A 70-year-old female patient with a history of gradual onset unsteady and shuffling gait and generalized body pain was referred to the neurology clinic for assessment of possible parkinsonism. Her history and physical examination were atypical for parkinsonism. As a result, the patient underwent MR head and spine for further evaluation. MR head was unremarkable apart from a small 1 cm right-sided vestibular schwannoma. MR spine showed an intradural mass, which was isointense to muscle on T1-weighted sequence, hyperintense on T2-weighted sequence, and demonstrated relatively homogenous avid enhancement (Figure 1). The mass also involved filum terminale in the sacral spinal canal. The differential diagnosis for the lesion was myxopapillary ependymoma, schwannoma, paraganglioma, and meningioma.
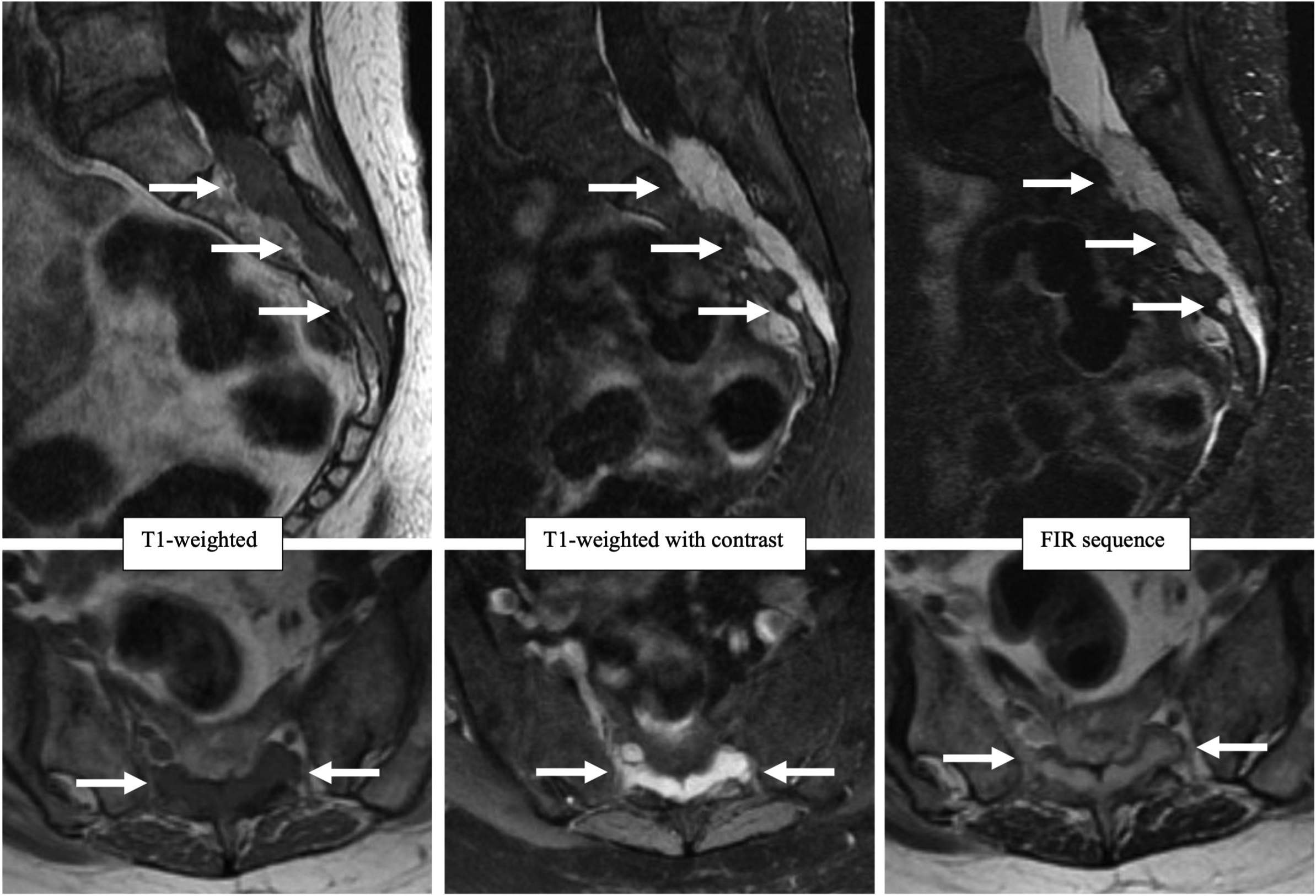
Figure 1: Selected T1-weighted, T1-weighted with fat saturation and contrast, and fast inversion recovery (FIR) images. There is a lobulated intradural avidly enhancing mass filling the sacral spinal canal and extending through the anterior sacral foramina.
The patient underwent a CT-guided biopsy of the intradural sacral lesion, and pathology showed “fibro-osseous lesion suggestive of calcifying pseudo-neoplasm of neural axis with no evidence of malignancy.” Meanwhile, the patient developed progressive urinary incontinence and bilateral heels, ribs, and left hip pain, which on further workup with bone scintigraphy and CT scan demonstrated multifocal fractures (Figure 2). It was suspected that fractures were related to the osteoporosis, given the patient’s age and female sex, with an unusual sudden onset. Her gait abnormality and diffuse skeletal pain could not entirely be explained by her sacral mass; however, the urinary incontinency was felt to be related to compression on sacral nerves. As a result, the decision was made to proceed with surgery to establish a definitive diagnosis and also to decompress the sacral nerve roots to possibly improve her bladder function. The surgical pathology revealed a phosphaturic mesenchymal tumor (PMT) against the first biopsy result. The biopsy was most likely insufficient because of the small sample size, and as a result, the pathology was not identified correctly initially. A selected histopathology image and findings are shown in Figure 3. Due to incomplete resection, the patient underwent radiation and was placed on phosphorus and calcitriol. She showed a drastic improvement with almost complete resolution of multifocal skeletal pain and gait improvement. On a retrospective search, we noticed that patient had a low phosphate level of 0.48 mmol/l (normal range: 0.8–1.45 mmol/l) on an extensive laboratory investigation performed 2 years before the surgery. The patient’s vitamin D level was within normal range at that time.

Figure 2: Posterior view of total body bone scan and selected CT scan images. There are multiple fractures involving bilateral ribs, left hip, and bilateral calcaneus.

Figure 3: A selected histopathological image with hematoxylin and eosin stain shows a moderately cellular tumor composed of bland spindle-shaped mesenchymal cells with entrapped grungy basophilic matrix (arrows) and dilated thin-wall vessels (arrowheads).
Unfortunately, due to the rare entity, the diagnosis of PMT is often delayed, as in our case Reference Ledford, Zelenski, Cardona, Brigman and Eward1 . The purpose of this case report is to increase familiarity with this disease, its clinical and imaging features, and diagnosis.
Most PMTs have been reported in middle-aged adults and very rarely in infants and elderlies Reference Folpe, Fanburg-Smith and Billings2 .
PMT is an extremely rare mesenchymal tumor that can involve soft tissue or bone in any part of the body Reference Shi, Deng, Li, Li, Cao and Coossa3 . The soft tissue type mainly involves the extremities, and bone type, commonly the appendicular skeleton, cranial bones, and paranasal sinuses Reference Folpe4 . In terms of imaging features, the bone lesions are typically osteolytic, with a narrow zone of transition on the CT scan. The soft tissue type of PMT on MRI examinations is typically isointense to muscle on T1-weighted sequence, hyperintense with areas of dark signal on T2-weighted sequence, and demonstrates avid enhancement Reference Folpe4 . In a patient with a clinical diagnosis of oncogenic osteomalacia, 68Ga-DOTATATE PET-CT is the most sensitive study in localizing occult PMT Reference Ho5 . PMT causes diffuse muscle pain and weakness and tumor-induced osteomalacia (TIO) or oncogenic osteomalacia secondary to hypophosphatemia Reference Ghorbani-Aghbolaghi, Darrow and Wang6 . TIO results in multiple fractures in which the main differentiating factor from osteoporotic fractures is sudden onset and hypophosphatemia Reference Folpe4 . Early diagnosis of disease and tumor excision leads to near-complete resolution of symptoms and biochemical abnormalities Reference Kawthalkar, Janu, Deshpande, Gala, Gulia and Puri7 .
Conflict of Interest
We have no conflicts of interest to disclose.
Statement of Authorship
GS: gathering data and writing manuscript. YS: gathering data and writing the draft paper. AL: the initial radiologist who reported the images of the patient and revised the manuscript. WN: the neurosurgeon who operated on the patient and revised the manuscript. LA: the pathologist who reviewed the slide and provided us with the histopathology image and description. MS: the lead who reviewed all the images and pathology in the tumor board and helped with gathering the data and final revision of the manuscript.







