Hypertrophic olivary degeneration (HOD) is a rare condition characterized by the increased size of the inferior olivary nucleus (ION) on MRI of brain, often accompanied by T2 hyperintensity. Reference Kitajima, Korogi and Shimomura1 We describe the case of a 27-year-old man with generalized dystonia due to Wilson’s disease (WD) who presented with bilateral HOD 13 months after initiating treatment. The patient had significant dysphagia and dysarthria, but there was no palatal tremor. In addition to the classic panda signs frequently seen in WD (Figs. 1a and b), this patient’s brain MRI showed increased volume and hyperintensity on FLAIR/T2-weighted images at the ION bilaterally (Figs. 1c and 2). The T2 axial image at the level of the medulla was reminiscent of the ghost in the Pac-Man video game (Figs. 1c and d).

Figure 1: Axial T2-weighted image demonstrates the “face of the giant panda” in the midbrain (a) and the “face of the miniature panda” in pons (b). Axial FLAIR (c) at the medulla oblongata: bilateral hyperintense of both inferior olivary nuclei, consistent with hypertrophic olivary degeneration resembling the Pac-Man ghost (d).
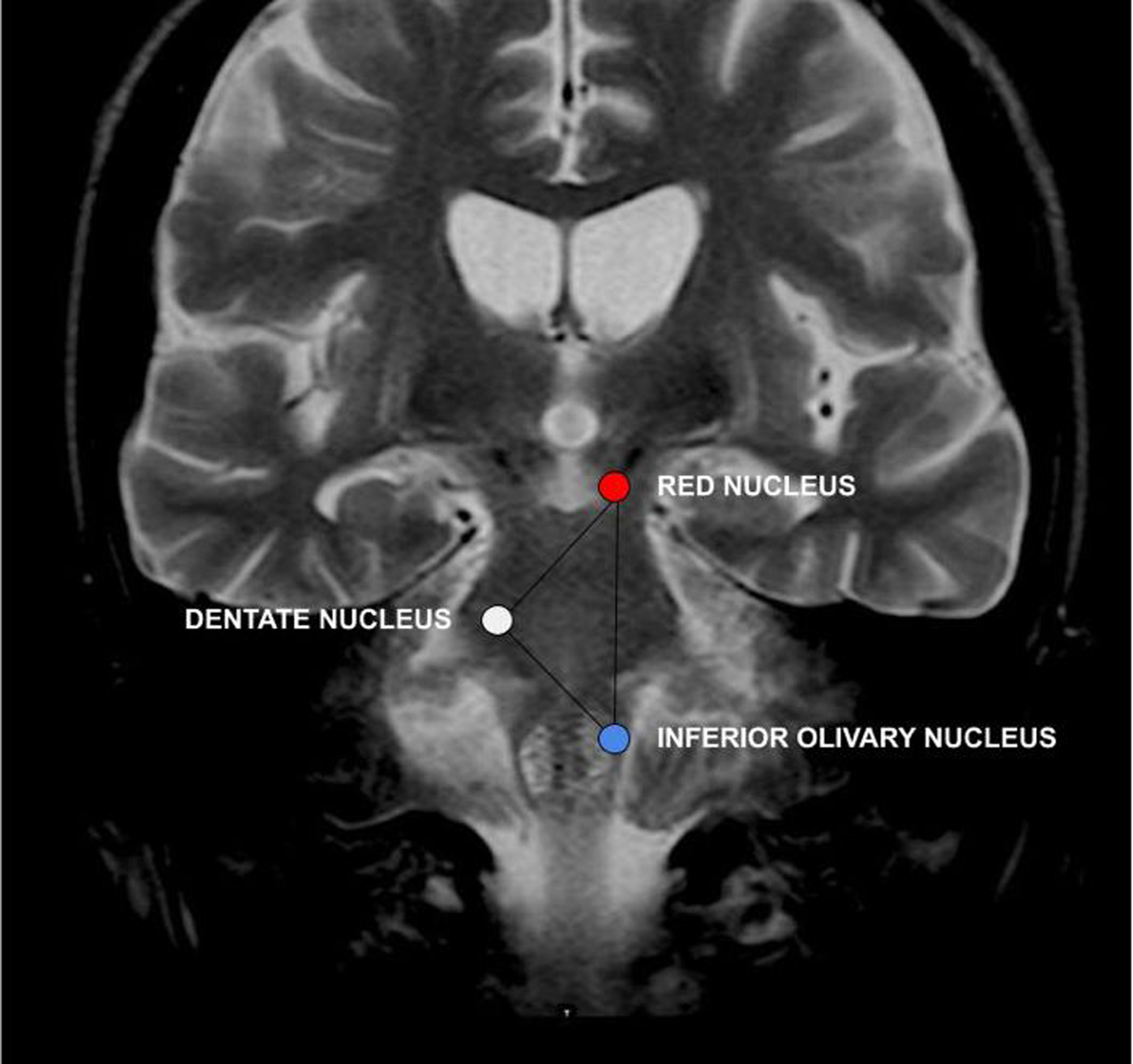
Figure 2: A coronal T2-weighted MR image with schematic of the Guillain–Mollaret triangle.
HOD is caused by injury to the dentato-rubro-olivary circuit, also known as the Guillain–Mollaret triangle. Reference de Raeder M.T., Reis, Campos, Zamilute, França Júnior and Reis2 Efferent fibers originating in the dentate nucleus project through the superior cerebellar peduncle to the contralateral red nucleus. Red nucleus fibers project to the ipsilateral ION via the central tegmental tract (CTT). The ION in turn connects with the contralateral dentate nucleus, via the inferior cerebellar peduncle, thus forming a triangle. Together, these structures are related to the control of fine voluntary movement.
Unilateral CTT lesions result in ipsilateral HOD, while dentate nucleus or the superior cerebellar peduncle lesions cause contralateral HOD. Either bilateral CTT lesion, or unilateral lesion of the CTT and superior cerebellar peduncle/dentate nucleus will lead to bilateral HOD. In our case, as often happens in metabolic disorders, lesions were bilateral. The damage involved both dentato-rubral and rubro-olivary (both part of the CTT) fibers, resulting in loss of transynaptic input on both ION with subsequent degeneration. Iron accumulation was present in the dentate and red nuclei as seen on T2 and susceptibility-weighted images sequences.
Other cases of bilateral HOD in Wilson’s disease have been described. Reference Otto, Guenther and Hoffmann3,Reference Seliverstov, Suslin, Kremneva and Krotenkova4 Ocular myoclonus and nystagmus, dentatorubral (Holmes) tremor and, especially, palatal tremor have been described in association with HOD. Reference Tilikete and Desestret5,Reference Walker, Kim and Samii6 However, as seen in this patient, not all HOD patients will develop the classic symptoms. Reference Robin and Alcala7,Reference Murdoch, Shah and Jampana8 The finding of HOD can be easily overlooked and a mnemonic sign might boost awareness and increase recognition in WD and other conditions. In the case of WD, new changes in MRI might be interpreted as disease progression, but HOD is known to occur as an unusual secondary lesion probably due to axonal degeneration and should not prompt adjustment of treatment. Furthermore, HOD can happen in various other conditions and may be mistaken for demyelination, brainstem ischemia, or even neoplastic lesions. The Pac-Man video game is iconic and highly recognizable. Reference Records9 Previous cases of bilateral HOD described in the literature present with similar appearance to ours and the sign might be useful for teaching purposes. Reference Otto, Guenther and Hoffmann3,Reference Seliverstov, Suslin, Kremneva and Krotenkova4,Reference Arkadir, Meiner, Karni and Lossos10
Statement of Authorship
CA, FR, and LSM wrote the manuscript. ERB reviewed and corrected the manuscript. FR analyzed and discussed the images. All authors participated in the treatment of the patient.
Competing Interests
The authors report no disclosures relevant to the manuscript.






