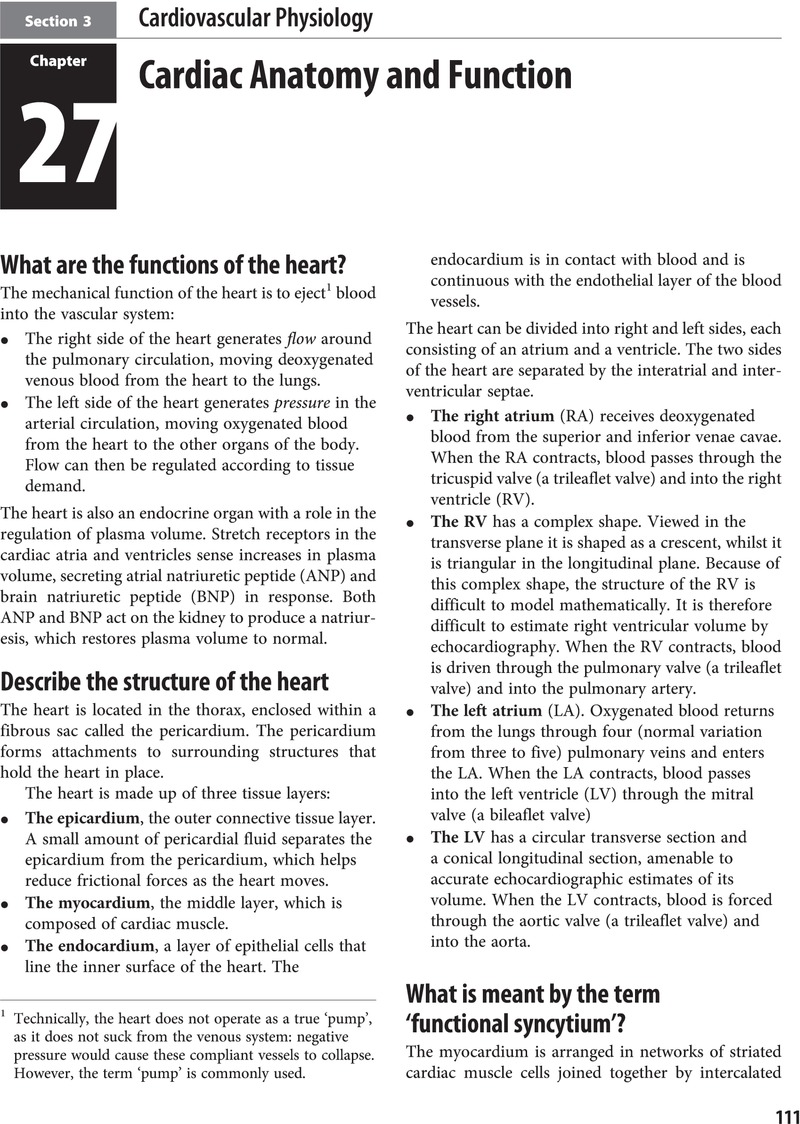
- Type
- Chapter
- Information
- Basic Physiology for Anaesthetists , pp. 111 - 188Publisher: Cambridge University PressPrint publication year: 2019