The Supplemental Nutrition Assistance Program-Education (SNAP-Ed) is the largest federally funded program supporting science-based behavioural focused nutrition education and obesity-prevention efforts targeting low-income populations in the USA(1). The goal of SNAP-Ed is to help SNAP-eligible households and SNAP recipients make healthy lifestyle choices on a limited budget consistent with the Dietary Guidelines for Americans (DGA)(2) and United State Department of Agriculture (USDA) food guidance. The program is offered in all fifty states, District of Columbia and several US territories, with each identifying at least one SNAP-Ed administrative and implementing agency that is responsible for including evidence-based and USDA-approved obesity prevention strategies in their SNAP-Ed plans(2). Approved curricula must demonstrate positive effects on individual behaviours related to food and physical activity environments. In an effort to promote behaviour change and decrease SNAP-Ed participation dropout, curricula that offers short-term education interactions are of particular interest to SNAP-Ed implementing agencies(1,3–Reference Bailey5) . Although nutrition education is essential to achieving dietary and physical activity changes, only a limited number of studies and curricula have been published on SNAP-Ed programs utilising a goal-setting approach with replicable outcomes(6).
Behavioural focused approaches have become an integral part of the design, implementation and evaluation of public health interventions(Reference Glanz and Bishop7–Reference Ajzen11). Research has shown that nutrition education interventions that utilise goal-setting strategies have been instrumental at understanding factors related to dietary choices and effectively influencing behaviour change(Reference Madera, King and Hebl12–Reference Lenzen, van Dongen and Daniëls15). Studies that have been successful at implementing this approach are those designed to set specific goals, promote feedback through self-monitoring and encourage participant commitment(Reference Shilts, Horowitz and Townsend17). Locke and Lantham have utilised a goal-setting theory in the work environment showing that employees who select specific behaviour goals were more likely to set challenging ones and successfully change their behaviours(Reference Locke and Latham16). In addition, a review of literature by Shilts et al. demonstrated that assigning goal setting was more effective than self-setting goals at maintaining desirable outcomes and that proximal goals might be more effective at promoting behaviour change compared with distal goals(Reference Shilts, Horowitz and Townsend17). Additionally, literature on effective approaches to incorporating goal setting among racial and ethnic minorities(Reference Cullen, Baranowski and Smith18) as well as low-income communities is limited(Reference Shilts, Horowitz and Townsend17), especially among SNAP-Ed programs.
Goal setting has been used in the public health field to guide interventions and help individuals regulate their own behaviours. To address the gaps in literature on goal-setting approaches for obesity prevention in SNAP-Ed, this study examines the impact of a goal-oriented nutrition education strategy on the knowledge, self-efficacy and behaviour of adult SNAP-Ed participants.
Methods
Curriculum and program framework
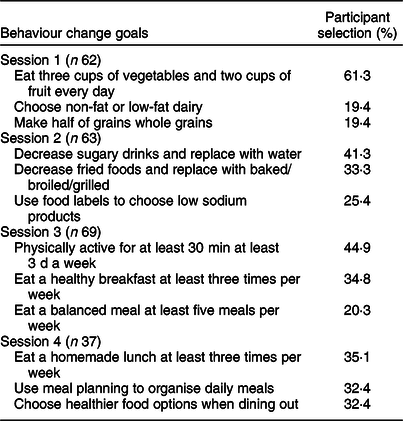
The development of Nutrition for Life (NFL) was aligned with the USDA MyPyramid/MyPlate guidance and the 2010 DGA(2) and utilised a goal-setting approach to offer knowledge, motivation and tools to help adult individuals build the skills needed to make practical changes for a healthy lifestyle. NFL education was delivered in four 90-min weekly sessions over 1 month. The intervention was designed to be short to reduce participant dropout and test whether short-term education could positively affect knowledge, self-efficacy or behavioural change. The sessions were designed to focus on a specific nutrition area and build upon knowledge and skills gained in previous sessions. Participants received a booklet with nutrition information and activity guides aligned with the session content. At the end of each session, participants were presented with a list of three healthy behaviours and asked to select one behaviour to work on during the time between sessions (Fig. 1). Additionally, participants shared their goal selection with other group members and discussed potential strategies to improve eating habits and activity patterns for the upcoming week.
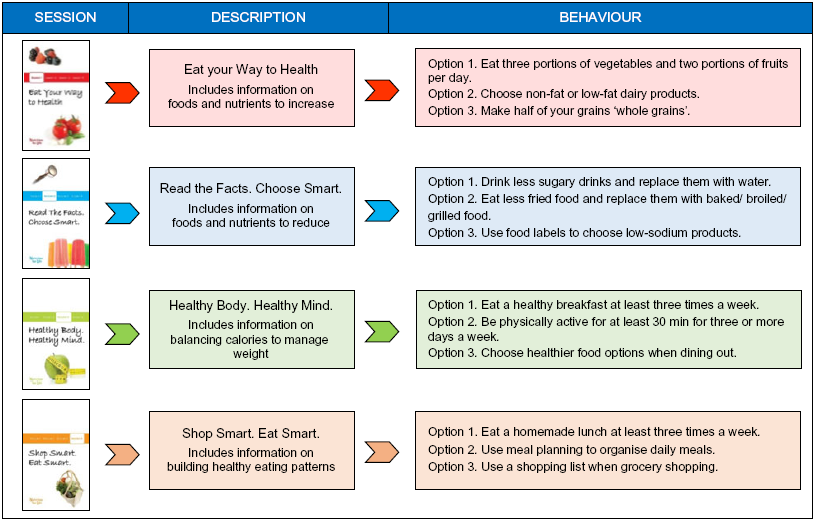
Fig. 1 Nutrition for Life sessions 1, 2, 3, 4 and title, description and behaviour goal selection options, Philadelphia, April 2014–July 2015
Setting
The four-part nutrition series was conducted at two Federally Qualified Health Centers (FQHCs) serving SNAP-eligible communities in Philadelphia, PA, USA. These FQHCs provide comprehensive primary healthcare, family planning, disease management and social services to men, women and children. Each series was conducted in a classroom setting with groups of 5–10 individuals. Sessions were led by a health educator from Health Promotion Council of Southeastern Pennsylvania, Inc. (HPC), a Philadelphia-based non-profit organisation.
Program and study recruitment
From April 2014 to July 2015, adults interested in nutrition education classes were recruited from two FQHCs, two subsidised housing program sites and parent workshops at three schools. Participation in the series was voluntary. Exclusion criteria included those under 18 years of age, pregnant women and those with an inability to attend all four sessions. FQHC staff and healthcare providers referred patients to NFL. Flyers were posted in waiting room areas and distributed to clients by HPC health educators to promote self-referral/enrollment. Sample size calculations were not conducted because participant recruitment was limited by site capacity, program resources and funding.
All participants in the nutrition education series enrolled in the exploratory research study and corresponding program evaluation. The health educator verbally explained research requirements, its purpose, procedures, risks and benefits of participation and confidentiality to each interested participant at the beginning of the first session. All program participants completed written consent forms prior to the start of data collection. Study participants received a $10 gift card at the completion of each session, for up to $40 if all four sessions were completed. Study participants completed a contact form providing their phone number to be reached at 1 week and 1 month for follow-up data collection. No additional compensation was provided for the follow-up measures.
Measurement
Evaluation of NFL education series was focused on assessing changes in knowledge, self-efficacy and goal-setting behaviour related to the content of the NFL curriculum. Participant progress was measured before and after each of the four sessions and 1 week and 1 month after series completion.
The surveys included questions on knowledge, self-efficacy and behaviour related to the content of the session. Knowledge was measured using the sum of correct responses to a series of multiple choice questions focused on the content of each session. Nutrition-related self-efficacy was measured using responses from a series of statements on a four-point Likert scale (‘1 = not confident at all’ to ‘4 = very confident’). Higher scores (range 1–4) indicated a higher level of nutrition-related self-efficacy. Behaviour change was measured using responses from a series of behavioural questions, corresponding to participant’s nutrition-related behaviours during the past week.
Participants were asked to provide demographic information (age, race/ethnicity and gender) on the first session survey. Beginning with the second session, each pre-survey included follow-up behavioural questions based on the goal participants chose to work on at the previous session. At the close of each session, the self-efficacy and knowledge measures were repeated to determine immediate changes in these areas. The surveys were self-administered, and the health educator was available to assist with survey completion as needed (e.g. supporting those with low literacy levels etc.).
All participants who agreed to be part of the study were contacted by research staff to complete a follow-up survey by phone at 1 week and 1 month after the last session. The follow-up survey included the same nutritional and physical activity behavioural questions from the previous surveys to assess longer-term impact of the nutrition education series.
Data analysis
Researchers performed descriptive statistical analysis on demographic data and compared collected measurements at each of the ten intervention stages. Frequency distributions were used to describe participant age, gender and race. Knowledge change was measured using a series of McNemar’s tests. Ordinal self-efficacy and behaviour change questions were analysed using Wilcoxon matched pair signed-rank tests. Fruit and vegetable consumption questions were treated as continuous and analysed using paired t tests. Significance was set at P < 0·05. All data analyses were conducted using the Statistical Software Package IBM SPSS Statistics (version 24.0, SPSS, IBM Corp., 2013).
Results
Sample characteristics
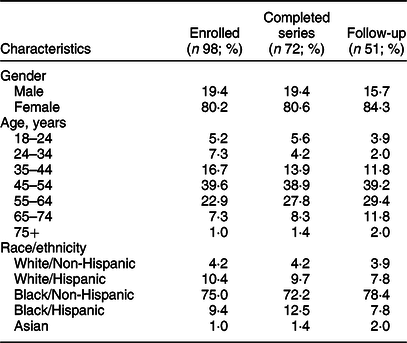
Table 1 shows demographic characteristics of NFL participants. A total of ninety-eight adults enrolled and participated in at least one nutrition education session within the four-part series. Nearly three-quarters (73·5 %) of enrolled participants completed the full series (n 72), and among those, 70·8 % also completed the 1-month follow-up survey (n 51). The majority of participants identified as Black/Non-Hispanic (75·0 %) and female (80·2 %). The age of participants ranged from 18 to 75 years with 45–54 year old (39·6 %) being the largest age group.
Table 1 Demographic characteristics and enrollment status of nutrition for life adult participants in Philadelphia, April 2014–July 2015
Nutrition knowledge change
Participants completed a series of knowledge questions at the beginning and end of each session, for a total of twenty-seven questions. Results presented describe knowledge questions directly related to the positive behavioural outcomes discussed later in the manuscript. These include recommended daily vegetable consumption, recommended daily fruit consumption and recommended physical activity (Table 2).
Table 2 Correct responses to selected knowledge items in the evaluation of nutrition for life adult participants, Philadelphia, April 2014–July 2015
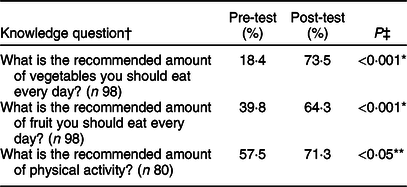
* Significantly different at P < 0·001.
** Significantly different at P < 0·05.
† There were no knowledge questions directly related to water consumption or meal planning, the two other categories of interest for behavioural outcomes.
‡ McNemar’s test used to determine significance for pre-/post-paired data.
Self-efficacy change
Participants also completed a series of nutrition and physical activity related self-efficacy questions at the beginning and end of each session, for a total of thirty-five items. Cronbach alpha coefficients for all four sessions were greater than 0·7, indicating an acceptable level of internal consistency. Participant self-efficacy significantly improved at each session (P < 0·001) and for twenty-five specific nutrition and/or physical activity areas explored in the NFL curriculum (P < 0·05). Table 3 compares the pre- and post-mean, median, sd and interquartile ranges for ten individual questions aligned with observed behaviour change outcomes in the areas of fruits and vegetable consumption, water consumption, physical activity and meal planning. There were significant differences in pre-test and post-test self-efficacy scores for these topics except for water consumption.
Table 3 Mean changes in perceived intention of nutrition for life adult participants, Philadelphia, April 2014–July 2015
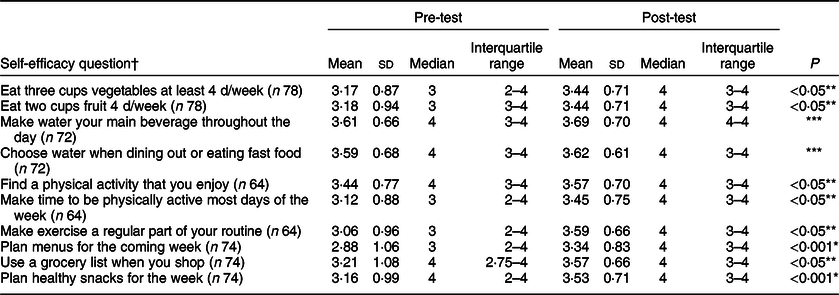
* Significant difference at P < 0·001.
** Significant difference at P < 0·05.
*** No significant difference.
† Comparisons were performed using Wilcoxon signed rank tests. Scale: 1 = ‘not confident’ to 4 = ‘very confident’.
Behaviour change
Participant nutrition and physical activity related behaviour were assessed at three time points: (i) at the beginning of each session for behaviours related to the content of that session; (ii) at the beginning of each subsequent session (1-week follow-up) for behaviours related to the selected goal from the prior week and (iii) at 1-month follow-up for all behaviour items. Table 4 lists the percentage of participants who selected each goal. Goals related to increased fruit and vegetable consumption (session 1), decreased sugary drink consumption (session 2) and physical activity (session 3) were most frequently selected. Session 4 behaviour change goals related to meal preparation were evenly split across categories.
Table 4 Selection of behaviour goal by session of nutrition for life adult participants
Behaviour change related to fruit and vegetable consumption increased at 1-week follow-up, but plateaued at 1-month follow-up (Fig. 2). At 1-week follow-up, participants increased their mean daily intake of vegetables by 0·39 cup (P < 0·01) and fruit by 0·42 cup (P < 0·01). At 1-month follow-up, the increase dropped to 0·25 cup (P = 0·11) for vegetables and 0·25 cup (P = 0·16) for fruit and were no longer significant at the P < 0·05 level.
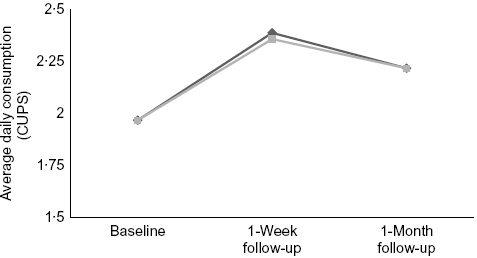
Fig. 2 Average daily cups consumption of fruits and vegetables (n 36) at baseline, 1-week post-intervention and 1-month post-intervention for Nutrition For Life participants. Wilcoxon signed rank tests showed significant differences in fruit and vegetable consumption at 1 week (P < 0·01). ![]() , Fruit*;
, Fruit*; ![]() , vegetables**. *One-week follow-up significant at P < 0·01; **one-week follow-up significant at P < 0·05
, vegetables**. *One-week follow-up significant at P < 0·01; **one-week follow-up significant at P < 0·05
Improvement in some health-promoting behaviours, however, increased at 1 week and continued to increase at 1-month follow-up (Fig. 3). Specifically, the percentage of participants following meal planning guidance (planning seven or more meals per week) increased from 14·8 to 50·0 % (P < 0·01), and water consumption guidance (drinking only water at every meal) increased from 39·0 to 70·6 % (P < 0·01). The percentage of participants exceeding physical activity guidance (at least 30 min of physical activity every day) increased from 16·7 to 36·0 % (P < 0·01). Although the percentage of participants meeting physical activity guidance (at least 30 min of physical activity 3 d/week) increased, and the change was NS.
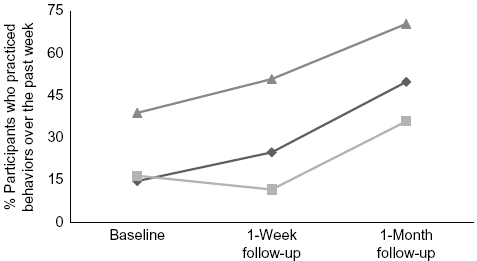
Fig. 3 Percentage of Nutrition For Life participants who met guidelines for health promoting behaviours related to water consumption, meal planning and exercise at baseline, 1-week post intervention and 1-month post-intervention. Wilcoxon signed rank tests showed differences between baseline and one-month follow-up for all three categories (P < 0·01). ![]() , Drank only water at every meal**;
, Drank only water at every meal**; ![]() , planned more than seven of their weekly meals**;
, planned more than seven of their weekly meals**; ![]() , exercised for more than 30 min everyday**. **One-month follow-up significant at P < 0·01
, exercised for more than 30 min everyday**. **One-month follow-up significant at P < 0·01
Discussion
The purpose of the current study is to provide evidence that a nutrition education program supported by a goal-setting behavioural focus strategy has the potential to improve nutrition and physical activity-related knowledge and behaviour among SNAP-eligible individuals. Specifically, program participants showed improvement in knowledge related to recommended consumption of fruits and vegetables and physical activity. Based on reported confidence in ability to select and prepare healthy foods, participant self-efficacy increased at the end of the education series. Significant increases in fruit and vegetable intake were observed at 1-week follow-up; however, the increase reached a plateau at 1-month follow-up. The most significant increases at 1-month follow-up were related to utilisation of meal planning techniques, physical activity and consumption of water. These changes showed a steady increase throughout the entire follow-up period. Thus, utilising a goal-setting approach as part of a SNAP-Ed program delivery enables participants to set and attain behaviour change goals.
Results of this study are aligned with previous findings. The participation in SNAP-Ed evidence-based interventions has a positive influence in nutrition-related behaviours intention among SNAP-Ed participants(Reference Savoie, Mispireta and Rankin19). Participation in SNAP-Ed services supported by a small monetary incentive has the potential to encourage individuals to initially enroll and improve retention rates for populations that are particularly hard to reach and follow-up(Reference Davis, Hitch and Salaam20,Reference Sutherland, Christianson and Leatherman21) . In addition, integrating SNAP-Ed services into primary care settings, such as FQHCs, can support efforts and activities related to health promotion and primary prevention to decrease risk factors for diet-related chronic diseases among low-income families(Reference MkNelly, Nishio and Peshek22). Lastly, the application of specific goal-setting provides a strategy for organising nutrition and physical activity information into practical and manageable steps for at-risk and low-income populations(Reference Brown, Sinclair and Liddle23,Reference O’Donnell, Carey and Horne24) and should potentially be considered as a fundamental component of successful interventions.
Based on literature review and findings from the current study, successful goal-setting strategies to promote healthy behaviour were particularly effective among the SNAP-Ed audience if the process included: (i) participant self-assessment and self-affirmation; (ii) selection of a specific goal and (iii) commitment to short-term changes.
Limitations
Despite important findings, our study has the following limitations. This study did not determine whether the effects of goal setting are sustained beyond the 1-month post-intervention assessment. Data on sustainability of nutrition-related knowledge and behaviour change would strengthen the results of this study as well as increased duration of engagement of participants beyond the 1-month nutrition education series. The pre–post questionnaire utilised in the current study is a self-reported instrument; participant estimates on behaviour change may include overestimation of actual behaviour change(Reference Drennan and Hyde28). Improvements in subsequent behaviours reported by participants might be a consequence of their awareness of being studied(Reference Miller, Abdel-Maksoud and Crane29–Reference Kipnis, Midthune and Freedman31). This research study did not use a control group, which limits the causal inference of the results. Given that NFL is a community-based, direct education program that relies on voluntary participation, a randomised design was not feasible. The small sample size prevents generalisability of findings to the broader SNAP-Ed population, and it is unclear whether these results would persist in a larger study group. While the program retention rate of 73·5 % was relatively high for the SNAP eligible population, individuals who continued with the program may have had greater resources and higher levels of motivation for change in behaviour and knowledge than the general target population of this study. To increase retention rates, participants who completed the program were provided with a monetary incentive, which might have influenced their decision to continue participating. Further, the 1-month follow-up sample was 52 % of the original program sample and is only representative of those who successfully completed the program, not the original study cohort. The small sample size of this preliminary study provides estimates for SDs and effect sizes and inform sample size calculations for future, more rigorous goal-setting nutrition education studies. Finally, although over half of participants reported this was their first SNAP-Ed lesson, there was diversity in the number of lessons participants had taken previously. It is possible participants who had attended multiple lessons had greater exposure to nutrition education and intention to change compared with new, first-time participants.
Conclusion
The current study builds on the recent literature that demonstrates the impact of goal-setting approaches to changing lifestyle behaviour including consumption of healthy foods and promotion of physical activity(Reference Pearson14,Reference Ritchie, Whaley and Spector32) . The positive correlation between changes in knowledge and subsequent behaviour makes the design of this curriculum a practical and valuable approach for delivering SNAP-Ed programs. Further studies may strengthen the result by following SNAP-Ed participants over time to determine if knowledge and behaviour change are sustained. Conducting qualitative interviews with participants could provide a more in-depth understanding on behaviour selection, social support, behaviour control and other promoters and barriers to successful behaviour change. The current study demonstrates implementing goal-setting behaviour strategies to deliver SNAP-Ed programs is effective at producing positive outcomes among adults and emphasises the importance of supporting federally funded nutrition education programs.
Acknowledgements
Acknowledgements: The authors greatly appreciate Jennifer Keith and Lauren Nocito for their support in this project and SNAP-Ed participants in Philadelphia for their willingness to participate in nutrition education sessions, complete the surveys and make this study possible. Financial support: This project was funded by USDA’s Supplemental Nutrition Assistance Program (SNAP) through PA Department of Human Services (DHS). Conflict of interest: There are no conflicts of interest. Authorship: K.V. formulated the research question(s), designed the study, carried it out, analysed the data and wrote the article. Z.B. analysed the data and wrote the article. E.A. analysed the data and wrote the article. W.C. designed the study and analysed the data. G.G. designed the study. M.C. formulated the research question(s) and designed the study. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Institutional Review Board of Public Health Management Corporation through an expedited review process. Written informed consent was obtained from all participants.











