Introduction
Both biological and behavioural differences between men and women affect the development, progression, and management of numerous chronic conditions. Modifiable health risk factors, such as smoking, diet, physical activity, and alcohol consumption contribute to the development of chronic diseases (Ng, Sutradhar, Yao, Wodchis, & Rosella, Reference Ng, Sutradhar, Yao, Wodchis and Rosella2020; Vari et al., Reference Vari, Scazzocchio, D’Amore, Giovannini, Gessani and Masella2016). These health risk factors also contribute to the development of clinical risk factors such as overweight/obesity, high blood pressure, dyslipidemia, and high fasting plasma glucose. Lifestyle recommendations are suggested as the first line of defence for the prevention and management of chronic disease, and include engaging in regular physical activity, maintaining a healthy body weight, consuming a good quality diet, consuming moderate amounts of alcohol, and avoiding smoking (Beasley, Firestone, Popp, Russo, & Yi, Reference Beasley, Firestone, Popp, Russo and Yi2020; Gaudreau et al., Reference Gaudreau, Morais, Shatenstein, Gray-Donald, Khalil and Dionne2007; Puddu & Menotti, Reference Puddu and Menotti2015).
Accumulating literature suggests that risk factors that influence health are sex and gender specific, contributing directly to risk exposure and behaviours (Crimmins, Kim, & Sole-Auro, Reference Crimmins, Kim and Sole-Auro2011; Mauvais-Jarvis et al., Reference Mauvais-Jarvis, Bairey Merz, Barnes, Brinton, Carrero and DeMeo2020; O’Neil, Scovelle, Milner, & Kavanagh, Reference O’Neil, Scovelle, Milner and Kavanagh2018; Regitz-Zagrosek, Reference Regitz-Zagrosek2012; Vari et al., Reference Vari, Scazzocchio, D’Amore, Giovannini, Gessani and Masella2016). For example, men are more likely to smoke (Crimmins et al., Reference Crimmins, Kim and Sole-Auro2011) and women are more likely to engage in healthier dietary habits, including higher consumption of fruit and vegetables, and lower frequency of snacking and alcohol consumption (Vari et al., Reference Vari, Scazzocchio, D’Amore, Giovannini, Gessani and Masella2016). Crimmins et al. (Reference Crimmins, Kim and Sole-Auro2011) examined health differences in individuals 50 years of age and older across 13 different countries, and found that overall, women were more likely than men to report arthritis, depressive symptoms, and hypertension, and less likely to be current smokers, be overweight, or report heart disease. More recently, the influence of age and stage of life on health risk factors has come to light (Dash, Hoare, Varsamis, Jennings, & Kingwell, Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019; Hoare, Dash, Jennings, & Kingwell, Reference Hoare, Dash, Jennings and Kingwell2018). Data from the Australian Health Survey indicate distinct patterns for fruit and vegetable consumption, sugar-sweetened beverage intake, the prevalence of overweight/obesity, and level of physical activity among younger (25–51 years of age) compared with older adults (≥ 65 years of age) (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019). Applying a lifespan approach to research on risk factors for chronic disease has the potential to provide additional insight into the causes of health problems, while also identifying important patterns within different age groups and those that cut across all age groups (Hankivsky, Reference Hankivsky, Morrow, Hankivsky and Varcoe2007). This type of information may also identify sex-specific key times of life where health intervention or health policies may be most beneficial. A sex-specific lifespan approach is necessary to consider how risk factors for chronic disease change over time; however, this approach is lacking from the existing literature and detailed data on age- and sex-specific modifiable risk factors reported for other countries is limited.
Most concerning is the recent data providing evidence for the strong relationship between mortality and various modifiable risk factors (Alam et al., Reference Alam, Lang, Drucker, Gotay, Kozloff and Mate2019; Danaei et al., Reference Danaei, Ding, Mozaffarian, Taylor, Rehm and Murray2009; Global Burden of Disease Study, 2017 Risk Factor Collaborators, 2018). The top risk factors contributing to the burden of disease were recently identified as hypertension, smoking, plasma glucose, and a high body mass index (BMI) (Global Burden of Disease Study, 2017 Risk Factor Collaborators, 2018). Regional analysis has identified smoking and diet as the top health risk factors contributing to disease in Canada (Alam et al., Reference Alam, Lang, Drucker, Gotay, Kozloff and Mate2019). However, more research is needed to understand how risk factors differ by sex and age. Identifying sex- and age-specific differences in risk behaviours offers an opportunity for the development of health promotion programs tailored to specific groups of individuals to reduce the burden of disease in Canada. Therefore, this study aimed to identify the sex differences in risk factors for chronic diseases in a Canadian cohort during younger (30–46), middle (47–56) and older (57–74) adulthood.
Methods
Ethics
Research Ethics Boards in each Atlantic Canada province (Nova Scotia, New Brunswick, Newfoundland and Labrador, and Prince Edward Island) approved the original data collection procedures.
Study Design and Participants
Participants were part of the Atlantic Partnership for Tomorrow’s Health (PATH) study, which is a regional cohort of the Canadian Partnership for Tomorrow’s Health (CanPath, formerly named the Canadian Partnership for Tomorrow Project), a pan-Canadian longitudinal study examining the role of genetic, environmental, behavioural, and lifestyle factors in the development of chronic diseases. Details on recruitment and data collection have been previously described (Dummer et al., Reference Dummer, Awadalla, Boileau, Craig, Fortier and Goel2018; Sweeney et al., Reference Sweeney, Cui, DeClercq, Devichand, Forbes and Grandy2017). The Atlantic PATH cohort includes 34,169 participants who completed baseline questionnaires between 2009 and 2015. The questionnaires included information about health, lifestyle behaviours, medical history, family health history, and demographic information. Additionally, physical measurements (height, weight, waist and hip circumference, body composition, and blood pressure) were collected on a subset of participants. The Global Burden of Disease Study (GBD) has identified modifiable behavioural risk factors such as tobacco and alcohol use, poor dietary habits, and low physical activity, as well as metabolic risk factors such as high blood pressure, overweight/obesity, hyperglycemia, and hyperlipidemia that are attributable to disease burden for males and females (Global Burden of Disease Study, 2017 Risk Factor Collaborators, 2018). In the Atlantic PATH cohort, data were collected on some of these modifiable and metabolic risk factors such as tobacco, alcohol, diet, physical activity, and overweight/obesity. The current study is a cross-sectional analysis of participants with baseline data on the above-mentioned risk factors, resulting in 16167 total participants. The social and demographic characteristics of the included and excluded participants are found in Supplementary Table S1.
Demographic and Health Conditions
The Atlantic PATH cohort includes participants 30–74 years of age. To explore differences across adulthood, age categories were created based on the age tertiles of participants within the cohort. The tertiles were categorized as younger (30–46 years), middle (47–56 years), and older (57–74 years) adults. Participants reported their level of education, household income, working status, and marital status. Participants reported physician-diagnosed conditions of high blood pressure, myocardial infarction, stroke, asthma, chronic obstructive pulmonary disease, diabetes, liver cirrhosis, chronic hepatitis, Crohn’s disease, ulcerative colitis, irritable bowel syndrome, eczema, lupus, psoriasis, multiple sclerosis, osteoporosis, arthritis, and cancer.
Health Risk Factors
The health risk factors of interest were BMI, abdominal obesity, physical activity, smoking status, alcohol consumption, and dietary intake of major food groups. For smoking behaviour, participants were categorized as a current smoker (1 cigarette daily or occasionally in the past 30 days), former smoker (ever smoked at least 100 cigarettes, but not in the last 30 days), and never smoked (< 100 cigarettes ever). For alcohol consumption, participants were classified as an abstainer (never), seldom drinker (< 1/month), occasional drinker (1–3 times/month), regular drinker (1–3 times/week), and habitual drinker (4–7 times/week).
A dietary screener questionnaire was used to assess dietary intake over the past 12 months. Dietary questions were modified from the Canadian Diet History Questionnaire (CDHQ-1) and the Physical Activity and Nutrition Survey (PANS) V2. The questions included the number of typical daily servings of fruit, vegetables, grains, and proteins, as well as the frequency of highly processed foods, fast food, desserts, snack foods, and added salt (choosing rarely/never, servings per day, servings per week, or servings per day) (DeClercq et al., Reference DeClercq, Cui, Forbes, Grandy, Keats and Parker2017). Physical activity level was assessed using the International Physical Activity Questionnaire (IPAQ). Metabolic equivalents of a task were calculated for each participant and level of physical activity was classified as low/inactive, moderate, and high (Keats et al., Reference Keats, Cui, DeClercq, Dummer, Forbes and Grandy2017).
Height, weight, hip, and waist circumferences were measured by trained personnel in assessment centres or self-reported. Only when measured variables were unavailable were self-reported anthropometric data used to calculate abdominal obesity and BMI (approximately 67% of participants in the current study have a measured waist circumference and 68% have a measured BMI value). Differences in measured and self-reported anthropometric indices and the associations between sex and these indices can be found in the Supplementary Materials (Supplementary Tables S2 and S3). Participants with a BMI of < 18.5, 18.5–24.9, 25.0–29.9, and ≥30.0 were considered underweight, normal weight, overweight, and obese, respectively. Abdominal obesity was defined as having a waist circumference ≥ 102 cm for men and ≥ 88 cm for women. Percent body fat was assessed by bioelectrical impedance (Tanita Segmental Body Composition Analyzer).
Statistical Analysis
IBM SPSS Statistics (version 25) software was used for all statistical analyses. Frequencies and proportions were calculated and presented for each sex and age category. Significant associations between age and demographic and health risk factors were determined by chi-square analysis. Continuous variables were presented as median ± interquartile range (IQR) and significant differences across age categories were analyzed using the Kruskal–Wallis test. Multivariable logistic regression models were used to evaluate the relationship among health risk factors, age, and sex (male = 1, female = 2). All lifestyle variables were examined in the same regression model. All models were adjusted for education, income, work, and marital status to account for socioeconomic inequalities (Choi & Marks, Reference Choi and Marks2011; Hazel & Kleyman, Reference Hazel and Kleyman2019). The age-specific associations between sex and health risk factors are presented by odds ratios (OR) with 95 per cent confidence intervals (95% CIs). All data were considered statistically significant at p < 0.05.
Results
Demographic Details across Age Groups
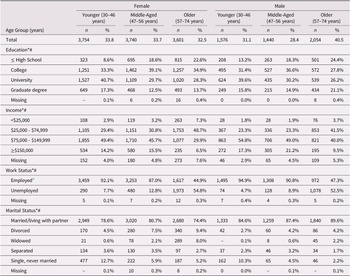
The mean age of participants was 39 years in the younger adult group (n = 5330), 52 years in the middle age group (n = 5,180), and 62 in the older adult group (n = 5,655). Demographic factors by sex and age group are reported in Table 1.
Table 1. Social and demographic characteristics of younger (30–46), middle-aged (47–56), and older (57–74) female and male participants

Note. *Significant association in females (p < 0.05); #Significant association in males (p < 0.05);
a Employed full or part-time.
–Data suppressed because of small cell counts.
Chronic Disease across Sex and Age Groups
The prevalence of chronic conditions in females and males differed across the age groups (see Figure 1). In younger females (30–46 years), the top three most prevalent conditions were eczema, asthma, and irritable bowel syndrome, whereas in older females (57–74 years) the top three most prevalent conditions were arthritis, high blood pressure, and cancer. In younger males, the top three most prevalent conditions were high blood pressure, asthma, and eczema. Similar to older women, the top three most prevalent conditions in older men were high blood pressure, arthritis, and cancer.

Figure 1. Chronic disease in female and male participants by age group. Prevalence (%) of chronic disease in younger (A), middle-aged (B), and older (C) adults.
The frequency of high blood pressure, diabetes, arthritis, and cancer increased across age groups in both females and males, whereas the prevalence of asthma and eczema decreased. Across all age groups, multi-morbidity was higher in females than males, but most striking was the difference in the older adults, where less than 40 per cent of males and nearly 50 per cent of females reported being diagnosed with two or more chronic conditions.
Health Risk Factors of Chronic Disease across Sex and Age Groups
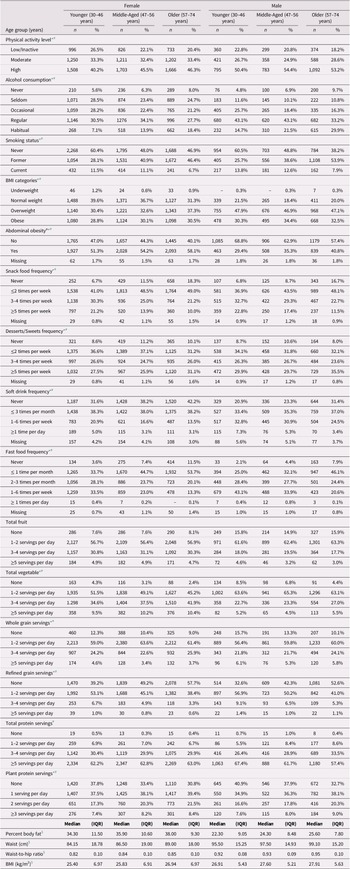
There are many health risk factors associated with the various chronic diseases listed; therefore, we explored several lifestyle and metabolic risk factors across sex and age groups (Table 2). The proportion of participants considered inactive decreased with age in both females and males, meaning more older adults overall were engaging in moderate to high levels of activity, but a greater proportion of men of all ages were engaging in a high level of activity. A greater proportion of males reported habitual consumption of alcohol compared to females, although habitual consumption across the age groups increased by 11 per cent and 15 per cent in females and males, respectively. Overall, the proportion of current smokers decreased across age groups, and a similar proportion of younger and middle-aged adults had never smoked, but more older females (47%) than older males (38%) had never smoked. A large proportion of females had a normal BMI; however, the proportion of those overweight/obese increased with age whereas the BMI for males appeared much more similar across the age groups. More pronounced was the increase in abdominal obesity across the age groups in both females and males, with 58 per cent of older females and 41 per cent of older males having abdominal obesity.
Table 2. Health risk factors across age groups of female and male participants

Note. aAbdominal obesity = waist circumference ≥ 88 cm for females and ≥ 102 cm for males.
* Significant association in females (p < 0.05).
# Significant association in males (p < 0.05).
$ Significant differences (Kruskal–Wallis Test p < 0.05).
–Data suppressed because of small cell counts.
BMI = body mass index; IQR = interquartile range.
Snack food frequency (≥ 3 times per week), soft drink frequency (≥ 1 time per week), and fast food frequency (≥ 1 time per week) all decreased whereas dessert/sweets frequency (≥ 3 times per week) increased across age groups in both males and females. The proportion of males consuming soft drinks and fast food one or more times per week was much greater than for females in all age groups. The proportion of females and males consuming fruit across the age groups was similar, with both consuming fewer servings of fruit than vegetables per day. The consumption of three or more servings of vegetables per day increased across age in both females and males. There was a small increase in daily whole grain consumption and a drastic reduction in daily refined grains consumption across age groups in both females and males. In females, total servings of protein per day were similar across age groups but differed in males, and in both sexes, there was an increase in consumption of plant-based proteins across age groups (67–69% of older adults were consuming plant-based proteins daily).
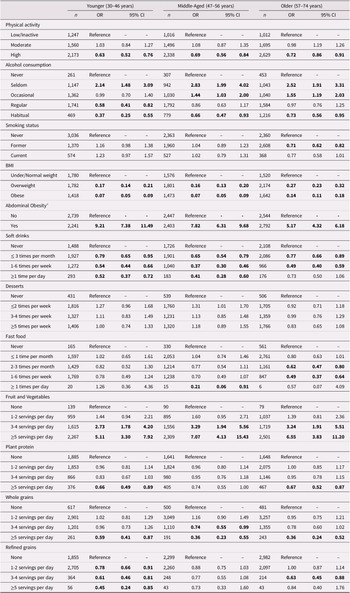
Sex-specific Association among Health Risk Factors across Age Groups
Using regression models that controlled for covariates such as education, income, work, and marital status, several of the health risk factors were found to be significantly different for females than for males (Table 3). Compared with low/inactive participants, the odds of engaging in high levels of physical activity were between 28 and 37 per cent lower for females than for males. Compared with those who never consume alcohol, the odds of habitually consuming alcohol were between 27 and 63 per cent lower for females of all ages than for males, whereas the odds of consuming alcohol seldom is nearly three times higher for middle and older females than for males. Compared with those who never smoked, the odds of being a former smoker were 29 per cent lower for older females than for older males. Compared with being under/normal weight, the odds of being overweight and obese were 73–84 per cent and 86–93 per cent lower for females than for males, whereas the odds of abdominal obesity were five to nine times higher for females of all ages than for males.
Table 3. Age stratified association between sex and health behaviours

Note. Bold font indicates significant at p < 0.05. The reference category for the outcome variable is “male”. All ORs are adjusted for education, income, work, and marital status.
a Waist circumference ≥ 88 cm for females and ≥ 102 cm for males.
OR = odds ratios; 95% CI = 95% confidence interval.
Compared with those who never consumed foods with added sugar such as soft drinks and desserts, the odds of consuming soft drinks up to six times per week were 21–63 per cent lower for females of all ages than for males; there was no difference in dessert consumption between females and males. The frequency of fast food consumption up to six times per week was similar between younger and middle-aged females and males; however, compared with those who never ate fast food, the odds of consuming fast food between twice a month and six times per week was 38–51 per cent lower for older females than for older males. Compared with individuals consuming no servings of fruit/vegetables, the odd of consuming five or more servings per day was five to seven times higher for females of all ages than for males. In contrast, the odds of consuming five or more servings of whole grains per day compared with consuming none, were between 41 and 61 per cent lower for females of all ages than for males. Compared with consuming no refined grains, the odds of consuming one or more servings per day was between 22 and 55 per cent lower for young females than for younger males but was similar in the middle age group. Compared with consuming no plant protein, the odds of consuming up to four servings per day were similar between females and males; however, compared with those who never consumed plant proteins, the odds of consuming five or more servings per day were 33–34 per cent less for younger and older females than for males in the same age groups.
Discussion
This study examines aging Canadians living in a region of the country with particularly high rates of chronic disease, and highlights important age and sex differences in health risk factors. These findings are consistent with national health and dietary surveys from the United States and Australia (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019; Ford, Zhao, Tsai, & Li, Reference Ford, Zhao, Tsai and Li2011). In addition, the inclusion of age categories allowed for a more in-depth and thoughtful analysis that demonstrated differences across the lifespan. This allows for the recognition that not all risk factors are present in all populations (Olivares et al., Reference Olivares, Chambi, Chani, Craig, Pacheco and Pacheco2017). For example, those in mid-life are at a greater risk of developing chronic disease and frailty than are younger populations (DeClercq, Duhamel, Theou, & Kehler, Reference DeClercq, Duhamel, Theou and Kehler2020; Kelly et al., Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016). This also allows for understanding that decisions related to behavioural health risk factors may be directly influenced by factors such as gender and age, which can provide insight into chronic disease outcomes and inform health promotion and intervention initiatives (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019; Kelly et al., Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016). The addition of risk factors for specific populations has direct implications for surveillance for improving health interventions and the implementation of effective prevention strategies (Olivares et al., Reference Olivares, Chambi, Chani, Craig, Pacheco and Pacheco2017). Current Canadian policies and guidelines for modifiable risk factors for adults do not distinguish among age categories. The findings of this research clearly demonstrate that public health efforts that target all adults (18 years of age and older) as a single homogeneous group do not adequately meet the needs of a diverse population.
Although there is limited literature examining behavioural and metabolic health risk factors for chronic disease using a lifespan approach among males and females, our results support the recently published research from the Australian Health Survey, which also utilized three age categories (21–51, 52–64, and ≥ 65) (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019). The Australian Health Survey found that there were differences in adherence to lifestyle behaviours that are protective against the risk of chronic disease between sexes and across age categories (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019). Likewise, the engagement of Atlantic PATH participants in protective health behaviours varied across age categories (e.g., smoking status or fast food frequency) and between sexes (e.g., consumption of alcohol or fruit/vegetables).
Similar to the Australian Health Survey, we found that females had lower levels of physical activity. However, we observed that the overall activity levels of females and males increased with age, whereas the Australian study showed fewer adults meeting physical activity guidelines with age (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019). It is worth noting differences in the age groups and methods of recruitment between the two studies. Nevertheless, differences among countries or within specific regions deserve particular attention for public health and policy development. For example, physical activity levels differ across regions in Canada, with the west coast reporting some of the highest levels of activity. The lowest levels of activity are found on the east coast, including the Atlantic PATH population (Dummer et al., Reference Dummer, Awadalla, Boileau, Craig, Fortier and Goel2018).
Whereas smoking rates among Atlantic PATH participants declined with age, Alam et al. (Reference Alam, Lang, Drucker, Gotay, Kozloff and Mate2019) demonstrate that overall smoking remains a primary risk factor for disease burden in Canada. Another recent Canadian study found that current heavy smokers had an increased risk of chronic disease, and that former heavy smokers had a greater risk than former light smokers (Ng et al., Reference Ng, Sutradhar, Yao, Wodchis and Rosella2020). Specifically, there was an association between current smoking and chronic obstructive respiratory disease, diabetes, lung cancer, myocardial infarction, and stroke among females and an association between current smoking and chronic obstructive respiratory disease, myocardial infarction, and lung cancer among males (Ng et al., Reference Ng, Sutradhar, Yao, Wodchis and Rosella2020).
There were noteworthy findings related to the frequency of alcohol consumption across age groups among Atlantic PATH participants. Whereas younger and middle-aged females were less likely overall to habitually consume alcohol, the frequency of both female and male participants consuming alcohol four or more times a week increased as participants aged. The number of drinks consumed should be examined, as well as the social context of consuming alcohol, because it is well established that the frequency of alcohol consumption with age increases the risk of several chronic diseases (Fernandez-Sola, Reference Fernandez-Sola2015; Rehm et al., Reference Rehm, Gmel GE, Gmel, Hasan, Imtiaz and Popova2017; Shield, Parry, & Rehm, Reference Shield, Parry and Rehm2013; Smyth et al., Reference Smyth, Teo, Rangarajan, O’Donnell, Zhang and Rana2015), whereas in some situations consuming alcohol may offer social benefits (Dare, Wilkinson, Allsop, Waters, & McHale, Reference Dare, Wilkinson, Allsop, Waters and McHale2014; Public Health Agency of Canada, 2016). A community-based longitudinal survey by Moos, Schutte, Brennan, and Moos (Reference Moos, Schutte, Brennan and Moos2009) in the United States found that habitual drinking among older adults declined over a 20-year period, as adults entered their seventies and eighties (baseline 55–65 years). However, they also found that among adults 75–85 years of age, more than one quarter of women and nearly half of men were consuming more than two drinks per day. The rates of alcohol consumption among Atlantic PATH participants were also highest among older adults, and among older males in particular. These findings highlight the role that alcohol consumption plays in an aging population, and support recommendations that alcohol guidelines and policies for older adult men should not be set higher than those for women (Moos et al., Reference Moos, Schutte, Brennan and Moos2009).
The analysis by age also allowed for some interesting insights into the dietary choices of participants. Health Canada’s newly published Dietary Guidelines for Health Professionals and Policy Makers represent a shift away from a focus on the number of servings eaten, and towards more generalized recommendations on food choices and eating habits. Although the complete version of Canada’s Food Guide has not yet been published, there is a clear emphasis on limiting processed foods that contain excess sodium, sugars, or saturated fats and towards the consumption of plant-based foods including vegetables, fruit, whole grains, and plant-based proteins in order to prevent chronic disease. Interestingly, whereas studies such as the National Health and Nutrition Examination Survey have found that adults eat less protein as they age and are less likely to consume plant-based proteins (Beasley et al., Reference Beasley, Firestone, Popp, Russo and Yi2020), we found that protein consumption increased as females aged and that plant-based protein consumption increased across all age groups. Some participants were consuming foods that align with the new Canadian guidelines. Consistent with the literature, overall, more females than males engaged in healthier dietary choices (Grzymislawska, Puch, Zawada, & Grzymislawski, Reference Grzymislawska, Puch, Zawada and Grzymislawski2020; Vari et al., Reference Vari, Scazzocchio, D’Amore, Giovannini, Gessani and Masella2016). Also similar to the findings of the Australian Health Survey, we found that more adults consumed fruit and vegetables as they aged, with more females doing this than males suggesting that female participants are continuing to choose healthier dietary choices as they age (Dash et al., Reference Dash, Hoare, Varsamis, Jennings and Kingwell2019).
Although older adults had a higher frequency of desserts/sweets consumption, younger adults reported a higher frequency of consuming snack foods, fast food, and soft drinks which may reflect a generational divide in snack/dessert preferences. The highest rates of sugar-sweetened beverage consumption occurred in the younger age category and decreased with age, which is also in line with the Australian findings. For example, the greatest proportion of participants consuming soft drinks at least once per week were the younger groups, whereas a larger proportion of participants in the older age group reported never consuming soft drinks in the current study. However, across all ages, weekly consumption was higher for males than for females. Sugar-sweetened beverages, including the soft drinks examined in this study, are a well-established source of caloric sweeteners linked to increased risk of chronic disease, including obesity, hypertension, type 2 diabetes, and coronary heart disease (Hu & Malik, Reference Hu and Malik2010; Malik & Hu, Reference Malik and Hu2019; Schwingshackl et al., Reference Schwingshackl, Schwedhelm, Hoffmann, Knuppel, Iqbal and Andriolo2017). Most recently, findings from the French NutriNet Sante cohort demonstrated a positive association with sugar-sweetened beverages and overall cancer risk and breast cancer risk, warranting additional exploration in this area (Chazelas et al., Reference Chazelas, Srour, Desmetz, Kesse-Guyot, Julia and Deschamps2019).
The Australian Health Survey reported on combined overweight and obesity categories. When combining the overweight and obese categories in Atlantic PATH, our data were higher in each of the three age categories, although the age range between the two studies differs slightly. The value found in separating the overweight and obesity categories in these data is best reflected in our female participants. Whereas the obesity rates remain relatively stable among the three age groups, there is a notable increase in female participants who are overweight as they age. This is particularly striking when coupled with the increased abdominal obesity as participants age, despite engaging in positive health behaviours, such as diet and physical activity. The rates of obesity and abdominal obesity among female participants place them at an increased risk for several chronic diseases as they age, including high blood pressure, diabetes, and cancer (Folsom et al., Reference Folsom, Kushi, Anderson, Mink, Olson and Hong2000).
The behavioural health risk factors examined are reflected in the high rates of chronic disease and multi-morbidity in Atlantic Canada and among the Atlantic PATH population (Keats et al., Reference Keats, Cui, DeClercq, Dummer, Forbes and Grandy2017). Whereas the prevalence of high blood pressure was higher in male participants across all three age groups, the prevalence of asthma, irritable bowel syndrome, and arthritis was higher across all ages in females. The most striking difference in prevalent chronic conditions was found in participants with arthritis. Given the high rates of multi-morbidity in this cohort, females with arthritis are likely living with multiple chronic conditions, further impacting their quality of life.
Many educational campaigns on risk behaviours and the prevention of chronic disease are implemented by national governments, charities, and non-profit organizations, and those that are local are supported by data and messaging from the national level. The findings of this research from Atlantic Canada highlight the need for considering region-specific campaigns, as well as the clear importance of sex- and age-specific content in order to best meet the needs of an aging population.
We acknowledge that this study has some limitations. There are potential limitations in relying on self-reported data. Two issues related to self-reported data are incomplete questionnaires or missing data, which could contribute to biases. Several participants in the Atlantic PATH cohort were missing data on the risk factors of interest and were excluded from the current analysis (Supplementary Table S1). We acknowledge that some characteristics differ between the included and excluded participants; however, in most cases, the proportions tend to reflect similar patterns. For example, a large majority of participants were living in urban centres, had a college or higher level of education, were employed, had an annual household income between $25,000 and $150,000, and were married/living with a partner. Another limitation of self-reported data is under- or over-reporting. For example, the IPAQ is a valid tool used to measure physical activity, but the levels reported may be overestimated. There are also limitations in self-reported dietary data when participants are required to recall past dietary habits over an extended period of time, as well as a possible bias for over-reporting healthy and under-reporting unhealthy dietary options. However, self-reported data are commonly used in longitudinal cohort studies and are supplemented where possible with measured data (e.g., measured anthropometric data). This research represents the baseline period of data collection and is necessarily cross-sectional. The longitudinal nature of the Atlantic PATH cohort will allow us to expand on this work by following health risk factors over time, as well as incident chronic disease outcomes. We will also be able to examine age- and sex-specific similarities and differences across Canada with the regional CanPath cohorts in future research. This study also has several strengths. Although much of the research on health risk factors has primarily focused on sex differences, our study was able to examine both sex differences and age categories, which allows for a life course approach in considering behaviour and risk for chronic disease. This study also benefits from the inclusion of a large participant base across four Canadian provinces and the assessment of multiple health risk factors at one time point.
Conclusions
Lifestyle behaviours are recommended for the prevention and management of chronic diseases. The findings of this study, supported by international research, demonstrate the differences in health risk factors between males and females in a Canadian adult population, as well as across age groups. There have been successful public health efforts targeting modifiable risk behaviours, such as anti-smoking campaigns, which are reflected in decreased smoking rates overall (Centers for Disease Control and Prevention, 2016; Durkin, Brennan, & Wakefield, Reference Durkin, Brennan and Wakefield2012; Golechha, Reference Golechha2016; Health Canada, 2018), and the lower rates of smoking found in younger participants. This study highlights a key opportunity to tailor education efforts and public health interventions to specific populations. Although this study focused on adults, a truly life course approach to the prevention of chronic disease would also include efforts focused on youth and adolescents in order to instill positive lifestyle choices at an early age, which can influence health outcomes in adulthood (Hoare et al., Reference Hoare, Dash, Jennings and Kingwell2018). We recommend that public health efforts in Atlantic Canada account for the role played by sex, gender and age in decision making and risk behaviours, in order to address the high rates of cancer and other chronic diseases in this region.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S0714980821000179.
Acknowledgement
This work was supported by funding from (1) the Canadian Partnership Against Cancer and (2) Health Canada. The cohort analyzed in this study was the Atlantic Partnership for Tomorrow’s Health (Atlantic PATH). The views expressed herein represent the views of the authors and do not necessarily represent the views of Health Canada. The authors declare no conflict of interest. The authors acknowledge members of the Atlantic PATH team responsible for data collection, capture, and coding, and thank all the Atlantic PATH participants who donated their time, personal health history, and biological samples to this project. The authors also thank Gabe Hayman for assistance with French language translation of the abstract.