Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease involving upper and lower motor neurons that leads to progressive paralysis. Reference Wijesekera and Leigh1 Disease progression is unavoidable and often rapid with an estimated life expectancy of 2–5 years from time of diagnosis in most individuals. Reference Mitchell and Borasio2 Since ALS is incurable, medical care is focused on slowing progression, maintaining respiratory function, addressing dysphagia and other symptom management. Multidisciplinary clinics are the standard of care for persons/people with ALS (PwALS). They increase access to specialized equipment and treatment modalities, improve quality of life (QOL), and lengthen survival for PwALS. Reference Shoesmith, Benstead and Chum3-Reference Schellenberg and Hansen5
PwALS commonly experience a relentless series of transitions, conceptualized as changes from one life phase or condition to another Reference Chick, Meleis and Chinn6 as they navigate life with ALS. Advances in life-sustaining treatments and interventions have evolved significantly over the past decades and this has impacted the transitions that PwALS experience as they adopt or decline therapies. Reference Chiò, Mazzini and Mora7,Reference Greenaway, Martin and Lawrence8 For example, the transition to using home mechanical ventilation (HMV) or percutaneous endoscopic gastrostomy (PEG) prolongs life and improves QOL, Reference Khamankar, Coan, Weaver and Mitchell9-Reference Bourke, Bullock, Williams, Shaw and Gibson12 but implementation and uptake is variable. Reference Pols and Limburg11,Reference Baxter, Baird and Thompson13 Responding to other transitions caused by ALS, such as developing new communication strategies and finding alternative transportation modes, can also have a significant impact on QOL for PwALS and their caregivers. Reference Beukelman, Fager and Nordness14,Reference Caron and Light15 The decisions to adopt or decline these therapies and utilize services to facilitate these transitions are evolving with medical advances and are highly complex and individualized. Reference Greenaway, Martin and Lawrence8
Family members are often the primary caregivers for PwALS and relationships between PwALS and their family members play a significant role in the decision-making process. Reference Regan, Preston, Eccles and Simpson16 The transitions that PwALS experience significantly affect their caregiver’s mental health and physical well-being, as well as the caregiver’s relationship with the PwALS. Reference Cipolletta and Amicucci17
This study uses a qualitative descriptive approach to gather information from PwALS and caregivers to understand how PwALS and caregivers experience transitions throughout their ALS journey and how those transitions affect their QOL. From this foundation, both barriers to and models for successful transitions can be identified and can inform clinical practice and clinical communication strategies in ALS care.
Methods
Participants and Setting
The University of Alberta Heath Research Ethics Board approved the study. PwALS were eligible if they were diagnosed with ALS Reference Brooks, Miller, Swash and Munsat18 and were offered or were using either HMV, gastrostomy, or assistive communication technology (ACT). Caregivers of PwALS who met the above criteria were also eligible. Only participants who spoke English or had a caregiver who could translate to English were included. PwALS and caregivers were recruited at a multidisciplinary ALS clinic in Edmonton, Canada, by author M.M. PwALS, and caregivers who had previously provided consent to be contacted for research were also invited to participate by phone or email.
Data Collection
Semi-structured interviews were performed at participant’s homes by author M.M. PwALS and caregivers were interviewed together. The interviews were audio-recorded and lasted 20–60 minutes. The interview guide included demographic and open-ended questions about beliefs, attitudes, and experiences with different kinds of transitions (see Supplementary Material). Other modes of communication including ACT were employed as needed for PwALS. The audio recordings were transcribed by a professional transcriptionist and deidentified transcripts were analyzed by the research team.
Analysis
Thematic analysis occurred concurrent with data collection using established guidelines. Reference Braun and Clarke19,Reference Attride-Stirling20 We met criteria for data saturation with 14 interviews and 15 participants. Reference Saunders, Sim and Kingstone21,Reference Guest, Bunce and Johnson22
Themes were identified using an iterative, qualitative approach. The process involved (1) reading transcripts in detail, (2) categorizing data into labels, (3) grouping similar labels into themes, (4) organizing themes into key themes and subthemes, and (5) comparing and confirming with other members of the research team.
The initial analysis was performed by author M.M. Following this, a second, experienced media coder (W.L.) was familiarized with the nodes and themes to ensure validity and reliability of their application to the interviews. Following training, the second coder independently coded 10% of the deidentified interview transcripts. Kappa scores were calculated using the coding comparison query in NVivoTM 12 (QRS International, Victoria, Australia). 23 The overall Kappa score was 0.81, indicating “substantial” agreement. Reference Landis and Koch24,Reference McHugh25 NVivoTM 12 software was utilized to organize and code data. Demographics were summarized by means and percentages as appropriate.
Results
Participant Characteristics
Interviews were conducted with 14 PwALS and 15 caregivers. The average age ± standard deviation (SD) of PwALS and caregivers were 69.7 ±9.3 and 62.5 ±11.7 years, respectively. PwALS had been diagnosed with ALS 2.9 ±2.7 years prior to the interview. There were 2 paid caregivers, 10 spouses, 1 friend, and 2 children among the caregiver participants. One PwALS lived with a partner who did not identify as a caregiver and was interviewed alone. At the time of interview, eight PwALS reported having paid caregivers (either through a homecare agency or family managed supports) at home and the remaining six dyads were cared for exclusively by familial caregivers. (See Table 1 for participant characteristics).
Table 1: Participant characteristics

PwALS = Person/People with Amyotrophic Lateral Sclerosis.
Key Themes
We identified 14 subthemes that were grouped into 5 key themes. Themes and subthemes with frequencies are outlined in Table 2.
Table 2: Themes and subthemes
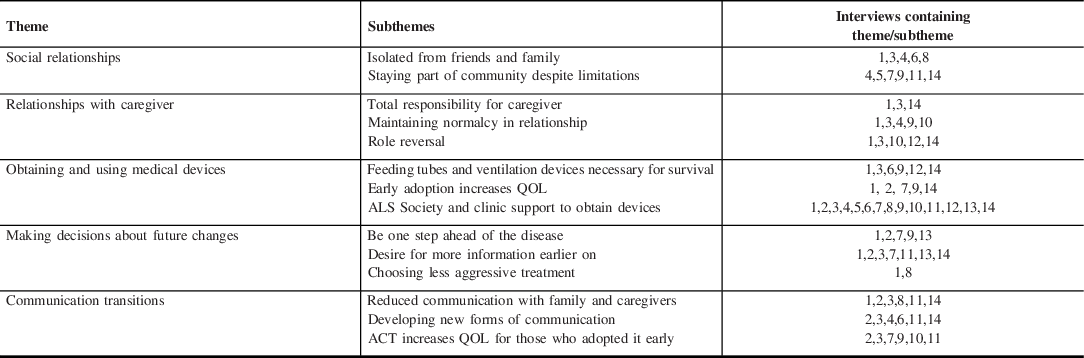
ACT = assistive communication technology; ALS = amyotrophic lateral sclerosis; QOL = quality of life; PwALS = person/people with amyotrophic lateral sclerosis.
Social Relationships
PwALS and caregivers experienced a significant change in their social relationships. The majority experienced this change as feelings of loneliness and isolation. This resulted from loss of participation in regular activities, the feeling of being “homebound,” and feeling disconnected from community.
I used to drive all the time, pick my sister up twice a week and take her for lunch and ALS has taken everything away from me. PwALS 8
Loneliness within the PwALS–caregiver relationship was exacerbated by communication challenges caused by dysarthria. Caregivers and PwALS reported that their social sphere shrank as PwALS became increasingly restricted due to mobility and transportation challenges. While caregivers retained their physical ability to travel, their ability to interact socially was restricted by the time and commitment required of their caregiving role.
I choose to be at home with Patient 1 but I can’t get out. I just can’t run to the grocery store like I used to, or I can’t go to yoga class when I want to. Everything has to be thought through and preplanned in advance. Caregiver (Spouse) 1
Some participants, despite experiencing a similar decline in mobility and communication, retained their social connections and in some cases even developed deeper social relationships. These PwALS and caregivers expressed having sufficient informal support from friends and family and lived either in relative proximity to and/or received regular home visits from friends and family.
I have a lot of support from the church. We have fellowship, Bible study, small group meeting and also the church service on Sunday…we moved here to be close to the church. PwALS 5
Relationship with Caregiver
Caregiver interviews included spouses, children, and paid caregivers. Spouses constituted the majority of caregivers in this study (75%) and, more than other caregivers, reported feelings of “total responsibility.” These spouses described feeling constant vigilance over the PwALS’s health status. For example, many PwALS experienced profound breathing difficulties, which led spouses to feel responsible for their partner’s survival. Paid caregivers and children expressed this sentiment as well, but the theme was much more pronounced among spouses.
If he were choking of anything like that, he is totally in your hands. Total responsibility…(pause begins to cry) It is very stressful, we have had near misses because of it. Caregiver (Spouse) 3
In addition to feeling totally responsible for the well-being of the PwALS, caregivers also experienced practical stresses such as managing the household independently and taking care of finances. All interviewed spouses who were employed before the ALS diagnosis reported either reducing work hours or discontinuing employment to care for their partner. This led to a loss of income in addition to rising costs associated with caring for the PwALS at home.
There was also role reversal for some dyads, with the spouse assuming the responsibilities that had once been the PwALS’s responsibilities. In some cases, the spouse had to learn new skills to adapt to changing circumstances.
I never got onto a computer until after he couldn’t, there have been so many changes that way and responsibilities and running the household and helping him and the finances and stuff and remembering to do the things that he always knew to do. Caregiver (Spouse) 3
PwALS who experienced a role reversal felt a loss of independence as their partner assumed responsibilities that were once theirs. Despite these relationship changes, couples emphasized maintaining normalcy in the marriage. Most dyads reported that their relationship was fundamentally unchanged, and caregivers identified equally as a spouse and caregiver.
(Our relationship) hasn’t really changed…we have talked openly about that. We always joked as we did as young couples, like one day you know you’re going to be taking care of me, and that one day is here now. Caregiver (Spouse) 1
Obtaining and Using Medical Devices
As ALS progressed, most PwALS became dependent on medical devices to maintain survival and QOL. These include (1) mobility equipment, such as wheelchairs, power chairs, hospital beds, and stairlifts; (2) ACT including tablets, voice banking, or eye gaze systems (3) alternatives to oral feeding such as PEG; and (4) HMV. While participants valued all devices, PEG and HMV were particularly important. These were considered life-sustaining and helped alleviate the feeling of total responsibility for caregivers.
I remember one time before the BPAP, she was tired and she gets very flushed and her face one time was literally crimson and she was breathing funny on the couch. As a caregiver out here in the country, just her and I you can get a little bit of panic going on. Knowing that BPAP is here…is like a comfort right. And I know it is a comfort for her putting it on and it is a comfort for me too. Paid Caregiver 14
PwALS and their caregivers believed that PEG and HMV improved QOL and were necessary for survival. A small subset of participants reported dissatisfaction with the bilevel positive airway pressure (BPAP) machine due to mouth dryness, difficulty sleeping when wearing the mask, and a lack of improvement in breathing or energy levels. When asked if they received information about medical devices at the right time in their ALS journeys, most PwALS reported that they would have preferred this information earlier. They linked early adoption to increased QOL.
The feeding tube and the breathing machine we probably should have had that a month earlier if not more. Caregiver (Spouse) 9
All the participants identified the ALS Society (ALS Alberta), a nonprofit, patient support, and advocacy organization (www.alsab.ca/), as an invaluable resource. Participants emphasized the critical role of the provincial ALS society in providing equipment and training in a timely manner and at little or no cost to PwALS.
The society is wonderful in providing things I didn’t even know I needed. PwALS 10
Making Decisions About Future Changes
From diagnosis, PwALS and caregivers need to make significant decisions about treatment and management of ALS. However, planning for future changes becomes increasingly important as ALS progresses to the point where more invasive treatment options are required to sustain life. These decisions to adopt or reject such therapies are largely based on the individual’s QOL, values, and priorities. We asked when clinicians should address progression and advanced care planning. Most participants expressed a desire for more information earlier in the disease course. Participants believed that this would facilitate proactive preparation for future changes.
I think knowledge is a good defense…that people need to be really educated and proactive like voice banking. PwALS 2
Some participants expressed the view that clinicians were withholding information about the later stages of ALS and were reluctant to address end-of-life decisions.
I am ok to talk about it, death…lets get it out there…address it early on, instead of waiting until your on your death bed. I know there is lots out there, but I have to really research and go through google and ask other ALS people and so on and so on, I would like it if the doctors just told me. PwALS 7
For other PwALS, symptom progression was accompanied by decreased desire to pursue therapies and interventions. For example, one PwALS decided to discontinue pharmacological therapies and ACT as the disease progressed.
When the disease progresses depending on how the ALS patient feels it just might not be a will to do those things even though they are available. Caregiver (Spouse) 1
Communication Transitions
All PwALS and caregivers highlighted significant changes in communication caused by the dysarthria commonly experienced by PwALS. Caregivers and PwALS had to develop new forms of communication. For some, this meant high technology solutions such as tablets, eye gaze equipment, or voice banking software. Others preferred simple solutions such as hand signals. This is exemplified in the contrast between the two quotes below.
I have worked with a speech path at the ALS clinic as well as the ICAN centre. I have banked my voice and I have an app I can use from the ALS society. PwALS 2
Actually, we haven’t even talked about it (developing new forms of technology). One way or another we usually figure it out…1 finger for pee, 2 for poo and 3 I run for the door (laughs). Caregiver (Spouse) 4
Participants reported that ACT improved their QOL, particularly when adopted earlier in the disease progression.
I think it gives him more purpose; he has something to look forward too. He tutored me in math and physics and helps us with taxes. Paid Caregiver 3
Due to the training required, some participants chose to adopt new devices or voice banking in advance. Despite the benefits ACT provided for the participants, it also presented new challenges. The amount of time required to communicate frustrated some caregivers and PwALS, and the lack of intonation lead to misinterpretation of meanings.
Sometimes it is hard to feel that you are really on the same page because it takes him awhile to express himself. Caregiver (Spouse) 3
Discussion
We used semi-structured interviews and thematic analysis to improve understanding of the transitions that PwALS and their caregivers experience as they navigate ALS. We explored the ways in which ALS-related transitions influenced people’s lives, disrupted the way they experienced daily activities, and forced people to adapt and change to a “new reality.” Reference Kralik, Visentin and Van Loon26 In this discussion, we explore the primary themes that were identified in our analysis and discuss how pragmatic changes in daily life allow healthcare professionals to better understand the transitions that PwALS and their families/caregivers experience.
It was not surprising that some PwALS and caregivers experience loneliness and isolation after diagnosis. While these aspects of ALS may not be discussed during clinical encounters, loneliness and isolation are risk factors for a variety of negative health outcomes including stress, hypertension, mortality, and reduced QOL for both PwALS and caregivers. Reference Cacioppo and Hawkley27-Reference Vasileiou, Barnett and Barreto29
Spouses of PwALS have been shown to experience significant feelings of loneliness as they cope with the knowledge that their partner has a terminal disease and transition to their role as primary caregivers. Reference Ozanne, Graneheim and Strang30 Participants in a recent qualitative study described the isolation of being a caregiver of a PwALS as “a prison without personal space.” Reference Winther, Kirkegaard Lorenzen and Dryer31 In our study, mobility and transportation were the main factors limiting social interactions. This study was conducted prior to the global COVID-19 pandemic. Undoubtedly, the loneliness and isolation experienced by participants have been exacerbated by public health precautions such as social distancing, and restricted public services and gatherings, including face-to-face ALS support groups, homecare services, and religious gatherings. Further, many jurisdictions have imposed limits on informal gatherings. A recent study confirmed that the COVID-19 pandemic led to an increase in loneliness and social isolation for PwALS. Reference Consonni, Telesca, Dalla Bella, Bersano and Lauria32 Given the transportation limitations and COVID-19 pandemic, online communication in the form of web-based support groups may provide more community interaction for PwALS and caregivers. There is ongoing work in this area, and it warrants further research. Reference Wasilewski, Nonoyama and Dale33
While all participants described transitions in their social interactions, there was an interesting contrast between participants who had maintained or increased their social circle compared to those who did not. Whereas many people experienced greater isolation because of issues related to mobility or communication challenges, a small number of participants reported improved relationships with members of their faith communities, with caregivers and/or with health professionals. This was an unexpected finding; however, similar findings have been reported by Young and McNicholl who found that some PwALS increased their social sphere considerably after diagnosis with ALS. Reference Young and McNicoll34 Participants reported that paid support workers and staff from the local nonprofit ALS Society contributed to their social spheres and in some cases replaced lost contact with pre-ALS friends. In addition to the central task of addressing symptom-related changes, individuals should be encouraged to access available resources including support groups, community, and faith-based centers and groups like the ALS Society. This is an important but often overlooked aspect of care for PwALS and caregivers. The importance of the ALS Society of Alberta was clearly demonstrated in our study, suggesting that PwALS and caregivers will benefit from receiving early information about these services and support offered by these types of not-for-profit patient advocacy organizations. Policymakers should be made aware of the critical role played by these organizations as they fill the gaps in provincially funded programs and equipment services.
Cipolletta and Amicucci characterized ALS as a family disease and described it as being “contagious” in that the sadness and sorrow experienced by the PwALS affect the entire family. Reference Cipolletta and Amicucci17 They also found a significant role change in the marriage relationship when one partner has a disease and the other is a caregiver. Reference Cipolletta and Amicucci17 In our study, spouses reported increased responsibilities and a role reversal due to having to learn new tasks or take on roles that were previously held by the PwALS. These extra tasks, in addition to the time spent performing direct care, meant that spouses had limited options for leisure or employment, especially outside the home. A study by Oyebode et al. found similar results and described carers of PwALS as having “role overload” – lives consumed by complex caregiving roles and little time for previous life activities. Reference Oyebode, Smith and Morrison35 Participants in our study expressed a sense of total or extreme responsibility for the PwALS. This sentiment was primarily due to the respiratory failure experienced by the PwALS and the subsequent dependence on breathing machines. A study by Tromonti et al. found that caregivers of PwALS described their life as a “permanent state of emergency.” Reference Tromonti, Barsanti, Bongioanni, Bogliolo and Rossi36 This parallels the “constant vigilance” many of our caregivers reported. It is unclear from our sample whether this sense of “total responsibility” is common to all caregivers of PwALS and is applicable at all stages of the disease or if respiratory failure is a precipitating factor. The likely need to obtain paid or unpaid caregivers should be communicated early in disease course to ensure that families and PwALS have adequate time to plan, hire, and train staff.
Developing new forms of communication was a significant transition for PwALS and their caregivers. It was also a major factor in maintaining relationships with family and friends. Advances in ACT afford PwALS the opportunity to choose from a variety of high or low technology supports and potentially mitigate the experience of speech loss. However, despite the indisputable benefits, the transition to using this technology can pose significant challenges. To be effective, ACT often requires lengthy training, troubleshooting, and support from specialists. Early adoption and planning are therefore critical. Reference Beukelman, Fager and Nordness14 Low technology supports can lack nuance. Speech-language pathologists are an essential member of the ALS healthcare team and should be consulted early in the ALS disease course to initiate training and support to develop new forms of communication as necessary.
The transition to using HMV increases QOL for PwALS. Reference Baxter, Baird and Thompson13 Both PwALS and caregivers described the transition to HMV as a positive and essential transition that facilitated improved energy, breathing, and sleeping. For PwALS, this transition facilitated greater engagement in desired activities, while caregivers expressed gratitude and relief that it was keeping the PwALS alive. Early information and initiation of HMV were particularly important. Delays caused significant strain on both PwALS and caregivers. These findings support recent recommendations for early referral and adoption of HMV. Reference Baxter, Johnson and Clowes37
This desire for more information earlier on was not limited to adoption of HMV or PEG. PwALS and caregivers noted that neither disease progression nor advanced care planning was adequately discussed by their clinicians. Other studies have found similar results, Reference Silverstein, Stocking, Antel, Beckwith, Roos and Siegler38 while others report that participants avoid future planning and prefer to live in the moment. Reference Flemming, Turner, Bolsher, Hulme, McHugh and Watt39 While information early in the disease course can facilitate critical decisions about care and treatment, the decision-making process for PwALS is a complex and nonlinear process. Reference Hogden, Greenfield, Nugus and Kiernan40 Hodgen et al. investigated shared decision-making in ALS and found that timing and planning was an important but contentious issue. Reference Hogden, Greenfield, Nugus and Kiernan40 Achieving balance between the right information and the right timing is difficult. Clinicians want PwALS to be prepared, but too much information too soon may provoke anxiety. Reference Flemming, Turner, Bolsher, Hulme, McHugh and Watt39 The amount and timing of information given must be patient-centered and driven by the preferences of PwALS. Reference Hogden, Greenfield, Nugus and Kiernan40 At the same time, clinicians should be prepared to provide timely information and referrals where appropriate, particularly for advanced care planning.
The role of palliative care in ALS has been discussed previously Reference Washington, Kukulka, Govindarjan and Mehr41-Reference Oliver, Borasio and Caraceni44 and a recent review of the palliative care literature in ALS has advocated for palliative care consultations early in the disease course. Reference Oliver, Borasio and Caraceni44 In many multidisciplinary ALS clinics, a neurologist or another member of the ALS healthcare team is specifically responsible for addressing palliative care and advanced care planning. However, some ALS clinics have integrated palliative care specialists into the multidisciplinary team. Reference Brizzi, Paganoni, Zehm, De Marchi and Berry43 Participants did not explicitly ask for palliative care consultations; however, these consultations may meet the expressed need for more information about end-of-life issues and facilitate anticipatory planning and decision-making process for both PwALS and family members.
It is unclear whether conversations on palliative care should come from a specialized palliative care physician or if PwALS and caregivers would prefer to have these discussions with familiar members of their multidisciplinary healthcare team. It is important that clinicians working with PwALS have the capacity to engage in effective and compassionate conversations about end of life with PwALS and family members. Consideration should be made for specialized palliative care for PwALS and family members who have more complex goals and require support with psychosocial issues, medical decision-making, or coping/caregiver support. Reference Brizzi, Paganoni, Zehm, De Marchi and Berry43
Although earlier palliative care and end-of-life discussions are key aspects of best care and lead to better compliance with the wishes of patients and family members, previous research has shown that clinicians are reluctant to discuss end-of-life and palliative care topics Reference Brighton and Bristowe45 The majority of patients do not have these discussions with their clinician. Reference Brighton and Bristowe45 It is important that ALS clinicians are proactive and competent in discussions regarding advanced care planning and end-of-life and education standards set by the Royal College of Physicians and Surgeons of Canada are met.
Areas for Future Research
One of the primary findings of this study is that, to plan for future transitions, participants wanted more information, earlier. However, since most of the participants were in the later stages of ALS and were speaking retrospectively, it is unclear if their perspectives would have been the same earlier in the disease course. Future understanding of information needs at different stages of ALS is warranted to understand how early is reasonable and effective to initiate end-of-life and advanced care planning discussions with PwALS. This could be accomplished through longitudinal interviews with PwALS and caregivers at different stages of ALS.
Limitations
Participants were English-language speakers or those with translators and were recruited at a single multidisciplinary ALS clinic. Although this limits transferability, our findings provide a foundation for further study in other jurisdictions and with larger sample sizes. Further, each PwALS/caregiver dyad participated in one interview, thus providing data at a single point in time. Although we did not collect longitudinal data, the in-depth interviews facilitated reflections on the transition’s participants had experienced previously. The inclusion criteria were broad and included a heterogeneous group of PwALS and caregivers who were interviewed together. In some cases, the PwALS’s verbal or written contribution was limited by dysarthria and/or fatigue. In those cases, the caregiver contributed primarily to the interview. The interviews were conducted in people’s homes to facilitate the greatest engagement possible for PwALS. In situations where communication was limited, the interviewer ensured that sufficient time was included to allow for the PwALS to indicate agreement or a wish for the caregiver to modify their statements to better reflect the experience of the PwALS.
Conclusion
This study used qualitative methods to identify and describe important transitions that PwALS and their caregivers experience throughout the ALS journey. The five transition themes experienced during ALS identified can inform clinical decision-making. Our recommendations are practical and feasible with the potential for significant improvement in patient-centered outcomes. Future research should extend these findings into developing further resources that will facilitate and minimize the impact these transitions have on PwALS and their caregivers.
Acknowledgments
The authors would like to thank Kelsey Tymkow and Shelley Wrona for assistance with recruitment and interview guide development. We would also like to thank the ALS clinic coordinator Margot LeClair-Upfold for coordinating recruitment visits and Kelsey Huber for transcribing the interviews. Finally, we are deeply grateful to our participants who devoted valuable time to this study.
Funding
This work was supported by the Covenant Foundation Research Infrastructure grant # 360.CFND.1819.081.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Statement of Authorship
All authors contributed to the conception and design of the study, author MM collected the data and analysis was done by MM, WL, SKG and EM. All authors contributed to drafting and revising the manuscript.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2020.240.






