INTRODUCTION
Gastroenteritis is very common with an estimated 17·2 million [95% confidence interval (CI) 14·5–19·9 million] episodes each year in Australia [Reference Hall1]. Agents causing gastroenteritis may be transmitted by consumption of contaminated food or water, or contact with other infected persons, animals or the environment [Reference Tauxe2]. The incidence of gastroenteritis in Australia (0·83 episodes/person per year) is similar to that reported in other developed countries, such as the USA (0·99), and Canada (0·99) [Reference Scallan3]. In an Australian community survey in 2001–2002, gastroenteritis was more likely to occur in summer and in a person who was: female, a young child, a resident of the warmest state, of higher socioeconomic status, and without health insurance [Reference Hall1]. People aged >70 years reported the lowest incidence of gastroenteritis of any age group [Reference Hall1].
Despite the potential susceptibility of elderly people to gastroenteritis and foodborne diseases, the incidence, risk factors and clinical outcomes have not been well characterized [Reference Roy, Scallan and Beach4, Reference Majowicz5]. In most studies of gastroenteritis, data for older study participants are too sparse to provide meaningful results and, at best, are aggregated to provide incidence for those aged >55 or >65 years [Reference Roy, Scallan and Beach4, Reference Jones6]. In a recent systematic review, the median incidence of diarrhoea in people aged >55 years was highest in the European region at 0·78 episodes/person per year and lowest in the South East Asian region at 0·3 episodes/person per year [Reference Walker and Black7]. Cross-sectional surveys conducted in the USA found that people aged >65 years experienced about 0·3 episodes/person per year [Reference Jones6, Reference Sargeant, Majowicz and Snelgrove8, Reference Thomas9]. By contrast, an intervention study in elderly people in the USA, found that people aged ⩾55 years experienced between 1·69–2·83 episodes/person per year [Reference Colford10], although the case definition was extremely sensitive [Reference Walker and Black7].
As case definition can be very influential on estimates, an international study recommended a standardized definition to improve comparability:
an individual with ⩾3 loose stools, or any vomiting, in 24 h, but excluding those (a) with cancer of the bowel, irritable bowel syndrome, Crohn's disease, ulcerative colitis, cystic fibrosis, coeliac disease, or another chronic illness with symptoms of diarrhoea or vomiting, or (b) who report their symptoms were due to drugs, alcohol, or pregnancy [Reference Majowicz5].
While this definition may be reasonable for the study of gastroenteritis in the general community, it may be inappropriate for the elderly, in whom there is a higher prevalence of some of these chronic diseases. It is possible to have both chronic and acute infectious causes of diarrhoea together and those with an underlying chronic bowel disease may also be more likely to acquire infectious gastroenteritis.
Residents of long-term care facilities (LTCFs) are thought to experience a higher incidence of gastroenteritis due to the commonness of outbreaks in the institutional setting [Reference Jones11]. However, we found in a meta-analysis of prospective surveillance studies that the incidence of gastroenteritis in LTCF residents was about 0·15 episodes/person per year [Reference Kirk12]. In a recent study of 16 Australian LTCFs in 2008, we estimated that the incidence in LTCF residents was 0·23 episodes of diarrhoea/person per year [Reference Kirk13]. In both Australia and overseas, the majority of episodes of gastroenteritis in LTCF residents appears to be related to outbreaks, particularly those caused by viral agents that are easily spread from one person to another [Reference Kirk14–Reference Lopman16].
In this paper, we examine gastroenteritis in the elderly living in the community, by comparing the incidence and identifying differences in clinical illness in the elderly and other adults. We compare the incidence of gastroenteritis and diarrhoea in elderly people living in the community with the Australian LTCF population. Finally, we examine risk factors for gastroenteritis in older Australians, and contrast perceptions about the safety of food and reporting outbreaks between the elderly and other adults.
METHODS
Cross-sectional surveys
Two National Gastroenteritis Surveys (NGSI-2001 and NGSII-2008) have been conducted in Australia. Both were cross-sectional surveys of the Australian community covering all states and territories and were of similar design [Reference Hall1, 17]. NGSI-2001 was conducted from September 2001 to August 2002 and NGSII-2008 was conducted between February 2008 and January 2009.
The study populations for the two surveys were: all Australians living in residential households with fixed telephone lines in 2001–2002 and 2008–2009, respectively. Random digit dialling was used to select a household. The person having the next birthday was selected for interview, which was conducted in one of seven languages. Introductory letters about the surveys were sent where an address was available [Reference Robertson18]. Carergivers answered for children aged ⩽15 years for both surveys. Nine attempts were made to contact the household at different times of the day before moving on to the next selected telephone number.
Computer-assisted telephone interviews (CATI) were conducted using a similar questionnaire for both surveys. All respondents were asked about symptoms of gastroenteritis, healthcare use, impact on daily activities, chronic illness, demographics, and socioeconomic status in the 4 weeks prior to interview.
Definitions
For this study, we modified the symptom-based definition recommended in the international study by Majowicz et al. [Reference Majowicz5]. We defined a case of infectious gastroenteritis as someone who experienced an episode of ⩾3 loose stools and/or ⩾1 episode of vomiting in 24 h, excluding those who reported a self-assessed non-infectious cause of their symptoms. We asked all people reporting diarrhoea and vomiting whether they thought their symptoms were due to a non-infectious cause, such as pregnancy, alcohol, medication use, or a chronic illness with diarrhoea or vomiting as a symptom, such as Crohn's disease or irritable bowel syndrome [Reference Majowicz5, Reference Hall19]. People reporting one of these non-infectious reasons as the cause of their episode of diarrhoea or vomiting were considered non-cases. To compare incidence with elderly people living in a LTCF, we also compared results using a different case definition of diarrhoea, comprising ⩾3 loose stools in 24 h excluding non-infectious causes.
We defined an ‘elderly person’ as someone who was aged ⩾65 years at the time of the survey, while an ‘other adult’ was aged 20–64 years.
Combining surveys and data weighting
The two surveys were combined in order to obtain more precise estimates of the incidence of gastroenteritis and compare findings between elderly people with other adults. Our aim was to estimate the incidence by age group in people aged ⩾65 years, which required a larger sample size than that obtained in a single survey. Prior to combining datasets, we compared data for the two surveys (see online Appendix). We did not use pre-determined criteria for whether the datasets should be combined, but assessed differences in key outcomes, such as the incidence of gastroenteritis by age group, reported symptoms and use of health services.
We adjusted the data to ensure that they were representative of the Australian population accounting for the sample design (stratified by state and territory) and weighted by gender and age group in 10-year age groups up to ⩾80 years. We used 2001 Australian Census data and 2008 population estimates from the Australian Bureau of Statistics (www.abs.gov.au) to weight the data for NGSI-2001 and NGSII-2008, respectively. We subtracted the number of permanent residents (about 150 000) living in LTCFs obtained from the Australian Institute of Health and Welfare (www.aihw.gov.au) from denominator data used to weight survey data, as they were not part of the sampling frame.
Comparing gastroenteritis in the elderly and other adults
We estimated the incidence of gastroenteritis, by extrapolating from the weighted prevalence of any gastroenteritis episode in the 4 weeks prior to the survey to the number of episodes occurring annually. We compared symptoms of illness in elderly cases with other adult cases, by estimating the weighted 4-week prevalence and calculating 95% confidence intervals. Similarly, we compared the use of medication for gastroenteritis, attendance at healthcare facilities and treatment in elderly and other adult cases.
Comparing incidence with LTCF residents
To compare the incidence of diarrhoea (⩾3 loose stools in 24 h) to published results for LTCF residents [Reference Kirk13], we directly standardized data to the age and sex structure of LTCF residents. We used Australian LTCF population for 2008 as the reference population [20].
Risk factors for gastroenteritis
In NGSI-2001, some risk-factor information was elicited in a nested case-control study, where all people reporting any diarrhoea or vomiting and 10 randomly selected controls per case were asked about risk factors for gastroenteritis. In NGSII-2008, all survey respondents were asked about these risk factors. We examined the risk of ⩾65-year-old survey respondents having gastroenteritis in the previous 4 weeks and whether they had eaten in the previous week at various venues, used specific medications or travelled recently. We conducted univariate logistic regression with gastroenteritis as the dependent variable and risk factors as the independent variable. To examine for potential confounding, variables that were significant at P<0·10 were included in a multivariable model that included state in the model to account for the effect of regional stratified sampling and a variable indicating which survey the data originated from. In regression analyses, we did not weight data as in NGSI-2001 controls were a subgroup of the survey sample and the purpose of the analysis was to identify relative odds ratios among risk factors.
Food safety
During the NGSI-2001 survey, respondents were asked about whether they were concerned about the safety of food supply and in the NGSII-2008 survey, respondents were asked about whether they were aware of recent outbreaks and who they would report them to. We compared responses of elderly respondents with those of other adults regarding their concerns about food safety and who they would report outbreaks to.
Statistical analysis and ethical issues
We calculated 95% confidence intervals using standard large sample methods. For comparisons of means and proportions, we calculated t scores and considered differences significant where P<0·05. We conducted all analyses using Stata statistical software (release 11.2, StataCorp, USA). Ethics committees at the Australian National University, Department of Health & Ageing and NSW Cancer Council approved these surveys.
Results
There was a 17·9% decline in participation rate between the two surveys, as 67% (6087/9085) of eligible households contacted agreed to participate in NGSI-2001, compared to 49·1% (7590/15 456) in NGSII-2008. People aged ⩾65 years comprised 18·0% (1095/6087) of survey respondents in NGSI-2001 and 27·4% (2087/7578) in NGSII-2008, which gave a sample size of 3176 elderly respondents available for analysis. Gastroenteritis was more commonly reported across all age groups in NGSI-2001 compared to NGSII-2008 and we did observe some differences in clinical presentation between the two surveys (online Appendix).
Incidence
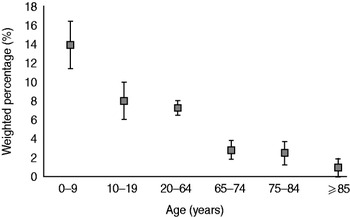
The weighted 4-week prevalence of gastroenteritis in people aged ⩾65 years for the combined surveys was 2·5% (95% CI 1·8–3·3). The incidence of gastroenteritis in elderly people in NGSI-2001 was 0·46 episodes/person per year, compared to 0·22 in NGSII-2008. From analysis of the combined dataset, we estimated that older Australians experience 0·33 (95% CI 0·24–0·42) episodes of gastroenteritis/person per year, equating to 848 000 (95% CI 614 000–1 083 000) cases annually. Other adults aged between 20 and 64 years experienced 0·95 (95% CI 0·74–1·15) episodes/person per year. The incidence of gastroenteritis was lowest in those aged >85 years (0·12 episodes/person per year). People aged <65 years, including children, experienced 1·09 (95% CI 1·00–1·18) episodes/person per year. The incidence of gastroenteritis in survey respondents declined markedly with age (Fig. 1).
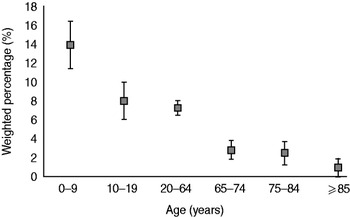
Fig. 1. Weighted percentage of survey respondents reporting gastroenteritis during the 4 weeks prior to interview, by age group, using combined data for 2001–2002, 2008–2009, Australia. Error bars represent 95% confidence intervals around point estimates.
Similarly, elderly people in the surveys experienced 0·27 (95% CI 0·18–0·36) episodes/person per year meeting the alternative case definition based on diarrhoea only, compared to 0·77 (95% CI 0·61–0·93) in other adults. In all survey respondents aged <65 years, including children, the incidence of diarrhoea was 0·77 (95% CI 0·69–0·84) episodes/person per year.
Clinical illness, healthcare use and medication
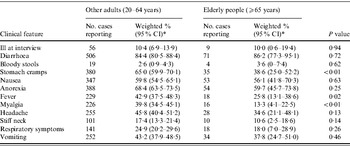
The mean duration of illness in older people was 3.3 days (95% CI 1·2–5·3), compared to 2.2 days (95% CI 1·9–2·6, P=0·58) in other adults. Older people (10·0%) were just as likely as other adults (10·5%) to still have symptoms at the time of interview (Table 1). Among cases of gastroenteritis, elderly people were significantly less likely to report symptoms of stomach cramps (P<0·01), fever (P=0·02), and myalgia (P<0·01) than other adults.
Table 1. Clinical features of people reporting gastroenteritis during the 4 weeks prior to interview compared to other adults (aged 20–64 years) and elderly people (aged ⩾65 years), using combined data for 2001–2002, 2008–2009, Australia
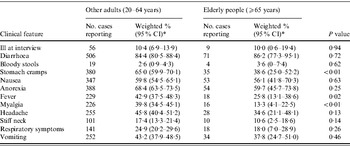
CI, Confidence interval.
* Data weighted for state, age and sex.
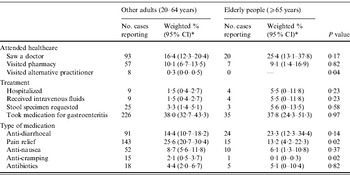
Compared to other adults, elderly people were somewhat more likely to receive healthcare, although this was not statistically significant (Table 2). Approximately, 25·4% of elderly cases visited a doctor, compared to 16·4% of other adults (P=0·17). Similarly, 5·5% of elderly cases were hospitalized compared to 1·5% of other adults (P=0·23), and higher proportions of elderly people received intravenous fluids as treatment and were requested to submit a faecal specimen by a doctor, although these were not significant. Approximately 23·3% of elderly cases used medications specifically for diarrhoea treatment, compared to 14·4% of other adults (P=0·14). Elderly cases were less likely to take medication for pain relief (P=0·02) or nausea (P=0·02) than other adults.
Table 2. Access to healthcare and treatment for people reporting gastroenteritis during the 4 weeks prior to interview compared to other adults (aged 20–64 years) and elderly cases (aged ⩾65 years), using combined data for 2001–2002, 2008–2009, Australia
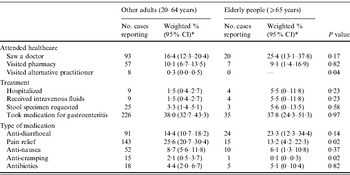
CI, Confidence interval.
* Data weighted for state, age and sex.
Comparison of community and LTCF residents
The age-standardized incidence for elderly people under the alternative definition based on diarrhoea only was 0·15 (95% CI 0·10–0·21) episodes/person per year in the community survey, compared to 0·23 (95% CI 0·11–0·52) in Australian LTCF residents [Reference Kirk13].
Risk factors
In univariable analysis, there was no statistically significant difference in the 4-week prevalence of gastroenteritis in people aged ⩾65 years with regard to gender, household size, health insurance, indigenous status, highest educational level of anyone in the house, season, or whether respondents lived in urban or rural locations (data not shown). Elderly people with a household income between $50 000 and $100 000 experienced significantly less gastroenteritis than people with an income of <$25 000 (P<0·01).
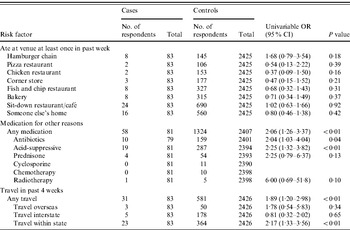
In univariable analysis, people aged ⩾65 years reporting gastroenteritis were more likely to have eaten at a hamburger chain restaurant in the previous week than controls (OR 1·89, 95% CI 0·88–4·06), although this was not statistically significant (Table 3). Case-patients who had travelled in the previous month were more likely to report gastroenteritis (OR 1·97, 95% CI 1·24–3·13), and particularly those who travelled internationally or within the state.
Table 3. Analysis of risk factors for elderly people (⩾65 years old) reporting gastroenteritis during the 4 weeks prior to interview; combined data for 2001–2002, 2008–2009, Australia
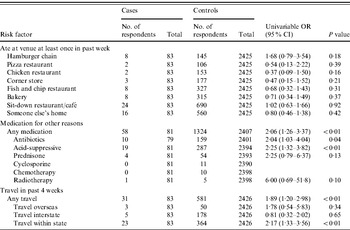
OR, Odds ratio; CI, confidence interval.
In an initial multivariable model, we included variables indicating that cases or controls took acid-suppressive medication, antibiotics, underwent radiotherapy, or travelled within the state; along with design variables for the state of residence and the survey the data were collected in that were held in the model. In multivariable analysis, only travel within the state was significantly associated with gastroenteritis (OR 1·35, 95% CI 1·07–1·71).
Food safety and awareness of outbreaks
In the first survey in 2001–2002, 46% (95% CI 42·5–49·6) of people aged ⩾65 years reported that the safety of food ‘was a serious concern’, compared to 59·0% (95% CI 57·0–61·0, P<0·001) of other adults.
In 2008–2009, 58·0% (95% CI 55·3–60·8) of people aged ⩾65 years indicated they would report an outbreak if they were aware of one, similar to the proportion of other adults who would report an outbreak (54·8%, 95% CI 52·8–56·8, P=0·06). Where elderly people were aware of an outbreak, 79·8% (95% CI 76·9–82·7) would report it to a medical doctor, which was more than for other adults (69·8%, 95% CI 67·2–72·4, P<0·001). Other adults were more likely than elderly people to report an outbreak to the manager of the store where food was purchased (P=0·03), Department of Health (P=0·002), a food safety authority (P=0·007), or a telephone a health advice line (P=0·012).
DISCUSSION
In our analysis of the combined data from two Australian surveys, we observed a markedly lower incidence of self-reported gastroenteritis as age increased. Our findings that people aged ⩾65 years experienced significantly less gastroenteritis than other adults is consistent with cross-sectional surveys conducted in other countries where the lowest incidence of gastroenteritis was in older persons [Reference Scallan3, Reference Jones6, Reference Sargeant, Majowicz and Snelgrove8, Reference Thomas9, Reference Ho21, Reference Majowicz22]. Comparing diarrhoea in elderly people living in the community and LTCFs, the age-standardized incidence of diarrhoea in older Australians dwelling in the community was comparable to that of elderly residents living in LTCFs [Reference Kirk13].
In this study, we modified a case definition that was proposed as an internationally standardized definition. We fully agree that a standardized definition is needed to allow easier comparison between different studies [Reference Majowicz5, Reference Ho21]. However, the international definition suggested excluding people with a wide range of chronic illnesses, such as bowel cancer, Crohn's disease or ulcerative colitis, and therefore they could not be a case regardless of whether a person's enteric symptoms were unrelated to the chronic disease. In our surveys, we asked survey respondents reporting enteric symptoms if they considered their symptoms to be due to a pre-existing chronic illness or if the symptoms were different from usual. If they responded that the symptoms were different from their chronic illness they were still eligible to be included as a case. In elderly populations, a high prevalence of chronic diseases may mean that investigators exclude a high proportion of survey respondents, which may result in distorted and less precise estimates of the incidence of gastroenteritis.
The clinical presentation of people aged ⩾65 years with gastroenteritis showed some differences from other adults, with an illness less likely to exhibit cramps, myalgia and other symptoms. As a consequence, elderly people were less likely to take medication to treat pain or cramping. These differences may reflect a different pattern of pathogens by age groups. One pathogen known as an increasingly common cause of community- and hospital-acquired gastroenteritis in the elderly is Clostridium difficile. C. difficile characteristically causes a diarrhoeal illness with mild abdominal cramping and occasional fever [Reference Bartlett and Gerding23]. There were potential differences between other adults and older people regarding presentation to a doctor for gastroenteritis and submitting a stool specimen, although these were not statistically significant. Older persons were 3–4 times more likely to be hospitalized or receive intravenous fluids, suggesting that elderly people may be more vulnerable to more severe outcomes, particularly following dehydration. A study with increased power may verify these findings.
Our analysis suggests that in people aged ⩾65 years, there was a higher risk of gastroenteritis if they had travelled in the previous month. Cases were also more likely to have eaten at a hamburger restaurant at least once in the previous week, although this was not statistically significant. Both of these behaviours are recognized risk factors for specific enteric infections [Reference Taylor24, Reference McPherson25]. Similarly, in univariable analysis we also identified that elderly people were more likely to report gastroenteritis if they had taken medications, such as antibiotics, acid-suppressive medication, prednisone or were undergoing radiotherapy. Acid-suppressive medications are recognized risk factors for gastrointestinal illness [Reference Tam26–Reference Leonard, Marshall and Moayyedi28]. It is not surprising that we did not identify other risk factors given the small number of cases and the fact that our study was focused on gastroenteritis of unknown aetiology.
It is also possible that elderly people were less likely to report gastroenteritis to survey interviewers compared to other age groups, which may have resulted in an under-estimation of incidence. The reliability of self-reported illness may vary with age, although we are not aware of definitive evidence of this. We observed differences in reporting of information by age, such as who survey respondents would report foodborne illness to if they became aware of an outbreak. Possibly, a higher rate of more serious chronic illness may influence older people about the relative non-importance of gastroenteritis and inhibit reporting.
In this study, we combined two surveys of differing response rate, which may have introduced biases that we were unable to control. In addition, there were declines in the number of households relying on fixed telephone lines in between the two surveys, due to reliance on mobile and internet-based phones that would not be included in the sampling frame of either survey. However, 96% of elderly people had fixed telephone lines in June 2008, which was the highest proportion of any age group [29]. In combining the two surveys, we effectively obtained an average of the incidence of gastroenteritis in elderly people over the two time periods. There were differences in the results of the two surveys, particularly that respondents reported a higher incidence in the first survey, although the declining pattern by age was consistent. There were some clinical differences for people aged ⩾65 years presenting with gastroenteritis in the two surveys, and it is conceivable that different pathogens may have affected people in the two time periods, leading to differing conclusions about how gastroenteritis manifests in the elderly. In fact, incidence can be expected to vary stochastically over time and by estimating a mean over two time periods we accommodated this to some extent.
In conclusion, we estimated that older Australians experience less gastroenteritis than other adults. The incidence we report in people aged ⩾65 years is consistent with what is reported in other surveys internationally [Reference Roy, Scallan and Beach4, Reference Sargeant, Majowicz and Snelgrove8, Reference Majowicz22, Reference Scallan30, Reference Kuusi31]. Gastroenteritis incidence in older Australians living in the community is similar to those living in LTCFs. Although the incidence in elderly people is low, elderly cases experience different symptoms and may be more likely to require hospitalization than younger cases. Elderly people were less concerned about food safety compared to other adults and were more likely to report outbreaks to doctors rather than health departments.
NOTE
Supplementary material accompanies this paper on the Journal's website (http://journals.cambridge.org/hyg).
ACKNOWLEDGEMENTS
M. D. Kirk received a National Health & Medical Research Council Postgraduate scholarship. The Australian Government Department of Health & Ageing provided funding for these surveys under the OzFoodNet programme of work, along with the New South Wales Food Authority.
DECLARATION OF INTEREST
None.