Introduction
During the COVID-19 pandemic, loneliness has been associated with worse mental health outcomes, including increased psychological distress and suicidal ideation (Allan et al., Reference Allan, Volarov, Koscinski, Pizzonia, Potter, Accorso and Allan2021). There is an urgent need to identify those at increased risk of loneliness to ensure that they are provided with appropriate therapeutic supports. Emerging research surrounding predictors of loneliness during COVID-19 has demonstrated that disadvantaged groups tend to be most at risk, including those with lower income and education, unemployment, living alone, and pre-existing physical or mental health conditions (Bu, Steptoe, & Fancourt, Reference Bu, Steptoe and Fancourt2020). The link between disadvantage and loneliness during COVID-19 can be understood by considering social determinants of mental health frameworks, which posit that one's social context and relative standing, including socio-economic status, employment, and living environments are strongly linked with mental health outcomes, including loneliness (McQuaid, Cox, Ogunlana, & Jaworska, Reference McQuaid, Cox, Ogunlana and Jaworska2021).
Social determinants may influence the extent to which an extreme event, like a pandemic, will influence a person's ongoing mental health, including experiences of loneliness (Mao & Agyapong, Reference Mao and Agyapong2021). Whitehead and colleagues (Reference Whitehead, Pennington, Orton, Nayak, Petticrew, Sowden and White2016) proposed a three-level framework that identifies pathways through which social determinants can influence mental health. Firstly, the micro/personal level, whereby a person's financial, informational and power-related resources influence their social standing, living conditions, personal resilience to external events, and control over decisions affecting their daily lives. Secondly, the meso/community level includes the collective capacity an individual has, as part of their membership in broader social groups/communities to create change, be resilient and control negative events, which may be more difficult in neighbourhoods with low resources. Finally, the macro/societal level includes influences on perceived control due to legislation, cultural norms and patterns of discrimination, and the broader context of socio-political transitions. Each of these levels are interrelated – for example, legislation made on a macro level will impact the control people have over their lives on a personal/micro level – and subsequently, the three levels should be explored in context. At each level, social determinants appeared to impact an individual's mental health by interacting with two psychological phenomena: their personal or collective resilience, or capacity to adapt well and continue functioning after such an event (Mao & Agyapong, Reference Mao and Agyapong2021) and perceived control over their daily lives and capacity to remain well (Lachman & Weaver, Reference Lachman and Weaver1998). While theory has linked these phenomena to loneliness (Perlman & Peplau, Reference Perlman, Peplau, Duck and Gilmour1981), limited research has explored this relationship empirically.
Figure 1 adapts this framework to illustrate the potential mechanisms through which the pandemic has resulted in increased loneliness, with impacts on social determinants, perceived control, and resilience. At the micro level, COVID-19 research has demonstrated that those confined to low-quality and unaffordable housing during lockdown experienced constrained control over their environment, particularly when lacking the financial resources to make home improvements, compared to those confined to better-quality housing (Bower et al., Reference Bower, Buckle, Rugel, Donohoe-Bales, McGrath, Gournay and Teesson2021). At the meso level, one example of collective resilience has been the advent of COVID-19 mutual aid groups, sharing resources to support community members experiencing isolation or financial stress (Mao, Drury, Fernandes-Jesus, & Ntontis, Reference Mao, Drury, Fernandes-Jesus and Ntontis2021). At the macro level, state-ordained social restrictions have impacted the perceived control people have over their daily lives throughout the pandemic (Misamer, Signerski-Krieger, Bartels, & Belz, Reference Misamer, Signerski-Krieger, Bartels and Belz2021).

Figure 1. Potential pathways of perceived control, resilience, and loneliness during the COVID-19 pandemic, based on theories of Whitehead et al. (Reference Whitehead, Pennington, Orton, Nayak, Petticrew, Sowden and White2016).
The current paper had several aims: (1) to explore which social determinants predicted loneliness during the first 2 years of the pandemic and (2) to explore the relationship between perceived control and personal and collective resilience with loneliness and social determinants.
Method
Participants
Analysis was conducted on longitudinal data collected over three time points from 7 July 2020 and 31 December 2021 as part of Alone Together, a 24-month study investigating the mental health impacts of COVID-19 among Australian adults. The baseline survey included 2056 individuals, with 65.66% retention (n = 1350) at 6 months and 62.79% (n = 1291) at 12 months, utilising participant data when they had completed all three waves of loneliness questions (n = 1512). This study was approved by The University of Sydney Human Research Ethics Committee (2020/460) and data were collected using Qualtrics software. Participants were recruited across all Australian states and territories through targeted advertisements on social media (i.e. Facebook, Instagram, Twitter), community websites, and physical flyers in public spaces. To reach a broad sample of Australians, including those unlikely to use social media, recruitment also occurred through charitable organisations providing support, social care, accommodation or health services for those experiencing, or at risk of, homelessness, isolation, and financial hardship. To be eligible to participate, participants were required 18+, residing in Australia and have sufficient English proficiency to understand the survey and consent procedures. Further description of recruitment and consent procedures are available in Bower et al. (Reference Bower, Buckle, Rugel, Donohoe-Bales, McGrath, Gournay and Teesson2021, Reference Bower, Donohoe-Bales, Smout, Ngyuen, Boyle, Barrett and Teesson2022).
Participants who had missing data on any of the predictors or outcome variables were excluded from analyses.
Measures
Loneliness (dependent variable)
Social and emotional loneliness was measured at three time points using the six-item De Jong Gierveld Loneliness Scale (DJGL-S; De Jong Gierveld & Van Tilburg, Reference De Jong Gierveld and Van Tilburg2010), resulting in a total loneliness score between 0 and 6, where higher scores indicated greater loneliness. Cronbach's alpha was satisfactory at each time point (α = 0.73, 0.78, and 0.73, respectively).
Micro/personal level independent variables
Demographics and life circumstances
Information was collected regarding participants’ gender identity, age, Aboriginal and/or Torres Strait Islander identity, current employment status, education, residency, language proficiency, mental health diagnosis, household income and expenditure, and LGBTQIA+ identity. See Supplementary Table 2 for coding information on demographic variables. Experiences of stressful life events within 12-months pre-COVID were measured using the List of Threatening Experiences Questionnaire (LTE-Q; Brugha & Cragg, Reference Brugha and Cragg1990), where a higher count indicated a higher number of experiences.
Living conditions
Living conditions, including number of major building problems, satisfaction with natural light in dwelling, frequency bothered by noise while indoors at home and family structure of household, were measured and adapted from The Australian Housing Conditions Dataset (Baker et al., Reference Baker, Daniel, Bentley, Pawson, Stone, Rajagopalan, Hulse, Beer, London and Randolph2018). See Supplementary Table 2 for coding information on these variables.
Resilience and control variables
The 10-item Connor-Davidson Resilience Scale-10 (Campbell-Sills & Stein, Reference Campbell-Sills and Stein2007), was used to measure personal resilience, on a 5-point Likert scale from 0 (not true at all) to 4 (true nearly all the time), with higher scores indicating higher resilience. Perceived control both generally and over one's health was measured via the Perceived Control and Self-Reported Health Questionnaire (Bobak, Pikhart, Hertzman, Rose, & Marmot, Reference Bobak, Pikhart, Hertzman, Rose and Marmot1998) with responses coded between 0 (agree strongly) and 5 (disagree strongly), with higher scores signalling higher control. Baseline Cronbach's alpha was respectable for resilience (α = 0.92) and perceived control (α = 0.71).
Meso/community level independent variables
Neighbourhood/community characteristics
Based on postcode data provided in the baseline survey, two Australian Bureau of Statistics (ABS) location index scores were generated, including Australia Remoteness Structure (Australian Bureau of Statistics, 2018) and Socio-Economic Indexes for Areas Index of relative socio-economic disadvantage (IRSD) for residence area (Australian Bureau of Statistics, 2018).
Personal perceptions of neighbourhood and community
Participants’ perceived neighbourhood belonging was measured using the nine-item Neighbourhood Belonging Scale (Young, Russell, & Powers, Reference Young, Russell and Powers2004), resulting in a total score between 9 and 45. Collective resilience was measured using the five-item Fletcher-Lyons Collective Resilience Scale, summing a total score between 5 and 35 (Lyons, Fletcher, & Bariola, Reference Lyons, Fletcher and Bariola2016). Baseline Cronbach's alpha was very good for collective resilience (α = 0.95). Higher scores on both scales indicated greater belongingness and resilience.
Social networks
The baseline survey measured participants’ social group membership using the four-item Exeter Identity Transition Scale (EXITS) (Haslam et al., Reference Haslam, Holme, Haslam, Iyer, Jetten and Williams2008), assessing both retrospective (pre-COVID) and current social group membership(s). Participants’ responses were coded on whether their engagement in multiple group membership(s), had changed since the start of the pandemic.
Macro/societal level independent variables
Participants were asked about their State/Territory of residence. This acted as a proxy variable to account for the variation in Australian COVID-19 government responses, particularly lockdowns and outbreaks.
Analysis
The STATA mixed command was used to fit two stepwise multi-level linear mixed-effect models predicting loneliness at baseline and two follow-up occasions. Random effects were clustered at a participant level and random slopes were fit, covarying for timing of each participant response. An unstructured covariance model was used. The first model accounted for social determinant variables, and the second model added resilience and control covariates. Given the large number of predictors, tests for multicollinearity were conducted using the STATA collin command, with no evidence for multicollinearity detected.
Due to the temporally staggered nature of participation at baseline, unequal spacing of subsequent follow-ups, and the specific timing of events that may have impacted loneliness (e.g. timing of COVID-19 outbreaks, state-based lockdowns/restrictions), the time variable used for analysis was days since the survey opened (e.g. Day 60, Day 242, Day 425). Timing of major outbreaks/lockdowns (see Supplementary Table 1) and preliminary analysis of graphs presenting loneliness over time suggested loneliness followed a non-linear trajectory; hence, a quadratic time variable was fitted into the model.
Results
Participant Demographic Characteristics
The sample ranged in age (18–89, median bracket: 40–49). Two-thirds (66.47%) identified as female, 8.12% spoke English as a second language, and 1.32% were Aboriginal and/or Torres Strait Islander. Median weekly income of the sample was between $1,075 and $1,700 per week (range: <$300 to >$2,400).
Loneliness
Loneliness mean score at baseline (July–December 2020) was 3.41 on the scale of 0–6 (SD = 1.87, n = 1825), 3.18 (SD = 2.04, n = 1185) at time two (January–June 2021), and 3.40 (SD = 1.90, n = 1269) at time three (July–December 2021).
Regression Analysis
After excluding missing data, 1523 participants were included in analyses, with 3442 observations across three time points.
The following results firstly report the results of model 1 (social determinants as predictors of loneliness) and then secondly reports any changes that occurred in model 2 (model 1 with addition of resilience and control covariates). All model findings reported account for all other variables.
Detailed results from the first (χ2(56, N = 1523) = 584.02, p ≤ .0001) and second models (χ2(59, N = 1512) = 1167.31, p ≤ .0001) are in Supplementary Table 3. Likelihood ratio testing showed that adding perceived control and resilience variables in model 2 made a significant contribution to loneliness, over and above the social determinants tested in model 1 (χ2 (3) = 450.10, p ≤ .0001).
In model 1, trajectories of loneliness showed significant linear (p = .006) and quadratic patterns (p = .003) over time, although the magnitude of change was small. The negative linear coefficient and very small positive quadratic coefficient suggest loneliness followed a slight convex trajectory over time. Examining fitted loneliness scores across time below (Figure 2), trajectories of loneliness appear to follow periods of COVID-19 outbreaks (often accompanied by lockdowns). These results were consistent in model 2.
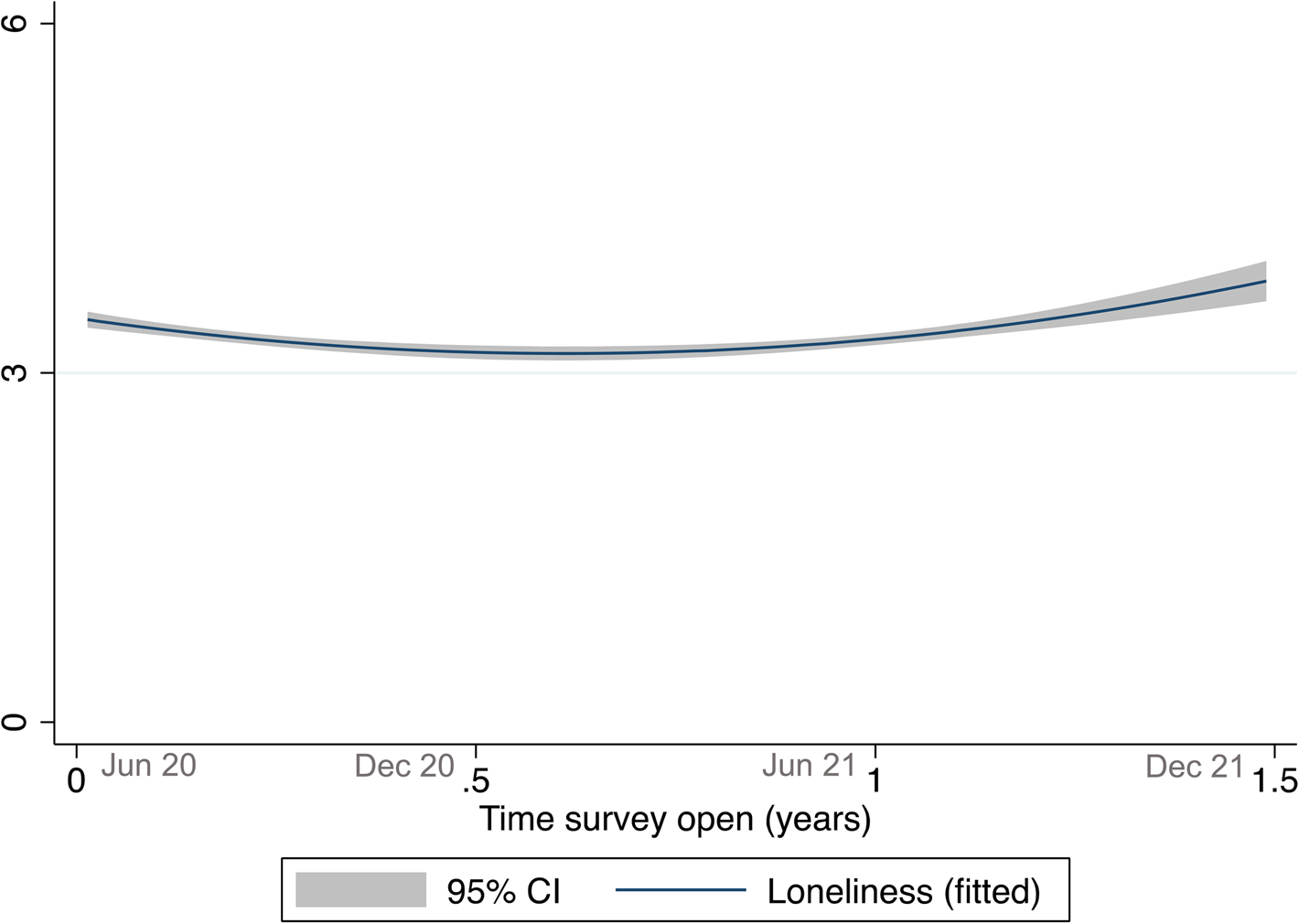
Figure 2. Fitted loneliness trajectories with 95% confidence intervals over the 1.5 years since survey was opened (three time points). The end of the national lockdown associated with the Coronavirus-19 Alpha outbreak coincided with June 2020, and varying lockdowns associated with the Coronavirus-19 Delta outbreak started in late June 2021.
Micro/Personal Factors
Females had an average loneliness score .25 lower than males (p = .006). Those with a lifetime diagnosis for a mental health disorder had an average loneliness score .41 higher than those without (p ≤ .001). Those with higher income tended to be significantly less lonely (β = −.07, p = .041) compared to those with lower income. LGBTQIA+ or Aboriginal and/or Torres Strait Islander status, age, income loss, current employment and tertiary education were not significantly associated with loneliness (p ≥ .05).
Every additional stressful life event experienced in the year pre-COVID was associated with a .09 increase in loneliness score during the pandemic period (p = .003). However, once perceived control and resilience variables were added in model 2, mental health diagnoses, current income, and history of stressful life events were no longer associated with loneliness (p ≥ .05).
Living in a house with satisfactory natural light was associated with a .36-point reduction in loneliness score (p ≤ .001) and every additional major building problem (mould, etc.) was associated with a .11-point increase in loneliness score (p = .002). Issues with noise while at home was associated with a .22-point increase in loneliness, relative to those without noise issues (p = .03). Household family structure was associated with loneliness, whereby single-person households (β = .24, p = .012) and couples with children (β = .29, p = .02) were significantly lonelier than couples without children.
In model 2, living in a house with satisfactory natural light (β = −.31, p = .001) and cumulative major building problems both remained associated with loneliness (β = .07, p = .03), but issues with noise were no longer associated with loneliness (p ≥ .05). Lone person households (β = .31, p = .005) and parents living with adult children (β = .28, p = .025) were significantly lonelier than couples without children in both models. Participants with higher levels of personal resilience (β = −.03) and perceived control over their lives and health (β = −.07) at baseline were less likely to experience loneliness across time (p ≤ .001 for both).
Meso/Neighbourhood and Community Characteristics
In both models, living in inner regional areas, rather than major cities, was associated with an increase in loneliness score (model 1: β = .39, p ≤ .001; model 2: β = .30, p = .002). There were no significant differences across other remoteness indicators and socio-economic disadvantage of living area was not associated with loneliness (p > .05).
Feeling a greater sense of belonging to one's neighbourhood was associated with reduced loneliness (model 1: β = −.08, p ≤ .001; model 2: β = −.04, p ≤ .001). Added at model 2, participants with higher levels of collective resilience at baseline were less likely to experience loneliness across time (β = −.04, p ≤ .001).
Participants whose involvement in multiple social groups had reduced since COVID-19 were significantly lonelier during the pandemic than those whose social contact increased or stayed at pre-COVID levels (β = .37, p < .001). This association remained in model 2 (β = .28, p < .001).
Macro/Societal
There was a significant effect of State/Territory on loneliness, where participants from Victoria were significantly lonelier than participants in New South Wales (NSW) in model 1 (β = .27, p = .02). In model 2, participants from both Victoria (β = .23, p = .04) and Queensland (β = .38, p = .03) were significantly lonelier than those from NSW. Slopes were fitted, testing whether changes in loneliness differed by State/Territory over linear and quadratic time. There was one significant linear effect where participants from South Australia (SA) had a positive linear change, relative to those from NSW (β = 2.13, p = .03), but there was no significant quadratic effect. In model 2, significant linear (β = 2.14, p = .03) and negative quadratic effects (β = −1.44, p ≤ .05) were found for SA. Figure 3 shows the trajectories of States with significant effects, revealing a concave loneliness trajectory over the three time points for participants from SA, whereas participants from NSW showed a convex trajectory.

Figure 3. Fitted loneliness trajectories over the 1.5 years since survey was opened (three time points), categorised by participants’ State/Territory of residence.
Discussion
Social determinants at the micro, meso, and macro levels contributed towards the likelihood of experiencing loneliness during the COVID-19 pandemic. This paper has clear implications for treatment and interventions around loneliness. Results may assist clinicians to identify clients at risk of experiencing loneliness during the pandemic, including Australians who live alone, with children, or in regional areas; are male; have a mental disorder; low income; low sense of belonging to their neighbourhood; low collective resilience; reduced social group membership; or recent experiences of stressful life events prior to COVID-19. People living in poorer quality housing (with building issues, noise, or low light) were also more likely to be lonely, revealing the significant impact of living environments on mental health. Clinicians could also use brief measures of loneliness, like the DJGL to confirm client loneliness.
There was evidence that, as hypothesised, perceived control over daily life and health and resilience (both personal and collective) may play a role in the relationship between some social determinants and loneliness. This was particularly the case among personal/micro-level social determinants, some of which – lower income, lifetime mental disorder, and living in noisy housing – have already been explicitly linked with lower perceived control (Bower et al., Reference Bower, Buckle, Rugel, Donohoe-Bales, McGrath, Gournay and Teesson2021; Eklund & Bäckström, Reference Eklund and Bäckström2006; Lachman & Weaver, Reference Lachman and Weaver1998). Others included being male and having experienced stressful life events in the year prior to COVID-19, such as divorce or natural disaster or couples living with children, compared to those living without. Other research has reflected on the added pressures of parenting and home learning during COVID-19 and resulting social impairment and mental ill-health (Calear et al., Reference Calear, McCallum, Morse, Banfield, Gulliver, Cherbuin and Batterham2022) and of adult children when pandemic-related job loss meant moving back home with ageing parents (Patulny & Bower, Reference Patulny and Bower2022). Although not examined explicitly, one can imagine such added responsibilities in living environment may impact one's resilience and control.
These results show building a sense of control and resilience among people at risk of, or experiencing, loneliness may buffer some of the negative effects of social determinants on health. As these psychological factors are often more malleable than social determinants (e.g. housing), there is a great opportunity for clinicians to work with people at risk of loneliness to target perceived control and resilience and potentially disrupt the impact such social determinants have on loneliness. Past research has confirmed higher perceived control is associated with positive effects on mental health for those experiencing financial disadvantage, low income, and pre-existing mental illness (Eklund & Bäckström, Reference Eklund and Bäckström2006; Lachman & Weaver, Reference Lachman and Weaver1998).
Other social determinants, mostly community level and living conditions were not impacted by resilience and perceived control, suggesting that they may be associated with loneliness through other pathways. These included living in housing that was dark or in poor-repair. Clinicians working with clients living in poor quality housing, without the financial means to make improvements, may wish to advocate for minimum-habitability housing standards for rental and public housing properties, to ensure that all Australians can live in health-promoting housing conditions, as New Zealand's Healthy Homes Standard has done (Tenancy Services New Zealand Government, 2021).
Participants who felt a sense of belonging to their neighbourhood were less lonely, regardless of how well-off their local area was. Disasters like COVID-19 may organically produce emergent neighbourhood ‘groups’, based on a shared identity and desire to help their community survive difficult situations (Drury et al., Reference Drury, Carter, Cocking, Ntontis, Tekin Guven and Amlôt2019). In other instances, simple community-based interventions can improve neighbourhood identification and effectively reduce loneliness (Fong et al., Reference Fong, Cruwys, Robinson, Haslam, Haslam, Mance and Fisher2021).
Participants who perceived their main social groups as more resilient against potential threats and changes tended to be less lonely. As were those who stayed involved in multiple social groups during the pandemic, relative to those whose networks became smaller and less diverse. Unfortunately, maintaining group relationships was not easy for Australians: COVID-19 restrictions prompted temporary or permanent disruption to many in-person community and hobby groups, e.g. choirs (Draper & Dingle, Reference Draper and Dingle2021). Clinicians can leverage the benefits of group membership: connecting clients to meaningful social groups can successfully reduce loneliness (Cruwys, Haslam, Rathbone, Williams, & Haslam, Reference Cruwys, Haslam, Rathbone, Williams and Haslam2021).
Although not tested explicitly, changes in loneliness over time initially appeared to mirror major COVID-19 outbreaks and lockdown periods, suggesting that enforced lockdowns and outbreaks are related to participant loneliness. However, this did not appear the case once differences were tested between States/Territories. Relative to NSW, participants from Queensland and Victoria tended to be lonelier during the pandemic, despite Queensland having fewer lockdowns and COVID-19 cases than NSW (see Supplementary Material). Participants from SA had a different loneliness trajectory than those from NSW, with increases in periods while SA was not experiencing lockdowns. Together, these findings suggest the relationship between lockdowns and loneliness is complex, and state/territory may not be a useful proxy. Future research may benefit from using the Oxford Stringency Index as a proxy for COVID-related restrictions, however these are only available at a national level, potentially missing nuances in local variability in restrictions (Hale et al., Reference Hale, Angrist, Goldszmidt, Kira, Petherick, Phillips and Helen2021). However, other research has also failed to find significant associations between COVID restrictions (e.g. social distancing or quarantine measures) and loneliness (Groarke et al., Reference Groarke, Berry, Graham-Wisener, McKenna-Plumley, McGlinchey and Armour2020).
Strengths and Weaknesses
This is the first Australian study to explore the complex interplay of micro/meso/macro factors and their conjoint influence on loneliness. Key strengths include our longitudinal design and data collection at pivotal points during the pandemic, when most existing pandemic research was cross-sectional, with data collected at a specific point-in-time (e.g. the beginning of a lockdown). This study also offered a unique exploration of the Australian social determinants of loneliness and their relationship with resilience and perceived control.
Unfortunately, the ability to identify the role of these characteristics in the causal pathway between social determinants and loneliness was limited by the single measure of these characteristics at baseline rather than over time. Future research could use a methodology like Structural Equation Modelling with longitudinal data points to develop a more detailed understanding of this relationship. Another limitation was our non-representative sample (e.g. with significantly fewer male than female respondents; under-representation of Aboriginal peoples), limiting the generalisability of findings. Our non-significant finding around a known association – Aboriginality and mental health – could be because our small sample limited power to detect this effect. Another very unusual finding – that men tended to be lonelier than women – could be attributed to self-selection bias. As is common in voluntary online surveys, men were much less likely to participate than women, but it's feasible that men feeling lonely during the pandemic are more likely to participate in a survey about mental health and connection than those feeling more socially connected.
In conclusion, social determinants (including quality housing, neighbourhoods and social relationships, among others) increased loneliness during the COVID-19 pandemic among Australians. While effects were not completely negated by an individual's perceived control and resilience, results suggest that these characteristics may be protective. As these are more readily modifiable than many social determinants, these results provide health practitioners guidance around identifying and helping clients vulnerable to loneliness.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/bec.2023.3.
Acknowledgements
We would like to acknowledge the participants of the Alone Together study for their generosity in sharing their experiences over the COVID-19 period.
Funding
This work was supported by the University of Sydney's LifeSpan Research Network (seed funding grant) and the Henry Halloran Trust (Festival of Urbanism research grant).
Declaration of Interest
None.







