Introduction
According to evidence from patient and mortality register data, mental disorders are related to increased mortality [Reference Bjorkenstam, Ljung, Burstrom, Mittendorfer-Rutz, Hallqvist and Weitoft1–Reference Walker, McGee and Druss4]. However, this research is limited by different kinds of bias. First, the mortality database and register data include routine treatment diagnoses that may suffer from a lack of standardization. Second, for treatment data, sample selection bias is likely. Only a portion of those affected by mental disorders utilize psychiatric treatment [Reference Evans-Lacko, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Benjet and Bruffaerts5]. Those who do not receive professional support might less severely suffer from mental disorders, and data from treatment-seeking population might result in an overestimation of mortality risk among populations with mental disorders. This is particularly important given that considerable proportions of general population were found to have a mental disorder. The prevalence for the 12 months prior to the interview was estimated to be 38.2% of the general population in the European Union [Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jonsson6]. The analysis of general population samples might help to reduce bias, as they are independent of the utilization of health care.
General population surveys used fully standardized diagnostic interviews that may be applied by trained lay interviewers. These data-gathering instruments include the Diagnostic Interview Schedule [Reference Robins, Helzer, Croughan and Ratcliff7] and the Composite International Diagnostic Interview (CIDI) [Reference Robins, Wing, Wittchen, Helzer, Babor and Burke8]. The Diagnostic Interview Schedule was used in the Epidemiologic Catchment Area study [Reference Eaton, Roth, Bruce, Cottler, Wu and Nestadt9]. At four sites in the United States, a sample of 15,440 residents was interviewed during the years 1979–1983, and mortality was proven in 2007 using the National Death Index of the United States. Eleven lifetime diagnoses of mental disorders according to the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association (DSM-III) [10] were analyzed. The hazard ratio (HR) for individuals with alcohol dependence or abuse, adjusted for psychiatric comorbidity, age, sex, education, marital, and occupational status, was 1.33 (95% confidence interval [CI] 1.21–1.47) compared to subjects who did not have the disorder. One limitation of the research using the Diagnostic Interview Schedule is that the classification system of mental disorders was an older version. In comparison to the DSM-III, the DSM-IV provides more precise diagnoses [11].
A study that used standardized DSM-IV 12-month diagnoses provided by an augmented CIDI (M-CIDI) was conducted in Finland [Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12]. In a nationally representative sample of residents 30 to under 70 years of age, M-CIDI data of 5,104 were gathered. Eight years later, vital status was proven. Three disorder groups were analyzed: alcohol use disorders, depressive disorders, and anxiety disorders. Study participants with any alcohol use disorder had an HR of 2.34 (CI 1.53–3.57), and those with any depressive disorder had an HR of 1.89 (CI 1.12–3.21) for time to death after adjustment for psychiatric comorbidity, age, and sex. Individuals with any anxiety disorder had no higher mortality risk than did individuals without the diagnosis [Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12]. One limitation of this study is that only disorders that had existed during the 12 months prior to the interview were reported. A period of 12 months is a short time frame for the occurrence or persistence of such criteria, considering their potential impact on mortality several years later. The use of lifetime diagnoses seems to be more appropriate because they encompass a much longer time span and seem to be less prone to recall bias regarding the time frames, in which the disorder had existed.
Thus far, evidence seems to be lacking on a broader range of lifetime mental disorders that have been diagnosed with an elaborated diagnostic system and their relation to mortality years later. Additionally, little is known about the utilization of treatment for mental disorders and mortality.
The purpose of the present study was to analyze whether the following factors may predict time to death 20 years later in the general adult population: the number of mental disorders; single substance use, mood, anxiety, somatoform, or eating disorders during one’s lifetime and treatment utilization.
Methods
Sample
In a northern German area, a random sample of adults aged 18–64 years from the noninstitutionalized population was drawn using the resident registration office data, which have to be maintained by law for every resident. The sample was stratified by living areas with different social structures. These living areas included the city of Lübeck and 46 surrounding towns and cities and encompassed a total of 193,452 residents aged 18–64 [Reference Meyer, Rumpf, Hapke, Dilling and John13]. The baseline interviews were conducted from July 20, 1996 to March 18, 1997. Among all 5,829 residents who had been eligible for the study, 4,075 (69.9%) gave verbal informed consent, participated in the interview, and provided data that were usable for data analysis [Reference Meyer, Rumpf, Hapke, Dilling and John13]. Additionally, 1,754 (30.1%) could not be reached (665), were reached but refused to be interviewed (979), were deceased or mentally severely handicapped (83), or an interview was conducted but was excluded from analysis (27). Among these, seven participants terminated the interview before its completion; in two cases, the interview was conducted by phone, and the data for 18 interviews could not be analyzed for technical or other reasons [Reference Meyer, Rumpf, Hapke, Dilling and John13,Reference Meyer, Rumpf, Hapke and John14]. Up to more than 12 trials were undertaken to establish a contact with the person by phone or in person.
A mortality follow-up was conducted from April 1, 2017 until April 30, 2018. The median time from the baseline interview to the verification of vital status was 20.6 years (7,532 days; range: 7,326–7,926 days). Vital statistics data of the last residence of each study participant were retrieved using the online vital status and address database of the federal state of Schleswig-Holstein. The data included whether the individual was alive or deceased and, if deceased, the date of death. If vital status of a study participant was not found in the database, we contacted the resident registration offices of the communities where the person had lived including places of residence in six other nations. For the 4,075 baseline study participants, vital status was proven. Among them, vital status was ascertained for 4,028 (98.8%), and it could not be verified for 47 individuals (1.2%). Among the 1,754 nonparticipants, vital status was ascertained for 1,733 (98.8%), and no data were available for 21 individuals (1.2%). Reasons for not being able to identify vital status include special data protection for single persons and the person having been lost from resident registration files (e.g., having no fixed abode or having been moved to other countries and then lost in the data files). The 4,028 study participants with vital status information comprised our final sample for the data analysis. All study participants gave verbal informed consent to participate in the study and were free to terminate the baseline interview at any time. All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The ethics committee of the University Medicine Greifswald gave approval for the study (BB 044/13).
Assessments
The baseline interviews were conducted at the home or another location according to the preference of the study participants. The M-CIDI [Reference Wittchen, Lachner, Wunderlich and Pfister15] was used, a fully standardized psychiatric interview that includes the CIDI. The M-CIDI was administered by 56 psychiatric lay interviewers after they had been trained for 5 days [Reference Meyer, Rumpf, Hapke and John14]. Each interview was conducted using laptop computers. The succession of questions and possible answers were determined by the M-CIDI software. The answers were checked for consistency and plausibility both by the software and by the editors who proved whether any inconsistencies or missing data existed. To limit the amount of missing data, corrections were made on grounds of information from other parts of the interview, the interviewer, or the study participants. They were contacted again in 6% of all interviews [Reference Meyer, Rumpf, Hapke and John14]. The editing process of the M-CIDI is described in detail elsewhere [Reference Meyer, Rumpf, Hapke and John14].
The M-CIDI provided DSM-IV diagnoses for 25 mental disorders. The presence of disorders was assessed based on integrated rules for any time in life prior (i.e., lifetime disorder) with two exceptions. Hypochondriasis was assessed for the last 12 months and dysthymia was assessed for the last 24 months before the interview. Thus, a study participant may have had major depressive disorder and dysthymic disorder in life. We analyzed 5 substance use disorders, 5 mood disorders, 10 anxiety disorders, 4 somatoform disorders, and any eating disorder. The substance use disorders included alcohol dependence, drug dependence, alcohol abuse, drug abuse, and nicotine dependence. According to the M-CIDI, a diagnosis of alcohol or drug abuse was given only if the criteria for alcohol or drug dependence, respectively, were fulfilled in lifetime. Drug dependence included dependence on sedatives, hypnotics or anxiolytics, cannabis, opioids, amphetamines, hallucinogens, or inhalants. The mood disorders were major depression (single episode), major depression (recurrent), dysthymic disorder, bipolar disorder, and mood disorder due to a general medical condition. The anxiety disorders were panic disorder without agoraphobia, panic disorder with agoraphobia, agoraphobia without history of panic disorder, specific phobia, social phobia, obsessive–compulsive disorder, posttraumatic stress disorder, generalized anxiety disorder, anxiety disorder due to a general medical condition, and anxiety disorder not otherwise specified. The somatoform disorders included undifferentiated somatoform disorders, conversion disorder, pain disorder, and hypochondriasis. We collapsed anorexia nervosa, atypical anorexia nervosa, bulimia nervosa, and atypical bulimia nervosa into a single category of eating disorders. Education was categorized into three ranks according to the German school system: basic school education, usually lasting for 9 years; middle school education, usually lasting for 10–11 years; and higher education that qualifies for university entry and usually lasts for 12–13 years. Inpatient psychiatric treatment was assumed if, before the baseline interview, the study participants had ever been an inpatient in a psychiatric, neurological, psychotherapeutic, addiction, or other inpatient treatment facility during their lifetime and if any psychiatric problems during their lifetime had been the reason why they were in such a facility. Outpatient psychiatric treatment was assumed if, before the baseline interview, the individual had ever in his or her lifetime consulted an outpatient psychiatric treatment or counseling facility, an addiction counseling service, or a psychiatrist or a psychotherapist in private practice for psychological problems. Among the vital status data, the date of death was used.
Data analysis
We compared the proportion of deceased individuals among those with and among those without baseline interview data. The Pearson chi-square test was applied. We analyzed whether any of the 25 mental disorders under analysis had been present during participants’ lifetimes prior to the interview as well as the number of disorders. For each disorder, we calculated the proportion of deceased individuals. There was one study participant with missing data for school education. It was replaced by the mean with respect to age and gender.
For analysis of time to death, we used Cox proportional hazards models with the baseline interview date as the origin of the time under analysis. As a precondition of Cox proportional hazard models and logistic regression analysis, it was safeguarded that the minimum number of outcome events (total death cases) per predictor variable was 5–10 [Reference Vittinghoff and McCulloch16]. Accordingly, we collapsed drug dependence and drug abuse into drug-related disorders. We combined panic disorder without agoraphobia, agoraphobia without history of panic disorder, anxiety disorder not otherwise specified, generalized anxiety disorder, obsessive–compulsive disorder, and anxiety disorder due to a general medical condition into other anxiety disorders (Table 1). Due to the number of death cases being less than five, we excluded the following from the data analysis as single predictor variables: bipolar disorder and mood disorder due to a general medical condition. We further excluded conversion disorder and eating disorder from the data analysis of single disorders (Table 1). All 25 disorders were retained in the data analysis of mental disorders in total and in terms of the number of mental disorders. We tested the proportional hazards assumption using graphical methods (Kaplan–Meier plots, log–log-plots) and Schoenfeld residuals [Reference Bellera, MacGrogan, Debled, Lara, Brouste and Mathoulin-Pelissier17, Reference Flynn18]. According to the nonproportionality of hazards based on the crossing of log–log-curves or the Schoenfeld criterion not being met, we excluded posttraumatic stress disorder, undifferentiated somatoform disorder and pain disorder. We calculated Cox proportional HRs with CIs. We fitted two Cox proportional hazard models after adjustment for age and any other mental disorder in addition to that under analysis (model 1) and after additional adjustment for gender and education (model 2). The reference group included study participants who had none of the mental disorders listed in Table 1. For psychiatric comorbidity, the presence of one or more of the other 24 lifetime disorders was included in the data analysis in addition to the disorder of interest. If the data did not fulfill the proportional hazard assumption, we calculated logistic regression analysis and gave the odds ratios (ORs) and CIs. STATA 15.1 was used for the data analysis [19].
Table 1. Proportion of deceased study participants per all persons with disorder in lifetime
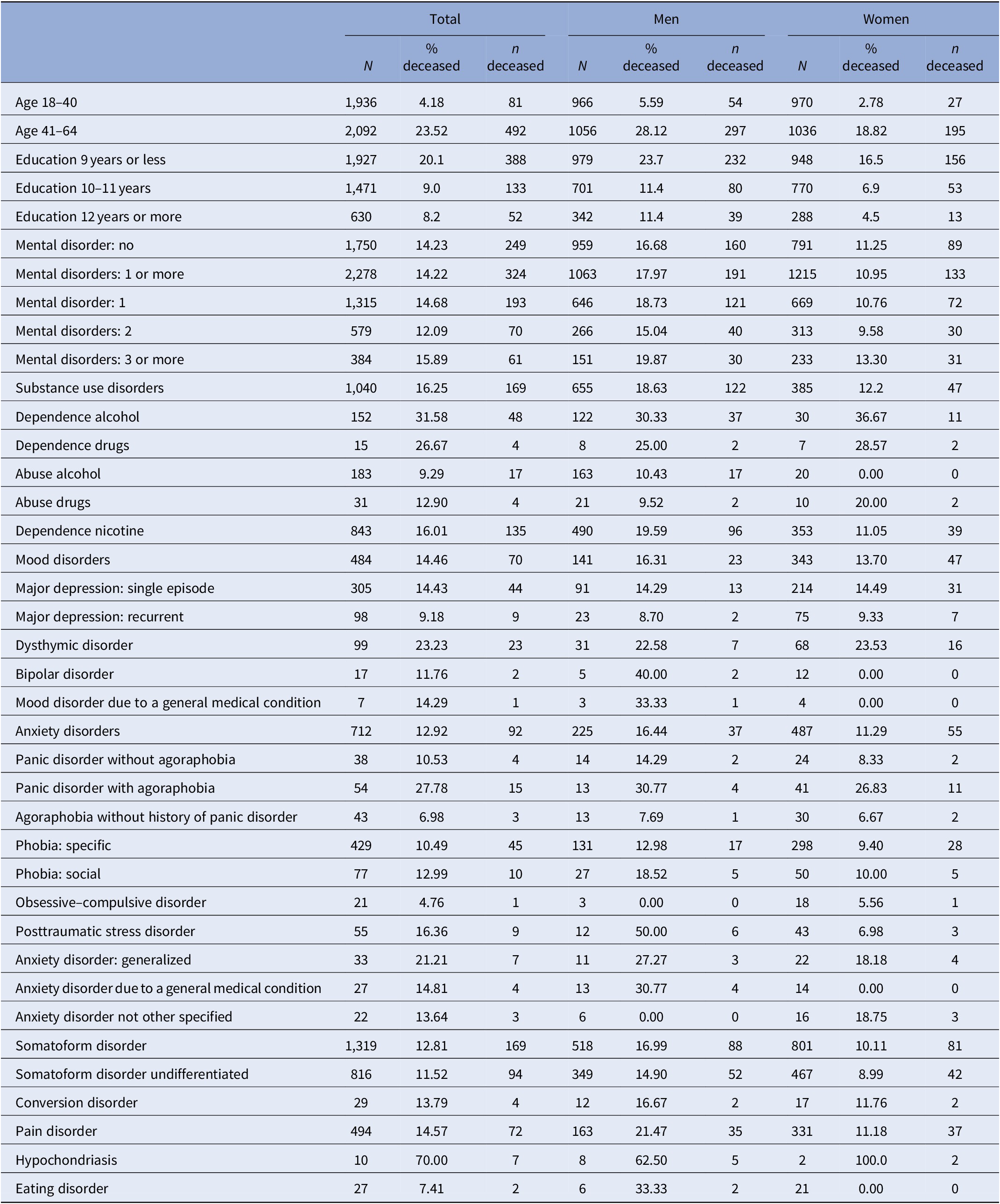
n, 4,028*; %, row percent.
Total sample with vital status data at follow-up. N number of study participants with disorder at baseline.
Results
Among the 4,028 study participants with vital status information, 573 (14.2%) had been deceased, and among the 1,733 eligible persons with vital status information in the sample who had not participated in the study or whose data were unusable, 286 (16.5%) had been deceased. These two proportions differed from each other (chi-square 4.95; p < 0.05). Among the study participants, the age at death ranged from 26 to 85 years. The 573 deceased persons included 222 (38.7%) females.
Table 1 includes proportions of deceased persons per mental disorder. Table 2 provides HRs and CIs for the number of disorders and for each individual disorder. Both among those with any of the 25 mental disorders and among those without any of these mental disorders, 14.2% had been deceased (Table 1; chi-square 0.000, p = 0.996).
Table 2. Mental disorders in lifetime and hazard ratios for time to death
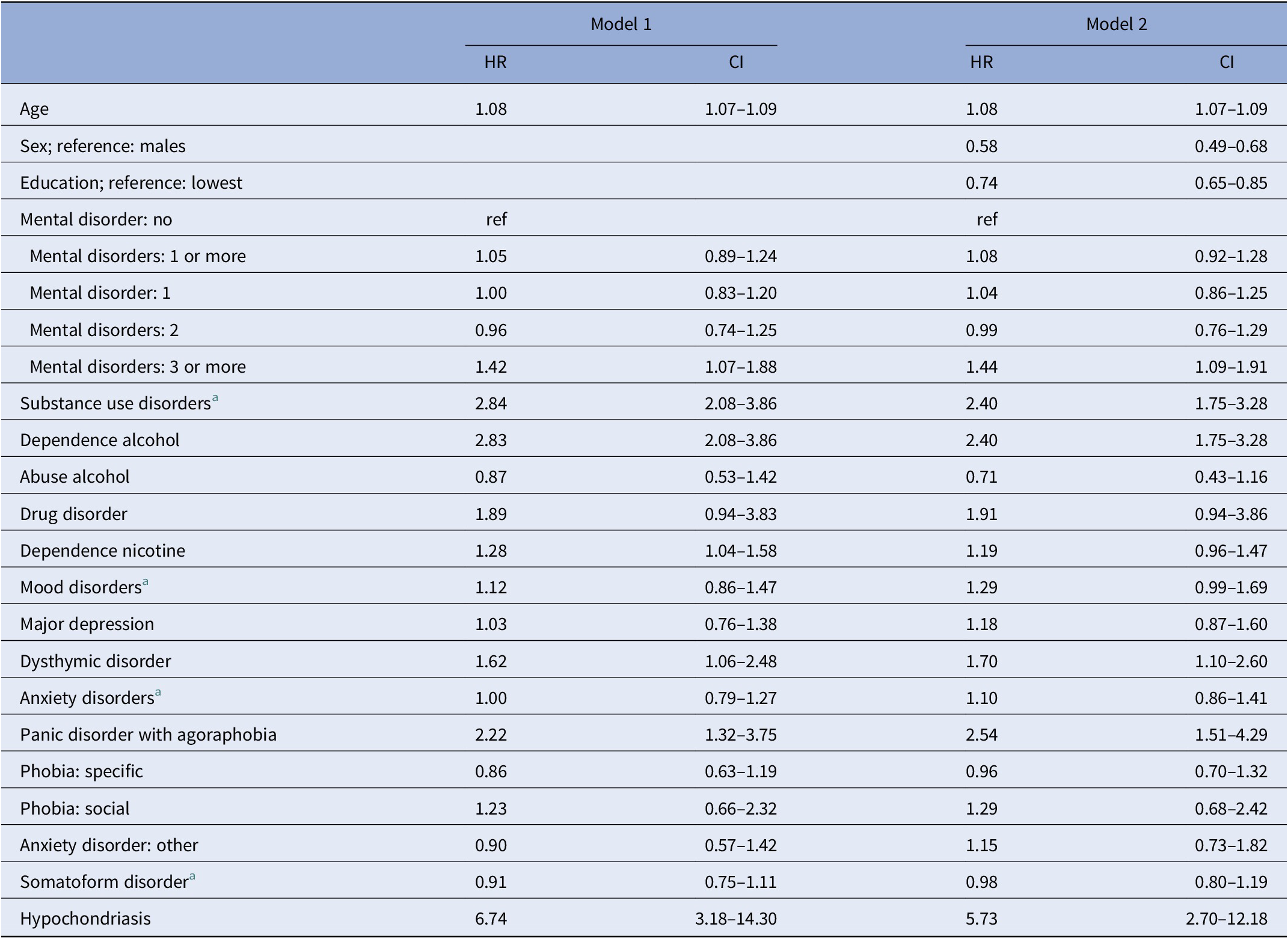
Cox proportional hazard models; study participants with baseline and vital status data.
Model 1: adjusted for age and any other mental disorder in lifetime listed in Table 1; model 2: adjusted for age, gender, education, and any other mental disorder in lifetime listed in Table 1.
Reference group: all individuals without any mental disorder listed in Table 1.
Abbreviations: CI, 95% confidence intervals; HR, hazard ratio; ref, reference group.
a Any of the disorders in this group as listed in Table 1.
For the study participants who had three or more mental disorders, the data revealed a higher HR than for those without any of the mental disorders that were assessed (Table 2). Study participants with alcohol dependence, dysthymic disorder, panic disorder combined with agoraphobia, or hypochondriasis had higher HRs than those without a mental disorder (Table 2). We tested whether the HR of each of the four disorders might be explained by the number of mental disorders. It turned out to be unrelated to time to death after inclusion in Cox proportional hazard models. Subjects with disorders for which the data did not fulfill the Cox proportional hazards assumption had no increased OR for death compared to study participants without any of the mental disorders under analysis and after adjustment for age, sex, education, and any other mental disorders analyzed (posttraumatic stress disorder: OR 1.40, CI 0.64–3.08; pain disorder: OR 1.08, CI 0.80–1.47; and undifferentiated somatoform disorders: OR 0.86, CI 0.66–1.13).
Among women but not among men, having three or more mental disorders (HR 1.57; CI 1.04–2.38) was related to time to death after adjustment for age and education (data not shown). Dysthymic disorder (HR 2.18; CI 1.28–3.72) and panic disorder with agoraphobia (HR 3.25; CI 1.73–6.09) were related to time to death among women after adjustment for any other mental disorder, age, and education. Among men, none of these relations were found, including in a logistic regression analysis for panic disorder with agoraphobia.
Psychiatric treatment was utilized by a minority of the study participants. Among the 2,278 individuals with any mental disorder prior to the baseline interview, 68 (3.0%) had been in inpatient and outpatient psychiatric treatment, an additional 88 (3.9%) had been in inpatient psychiatric treatment only, and an additional 189 (8.3%) had been in outpatient psychiatric treatment only. A higher proportion of those with inpatient psychiatric treatment (45; 28.8%) had died during the follow-up period than of the individuals with outpatient psychiatric treatment only (16; 8.5%) (chi-square 24.39; p < 0.001). The HR for time to death of subjects after inpatient psychiatric treatment was 2.65-fold (CI 1.47–4.75) higher than that of those after only outpatient psychiatric treatment after adjustment for age, sex, and education. Among all study participants who had a mental disorder without utilization of psychiatric treatment, 263 (13.6%) were deceased. Study participants after inpatient psychiatric treatment had an HR of 2.17 (CI 1.58–2.97), and those after outpatient psychiatric treatment only had an HR of 0.84 (CI 0.50–1.39) for time to death compared to those with any mental disorder, but without any psychiatric treatment for a mental disorder after adjustment for age, sex, and education. After additional adjustment for the number of mental disorders, the HR for those after inpatient psychiatric treatment was 2.04 (CI 1.46–2.85).
Discussion
Four main findings of this 20-year mortality follow-up are: (a) three or more mental disorders predicted time to death; (b) alcohol dependence, dysthymic disorder, panic disorder with agoraphobia or hypochondriasis during the lifetime each predicted time to death; (c) women with three or more mental disorders, with dysthymic disorder or panic disorder combined with agoraphobia had a higher HR of time to death compared to women without any of the mental disorders under analysis in this study; and (d) only a minority of study participants had been in psychiatric treatment. Those who had utilized inpatient psychiatric treatment had a higher HR of time to death than those with outpatient psychiatric treatment only and than those with any of the mental disorders assessed but who had not been treated.
Study participants with three or more mental disorders had an HR of 1.42 (1.07–1.88), with the reference group comprising study participants who had no mental disorder. Individuals with two or more disorders did not have a higher mortality than those with one mental disorder only.
There was no difference in the number of deaths between those with any of the 25 mental disorders under analysis and those without. In contrast to studies from treatment facilities, sample selection bias may be assumed to be small due to our random selection from the general population. Additionally, interview bias in our study was likely to be low because of the fully standardized interview, which automatically provides diagnoses independent of the interviewer. We may have overlooked parts of the general population who are affected by particularly severe mental disorders such as psychoses. However, among these individuals, more may be expected to be institutionalized than among individuals in the general population. In addition, these disorders have a low prevalence compared to those that we analyzed.
With respect to alcohol dependence, our data are in line with well-established findings of increased total mortality and shortened life expectancy compared to the age-equivalent general population [Reference Holst, Tolstrup, Sorensen and Becker20,Reference Rehm, Guiraud, Poulnais and Shield21]. Our data confirm those of four mortality follow-up studies in part [Reference Eaton, Roth, Bruce, Cottler, Wu and Nestadt9,Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12,Reference Kingsbury, Sucha, Horton, Sampasa-Kanyinga, Murphy and Gilman22,Reference Lundin, Modig, Halldin, Carlsson, Wandell and Theobald23]. In the Finnish study, those with current alcohol use disorder had an increased HR after 8 years [Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12]. In that study, assessment was limited to disorders in the last 12 months prior to the interview. Reasons for the increased mortality among populations with alcohol dependence include a variety of health disorders, such as cancers and heart disease. However, health risk behaviors, including tobacco smoking, should also be considered.
Our data suggest that dysthymia, rather than major depression, might be the depressive disorder that is related to premature death. Our findings compare to the evidence indicating that dysthymia showed increased HR for total mortality in Finland [Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12]. In the Finnish study, 22.3% of those with current dysthymia had been deceased after 11 years in comparison to 12.8% of those with current major depressive disorder at baseline [Reference Markkula, Harkanen, Nieminen, Pena, Mattila and Koskinen24]. Our data do not confirm that major depression was also related to premature death [Reference Markkula, Harkanen, Perala, Partti, Pena and Koskinen12] and are in contrast to those from a community sample of 1,397 adult persons in Canada [Reference Kingsbury, Sucha, Horton, Sampasa-Kanyinga, Murphy and Gilman22]. In that study, the Diagnostic Interview Schedule was applied in 1992, and in 2011, vital status data were gathered. Depression was related to time to death only in men (HR 2.08, CI 1.15–3.75). Dysthymia was unrelated to death. One reason for the importance of dysthymia being related to time to death might be the chronicity that characterizes the disorder.
Among anxiety disorders, panic disorders with agoraphobia turned out to show increased HR for death. Panic disorders have been revealed by data to be related to cardiac disorders [Reference Caldirola, Schruers, Nardi, De Berardis, Fornaro and Perna25]. Symptoms of panic attacks such as pounding heart, sensations of shortness of breath or chest pain make such relations plausible [11]. Among patients with coronary artery disease, higher rates of panic disorder have been found than in the general population [Reference Caldirola, Schruers, Nardi, De Berardis, Fornaro and Perna25]. Anxiety might be an epiphenomenon of life-threatening disease. However, also anxiety disorder itself might generate symptoms that are related to cardiac disease. It cannot be ruled out that an anxiety disorder elicits cardiac symptoms and somatic disorders that might induce premature death.
For hypochondriasis the question arises whether the M-CIDI provided a valid diagnosis. The validity of the M-CIDI has been revealed by clinical data [Reference Reed, Gander, Pfister, Steiger, Sonntag and Trenkwalder26]. This, however, seems to be uncertain for hypochondriasis. A reason for the proportion of 7 deceased among the 10 persons with hypochondriasis in our sample might be that somatic disorders existed that are not fully explained by hypochondriasis. Healthcare use has been shown to be particularly high among these individuals [Reference Tyrer27]. Somatic concern, which might indicate hypochondriasis, was assessed by a questionnaire in a Finnish study [Reference Tolmunen, Lehto, Julkunen, Hintikka and Kauhanen28]. The findings, including ours, suggest that individuals might have diseases beyond their fears that require further exploration and treatment.
Women more than men might suffer from the number of mental disorders, from dysthymic disorder, and from panic disorder with agoraphobia, with death being more likely than among men. Gender-specific prevalence rates should be considered in this regard. Among the study participants with three or more mental disorders, 60.7% were women; among those with dysthymic disorder, 68.7% were women; and among those with panic disorder combined with agoraphobia, 75.9% were women.
Our data suggest that subjects with a history of inpatient psychiatric treatment have a shorter life expectancy than those without. Treatment utilization could be an indicator of the severity of mental health problems, which might be associated with short time to death. This is supported by an HR of 2.2 (CI 2.1–2.3) for time to death among persons with any mental disorder across 203 studies [Reference Bjorkenstam, Ljung, Burstrom, Mittendorfer-Rutz, Hallqvist and Weitoft1] that included 166 from treatment or other mental health facilities. In contrast to that in our study having any of the 25 disorders under analysis did not reveal an increased hazard ratio for time to death. Clinical samples may be expected to overlook those in the general population who are less severely affected by mental disorders so that they do not seek treatment. In our sample, having consulted an inpatient or an outpatient psychiatric treatment facility for mental disorders was ascertained by only 15.2% of the participants with any mental disorder. These findings might suggest to provide more low threshold intervention approaches for individuals with mental disorders who do not enter inpatient or outpatient treatment facilities that exist so far.
Strengths of our study include that mortality was only marginally lower among the study participants than among the nonparticipants, the standardized interview and the provision of lifetime diagnoses. The standardization of the M-CIDI includes a nonstigmatizing step-by-step procedure to potentially determine a diagnosis. This might have added to the low number of just seven persons who terminated the interview before its scheduled end. The lifetime diagnosis has the advantage that it is less biased by inaccurate recall of the onset and recency of disorders symptoms than it is the case in a diagnosis of the last 12 months. A lifetime diagnosis seems to be a strong predictor of time to death mainly because of the chronicity of disorder. The existence of long-term precursors of a mental disorder such as dysthymia or substance use disorders, the history of the disorder itself, and maturing out of the disorder may be long-term processes that include risks of death from the disorder itself or from accompanying health risk behaviors. Although remission after a short period of time exists, a lifetime disorder bears the possibility that chronic problems may have existed for several years and may result in an accumulation of risks of death.
In addition to the strengths of our study, limitations must be considered. The data do not allow us to draw any causal inferences. The findings have not been adjusted for any health behaviors, somatic disorders, or related treatment. No information about the trajectories of somatic diseases such as cancer was gathered, which may have been the main cause of death. We did not analyze interaction of gender and mental disorders. Larger samples would be appropriate for that. We have not considered multiple testing since our study is explorative in nature. Additionally, different kinds of bias cannot be ruled out. The data are based on the answers to standardized questions from an unknown trained but lay interviewer. Reporting bias may have existed, particularly in case of stigmatized disorders such as alcohol dependence. Although our study participants represented almost 70% of the sample that had been drawn, sample selection bias cannot be ruled out.
We conclude that in this general population sample, three or more mental disorders, alcohol dependence, dysthymia, panic disorder with agoraphobia, and hypochondriasis were related to time to death. More preventive and early intervention efforts to reduce mortality among people who have one or more of these disorders might be considered.
Financial Support
This research has been funded by grants from the German Federal Ministry for Education and Research (grant number: 01 EB 9406) and the German Research Foundation (DFG; grant number: JO 150/11-1; ME 3180/4-1; RU 1570/3-1).
Conflict of Interest
The authors declare no conflict of interest.
Data Availability Statement
The data that support the findings are available from the corresponding author, U.J., upon reasonable request.






Comments
No Comments have been published for this article.