Introduction
Falls are a major contributor to morbidity and mortality among older adults (Burns & Kakara, Reference Burns and Kakara2018; Peel, Reference Peel2011). Falls and their related injuries increase the risk of hospitalization, placement into long-term care, and early death (Gill, Murphy, Gahbauer, & Allore, Reference Gill, Murphy, Gahbauer and Allore2013; Ioannidis et al., Reference Ioannidis, Papaioannou, Hopman, Akhtar-Danesh, Anastassiades and Pickard2009; Katsoulis et al., Reference Katsoulis, Benetou, Karapetyan, Feskanich, Grodstein and Petterson-Kymmer2017; Public Health Agency of Canada, 2014; Thompson, McCormick, & Kagan, Reference Thompson, McCormick and Kagan2006). Older adults who fall may also experience dependence, pain, loss of function, fear of falling, and depression (Scheffer, Schuurmans, van Dijk, van der Hooft, & de Rooik, Reference Scheffer, Schuurmans, van Dijk, van der Hooft and de Rooij2008). In addition to the negative physical and psychological consequences of falls, there are significant financial costs, estimated at $8.7 billion Canadian yearly in total injury costs (Parachute, 2015). Timely identification of risk, and subsequent delivery of fall and injury reduction efforts among older adults present an opportunity to maintain independence and, reduce pain and suffering, while lowering health care costs.
Increasing awareness of the public health impact of falls and the need to support healthy aging has led to the identification of fall and injury prevention as a global priority (World Health Organization, 2007, 2015). Growing interest in coordinated action across health and social care sectors has also galvanized support for research to inform effective fall prevention and injury reduction programs (Choi & Hector, Reference Choi and Hector2012; Cusimano, Kwok, & Spadafora, Reference Cusimano, Kwok and Spadafora2008; Lee & Kim, Reference Lee and Kim2017). Over the last two decades, efforts to translate fall research evidence into clinical practice have increased; several clinical practice guidelines (CPG) and recommendations have been published for various settings across the continuum of care (i.e. community, acute, and long-term care) (e.g., American Geriatrics Society and British Geriatrics Society, 2010; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; US Preventive Services Task Force, 2018). CPGs are systematically developed and consist of evidence-based statements to assist practitioner and patient decisions about appropriate health care for specific individual circumstances (Field & Lohr, Reference Field and Lohr1990). CPGs support the delivery of high-quality care by reducing inappropriate variation in practices and aid clinical decision making to achieve optimal health outcomes (Murad, Reference Murad2017; Scalzitti, Reference Scalzitti2001). Despite the proliferation of fall-related CPGs, most published CPGs have focused on community-dwelling older adults, with sparse attention to other settings across the care continuum (Welch, Ghogomu, & Shea, Reference Welch, Ghogomu and Shea2016). The extent of variation in content and consistency of guidance about the best approaches for fall screening and risk assessment across settings remains unclear. Furthermore, there has not been a synthesis of published CPGs for fall risk screening and assessment across the care continuum.
We conducted a scoping review to identify and synthesize international clinical practice guidelines and best practice recommendations related to fall risk screening and assessment in older adults across the health care continuum. Fall risk screening and assessment are separate but related processes; however, they have sometimes been used interchangeably in the literature. The latter term has been used broadly to refer to fall risk prediction as well as identification of contributing risk factors to target interventions. More recently, the distinction has been clarified; screening aims to identify individuals at risk of falling and determines the need for further evaluation, and risk assessment identifies fall risk factors (e.g., gait and balance problems, previous falls) that will be targeted for intervention (Registered Nurses’ Association of Ontario, 2017). This synthesis describes fall risk screening and assessment approaches across the care continuum and offers insights into identifying gaps and understanding areas where more research is needed to strengthen clinical practice.
Methods
A scoping protocol was developed based on the methodological framework described by Arksey and O’Malley (Reference Arksey and O’Malley2005). The protocol included a systematic process for developing research questions and conducting the literature search including study selection, data charting, collating, summarizing, and reporting the results. Consistent with typical scoping review methodology, quality appraisal was not conducted, as our aim was to provide an overview of published guidelines (Peterson, Pearce, Ferguson, & Langford, Reference Peterson, Pearce, Ferguson and Langford2017). This scoping review is a component of a larger program of work to develop best practice recommendations in fall risk screening and assessment in older adults across the care continuum. The project team includes a wide range of clinical experts, care providers, patient advisors, and decision makers, who have been engaged in a participatory process from conceptualization and design through implementation.
Search Strategy
A comprehensive search strategy was developed by the research team with assistance from a health sciences librarian. We searched ten electronic databases including MEDLINE®, Embase, Cumulative Index to Nursing and Allied Health (CINAHL), Physiotherapy Evidence Database (PEDro), Centre for International Rehabilitation Research Information and Exchange (CIRRIE), REHAB+, Epistemonikos, OTseeker, Infobase of Clinical Practice Guidelines, and Turning Research Into Practice (TRIP) database. In addition, grey literature searches included a wide range of materials published by organizations and professional societies that develop practice guidelines (e.g., Canadian Patient Safety Institute, National Institute for Health and Care Excellence [NICE], Registered Nurses’ Association of Ontario [RNAO], American Geriatrics Society, College of Occupational Therapy, Australian Clinical Practice Guidelines portal, Scottish Intercollegiate Guideline Network [SIGN] and Guideline International Network [G-I-N]).
The development of the search strategy followed the process recommended by the Joanna Briggs Institute (Aromataris & Riitano, Reference Aromataris and Riitano2014; Peters et al., Reference Peters, Godfrey, Khalil, McInerney, Parker and Soares2015). A preliminary search was conducted in MEDLINE (via Ovid) and text words and search terms found in key relevant articles informed the search strategy. The search terms focused on the central concepts of “accidental falls”, “risk prediction or screen”, “risk assessment”, and “clinical practice guidelines”. The final strategy was constructed by combining Index/MeSH terms, keywords, and their synonyms with Boolean logic operators. This was considered to be a more sensitive strategy than only relying on specific terms that may vary for each database. The search developed for MEDLINE was optimized for other databases. (Additional file) Once all search strategies were finalized, they were executed. The reference lists of all included publications were also searched for relevant CPGs that may have been missed in the primary search. The search results were exported to Endnote, a reference management software.
Study Selection
Two independent reviewers applied the selection criteria to screen titles and abstracts for eligibility. We included CPGs or best practice guidelines (BPGs) or recommendations that pertained to fall risk screening and assessment in older adults. All publications that met the following criteria were selected: (1) CPGs that included older adults, defined as 65 years of age and older; (2) pertained to care settings across the care continuum (i.e., community, acute, and long-term care); and (3) published in English over the period 2008 (January) to 2018 (October), to focus on the most recent guidelines.
CPGs were excluded if the publication: (1) focused on clinical or cost effectiveness of interventions to prevent falls; (2) pertained to occupational falls, sport-related falls, or intentional falls; (3) pertained to consequences of falls (e.g., fall-related injuries); (4) focused on the predictive accuracy of a screening or risk assessment tool; and (5) was not accessible for full text review.
Reviewers agreed on 92 per cent of articles. Discrepancies were resolved by discussion and consensus between the two reviewers. Full texts of potentially eligible CPGs were retrieved and reviewed for final inclusion by a single reviewer. A charting table was created to summarize key information relevant to the research question that was extracted (i.e., author, year, country of origin, intended clinical audience, care setting, and fall screening and risk assessment recommendations).
The synthesis described the recommendations within CPGs related to fall risk screening and assessment for each of the three health care settings examined in the review. Any discipline-specific guidelines as well as guidelines intended for specific sub-populations (e.g., those with chronic neurological conditions) that met inclusion criteria were discussed separately. Processes for identification of older adults at risk of falling were compared within and across health care settings. Similarities and differences in fall risk assessment components of CPGs were described.
Results
As shown in Figure 1, 456 records were identified. After duplicates were removed, 330 records were screened for eligibility by two reviewers based on titles and abstracts. Fifty records were selected for full text review. A total of 22 records were CPGs or best practice recommendations that satisfied our criteria and were included in this review (American Geriatric Society and British Geriatric Society, 2010; American Medical Directors’ Association, 2011; Australian Commission on Safety and Quality in Health Care, 2009; Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; College of Occupational Therapists, 2015; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Gagnon & Lafrance, Reference Gagnon and Lafrance2011 (referred to as Institut national de santé publique du Québec); Goodwin & Briggs, for the AGILE Fall Working Group, Reference Goodwin and Briggs2012; Health Care Association of New Jersey, 2012; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; Leland, Elliott, & Johnson, Reference Leland, Elliott and Johnson2012; Naqvi, Lee, & Fields, Reference Naqvi, Lee and Fields2009 (Nurses Improving Health Care for Health System Elders [NICHE] gave rise to the specific guidelines); National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015 (the Health Promotion Board, Singapore produced these guidelines); Thurman, Stevens, & Rao, Reference Thurman, Stevens and Rao2008; US Preventive Services Task Force, 2018; van der Marck et al., Reference van der Marck, Klok, Okun, Giladi, Munneke and Bloem2014; Winnipeg Regional Health Authority, 2011).
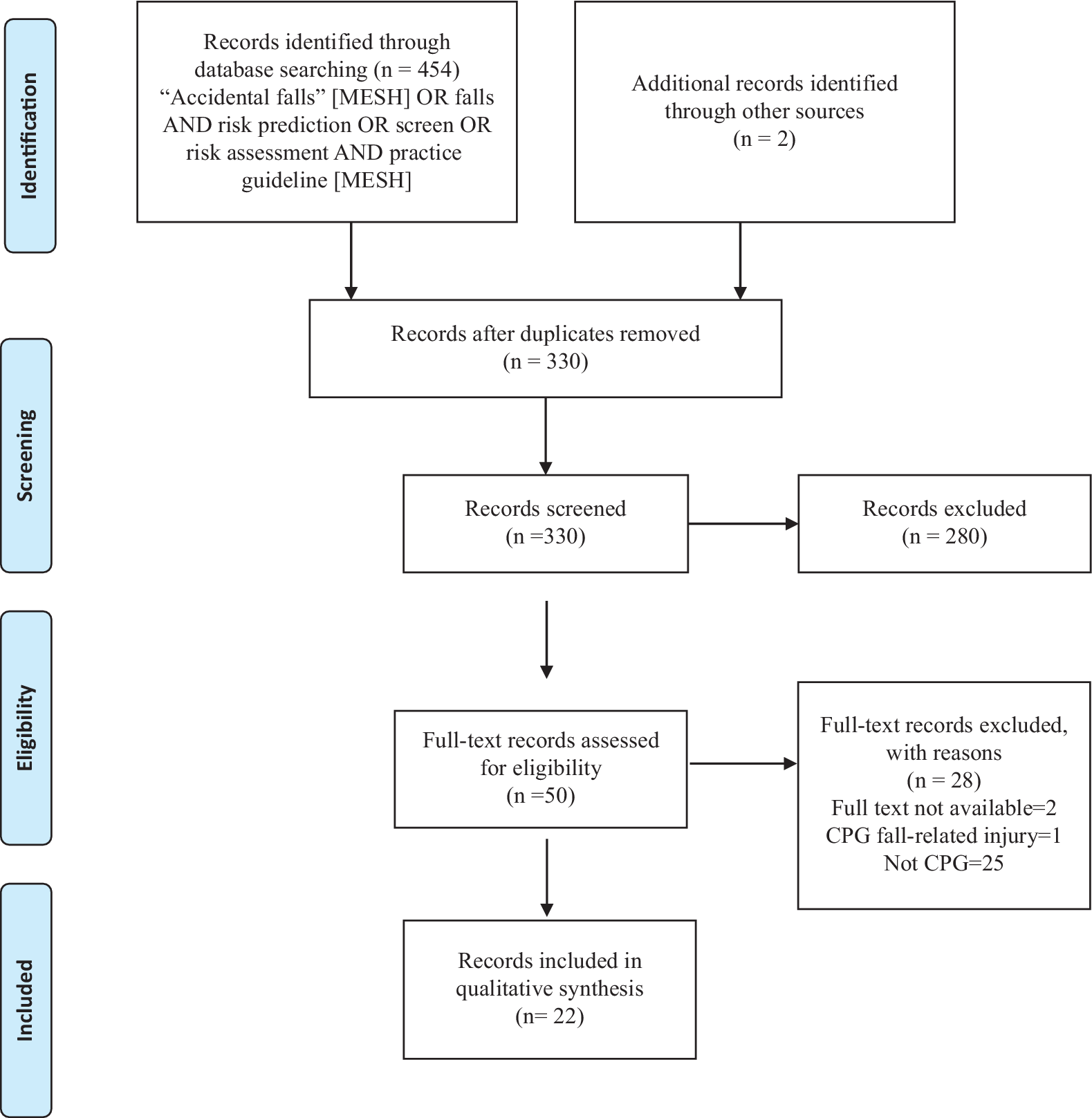
Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing the search and selection process
All CPGs/BPGs pertained to older adults (defined as 65 years of age and older). However, three CPGs applied to the broader group of all adults (18 years of age and older) (College of Occupational Therapists, 2015; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Registered Nurses’ Association of Ontario, 2017). Only one CPG (Australian Commission on Safety and Quality in Health Care, 2009) referred to Indigenous older adults who were defined as 50 years of age or older. In contrast to other guidelines that covered both single and recurrent falls; one CPG pertained exclusively to older adults who had experienced recurrent falls (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a).
Although guidelines were often intended to inform a wide range of health care professionals, CPGs were found that targeted clinical practices of nurses, physical therapists, occupational therapists, and physicians. All CPGs originated in high income countries. There were four CPGs from Canada (Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Winnipeg Regional Health Authority, 2011) and 10 developed in the United States (American Geriatrics Society and British Geriatrics Society, 2010; American Medical Directors’ Association, 2011; Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Health Care Association of New Jersey, 2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; Leland et al., Reference Leland, Elliott and Johnson2012; Naqvi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Thurman et al., Reference Thurman, Stevens and Rao2008; US Preventive Services Task Force, 2018). Guidelines were also identified from Australia, France, Korea, Singapore, Netherlands, and the United Kingdom. Six CPGs were endorsed nationally and were widely implemented in their respective contexts (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; National Institute for Health and Care, 2013; Registered Nurses’ Association of Ontario, 2017; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018).
More than half (n = 12) of the CPGs or their most recent version had been published prior to 2013. Among the CPGs identified, six had been revised at least once and three had been updated within the past 5 years (National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; US Preventive Services Task Force, 2018).
Six CPGs (Australian Commission on Safety and Quality in Health Care, 2009; College of Occupational Therapists, 2015; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011) offered guidance for multiple care settings; while nine CPGs (American Geriatrics Society and British Geriatrics Society, 2010; Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Leland et al., Reference Leland, Elliott and Johnson2012; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018) only provided fall risk screening and assessment guidance for community-dwelling older adults. Another two guidelines provided recommendations for acute care settings only (Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009). Two CPGs offered recommendations for long-term care settings only (American Medical Directors’ Association, 2011; Health Care Association of New Jersey, 2012). Three guidelines did not indicate a particular setting (Goodwin & Briggs, Reference Goodwin and Briggs2012; Thurman et al., Reference Thurman, Stevens and Rao2008; van der Marck et al., Reference van der Marck, Klok, Okun, Giladi, Munneke and Bloem2014).
CPG Fall Risk Screening and Assessment Recommendations
Community fall risk screening
Table 1 summarizes the CPG fall risk screening and assessment recommendations for community care settings. There were 12 general CPGs that pertained to community care settings (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013, Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018, Winnipeg Regional Health Authority, 2011). Guidelines support fall risk screening among community-dwelling older adults (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018; Winnipeg Regional Health Authority, 2011). Not all guidelines address best practice for timing and frequency of screening; however, five CPGs endorse fall risk screening at least annually for community-dwelling older adults (Australian Commission on Safety and Quality in Health Care, 2009;, American Geriatrics Society and British Geriatrics Society, 2010; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011).
Table 1: Components of fall risk screening and assessment in CPGs for community settings
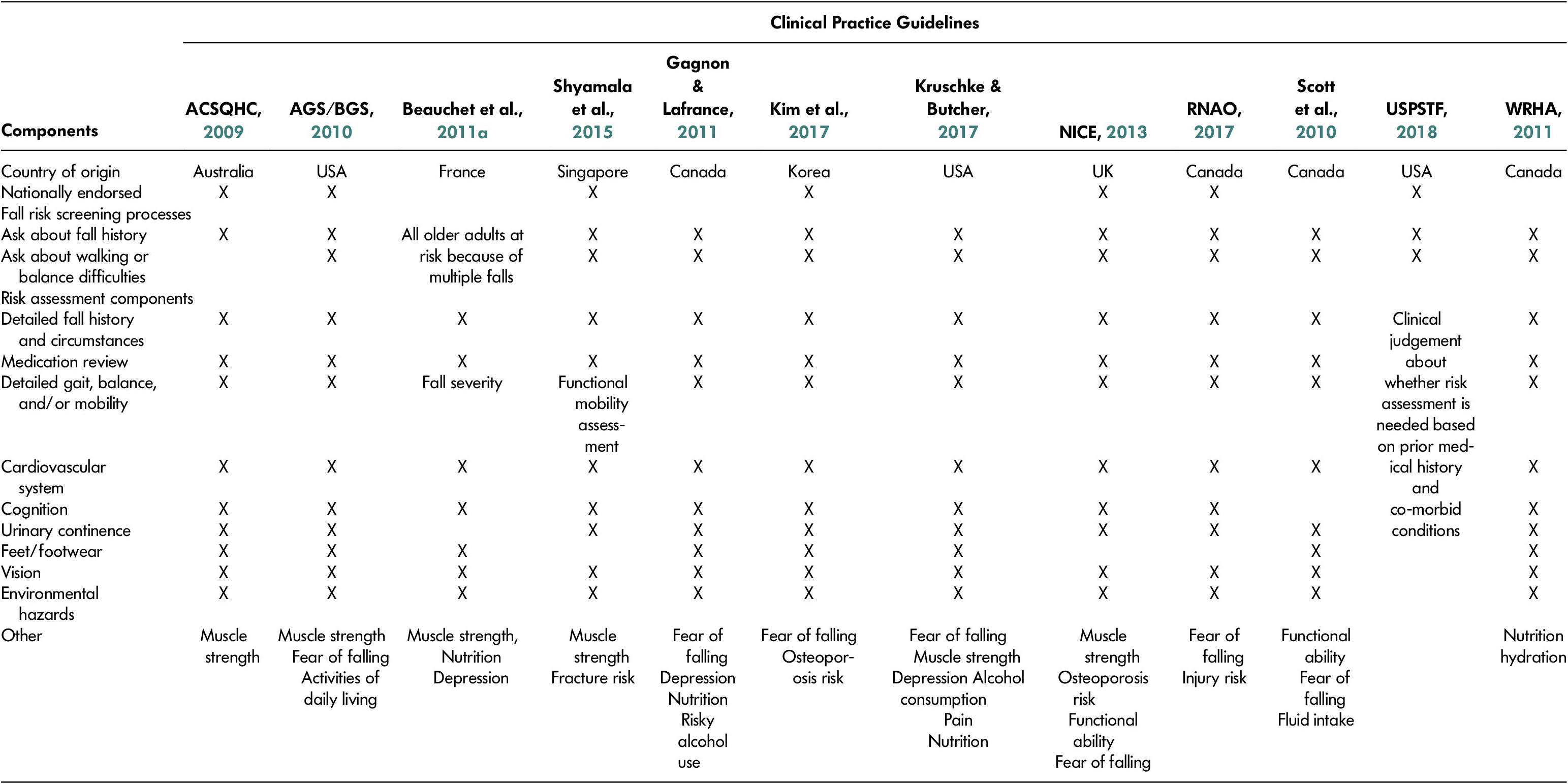
Note. AGS/BGS = American Geriatric Society/British Geriatric Society; ACSQHC = Australian Commission on Safety and Quality in Health Care; CPGs = clinical practice guidelines; NICE = National Institute for Health and Care Excellence; RNAO = Registered Nurses’ Association of Ontario; USPSTF, US Preventive Services Task; WRHA = Winnipeg Regional Health Authority.
Eleven screening algorithms identified an individual at risk of a future fall based on history of falls in a defined period (6 or 12 months) and gait, balance, and/or mobility abnormalities (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018; , 2011). Beauchet et al. (Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a) did not mention screening, because this CPG focused on older adults who had already experienced recurrent falls (defined as two or more falls in the prior 12 months).
Community CPGs identified older adults with gait, balance, and/or mobility abnormalities by asking about difficulties with walking and balance (American Geriatrics Society and British Geriatrics Society, 2010; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015) and/or observation of ambulation (National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010). The Registered Nurses’ Association of Ontario BPG (2017) advised health care providers to use their clinical judgment by looking for apparent disturbances (e.g. unsteady gait, poor balance, impaired mobility). The National Institute for Health and Care Excellence CPG (2013) recommended that observation of the individual’s ability to stand, turn, and sit, was adequate as a first level screen.
A history of a single fall in the prior 12 months, in the absence of other positive criteria, triggered further screening for balance and/or gait problems in four guidelines (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Kruschke & Butcher, Reference Kruschke and Butcher2017; Winnipeg Regional Health Authority, 2011). Examples of recommended gait or balance tests for fall risk screening included Timed-Up-and-Go (TUG), Berg Balance Scale, and Performance-Oriented Mobility Assessment (POMA). The Australian Commission on Safety and Quality in Health Care CPG (2009) also referred to the Sit-To-Stand test and Alternative Step test as fall risk screening tests in community settings.
Only one CPG (Australian Commission on Safety and Quality in Health Care, 2009) mentioned use of multi-item fall risk screening tools in community settings. The Fall Risk for Older People Community version (FROP-Com) was provided as an exemplar of a validated tool that is appropriate for use. The tool considers history of falls in the past 12 months; observations of steadiness while standing up, walking, turning, returning to the chair, and sitting down; and self-reporting the need for assistance in performing activities of daily living.
Community fall risk assessment
Multiple terms (e.g., comprehensive assessment, multifactorial risk assessment) were used by CPGs/BPGs to describe identification of fall risk factors signaling the need for clarity among CPGs and researchers whose work contributed to CPGs. CPGs/BPGs described a similar process for risk assessment including focused or detailed fall history and medical history, physical examination, and assessment of environmental hazards (American Geriatrics Society and British Geriatrics Society, 2010; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; Winnipeg Regional Health Authority, 2011). The use of validated assessment tools that are appropriate for the individual and setting was also supported by three guidelines as part of this process (Australian Commission on Safety and Quality in Health Care, 2009; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Additionally, the Registered Nurses’ Association of Ontario BPG (2017) highlights the multifactorial assessment as one component of comprehensive assessment.
Across CPGs, a fall risk assessment was recommended for community-dwelling older adults at risk for falls. Criteria that triggered an assessment included experiencing recurrent falls (≥ 2) in the previous year; abnormalities of gait, balance, and/or mobility; or presenting to a health care provider because of a fall. The Registered Nurses’ Association of Ontario BPG (2017) recommended that older adults with multiple risk factors or complex needs may require referral to an interprofessional team for further assessment and intervention.
Seven components were commonly considered in detailed assessment of fall risk factors across community guidelines including: (1) focused history to identify circumstances surrounding the fall and consequences; (2) medication review and history of chronic medical conditions; (3) detailed evaluation of balance, gait, and/or mobility; (4) vision; (5) cognitive evaluation; (6) cardiovascular assessment including rate, rhythm, and postural blood pressure; and (7) environmental assessment (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; Winnipeg Regional Health Authority, 2011). Additional components have been included in some CPGs such as perceived functional ability and fear of falling, footwear/foot problems, and urinary continence assessment (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015). Some guidelines also included assessments for osteoporosis (Australian Commission on Safety and Quality in Health Care, 2009; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011), depression (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kruschke & Butcher, Reference Kruschke and Butcher2017), alcohol misuse (Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kruschke & Butcher, Reference Kruschke and Butcher2017), pain and nutrition (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a, Kruschke & Butcher, Reference Kruschke and Butcher2017).
Acute care fall risk screening
Seven general CPGs addressed acute care settings (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Five CPGs recommended that health care providers perform fall risk screening on admission (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Additionally, because the condition of older adults in acute care settings can change rapidly, four guidelines made provisions for reassessment of older adults post-fall, and when changes occurred in health or functional status (Australian Commission on Safety and Quality in Health Care, 2009; Registered Nurses’ Association of Ontario, 2017; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Winnipeg Regional Health Authority, 2011).
Six of the seven CPGs recommended fall risk screening for older adults in acute care settings (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011) (Table 2). Similar to in community care settings, fall risk screening was based on a fall history and gait, balance, and/or mobility abnormalities (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., 2009; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Additionally, Naqvi, Lee & Fields (Reference Naqvi, Lee and Fields2009) screened by asking about fall history or fear of falling. Although four guidelines recommended validated screening or risk prediction tests (e.g. Morse Fall Scale, Heinrich II Fall Risk Model), two CPGs cautioned against their use as a stand-alone approach for screening in acute care settings (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Further, Degelau et al. (Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012) also suggested that any fall risk screening tests should be checked for their sensitivity, specificity, and ability to predict falls at the facility periodically to optimize performance.
Table 2: Components of fall risk screening and assessment in CPGs for acute care settings

Note. ACSQHC = Australian Commission on Safety and Quality in Health Care; CPGs = clinical practice guidelines; NICE = National Institute for Health and Care Excellence; RNAO = Registered Nurses’ Association of Ontario; WRHA = Winnipeg Regional Health Authority.
It was also recommended that a second stage assessment for risk of injury should consider the following factors: age (85 years and older), bone conditions (e.g., osteoporosis, metastases) and coagulation (receiving anticoagulants or bleeding disorder) (Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012). Major surgery was also included as a possible injury risk factor, as wounds could dehisce with a fall (Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012).
Acute care fall risk assessment
One CPG considered all older adults at increased risk of falls by virtue of the health concern that resulted in their hospital admission; consequently, assessment of fall risk factors was recommended for all admitted older adults (National Institute for Health and Care Excellence, 2013). This approach was also consistent with National Institute for Health and Care Excellence (2013) recommendations against the use of risk prediction tests for assigning inpatient fall risk. For other acute care CPGs (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011), a positive screen for fall risk triggered a comprehensive assessment to identify contributory fall risk factors.
Across CPGs in acute care, the most common domains incorporated in fall risk assessment included: history of circumstances of the fall; gait, balance, and/or mobility; medication review, cognition, and environmental safety assessment (Australian Commission on Safety and Quality in Health Care, 2009; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). These CPGs shared some similarities with community care settings. Other factors were sometimes considered, such as postural hypotension, vision, urinary continence assessment, and feet/footwear (Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Winnipeg Regional Health Authority 2011). Kruschke and Butcher (Reference Kruschke and Butcher2017) also recommended assessing for fear of falling, osteoporosis risk assessment, muscle strength, depression, alcohol misuse/abuse, pain, hearing, hydration, and nutrition.
Long-term care fall risk screening
Seven general CPGs provided recommendations for long-term care settings (Australian Commission on Safety and Quality in Health Care, 2009; American Medical Directors’ Association, 2011; Health Care Association of New Jersey, 2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Similarly to in acute care settings, fall risk screening was recommended upon moving into long-term care, and if there were significant changes in health or functional status (Australian Commission on Safety and Quality in Health Care, 2009; Health Care Association of New Jersey, 2012; Registered Nurses’ Association of Ontario, 2017) and post-fall. Guidelines also recommended screening routinely such as quarterly (Winnipeg Regional Health Authority, 2011), semi-annually (Australia Commission on Safety and Quality in Health Care, 2009; Health Care Association of New Jersey, 2012) or at least annually (National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011).
Fall risk screening approaches in long-term care settings were similar to those in other care settings (Table 3). A prior history of falls and reported and/or demonstrated impairment of gait, balance, and/or mobility were recommended for fall risk screening in four CPGs’ algorithms (Australian Commission on Safety and Quality in Health Care, 2009; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017). An alternative approach considered the majority of older adults to be at increased risk of falling, and recommended a more detailed assessment of fall risk factors for all older adults (Australian Commission on Safety and Quality in Health Care, 2009; Health Care Association of New Jersey, 2012).
Table 3: Components of fall risk screening and assessment in CPGs for long-term care settings
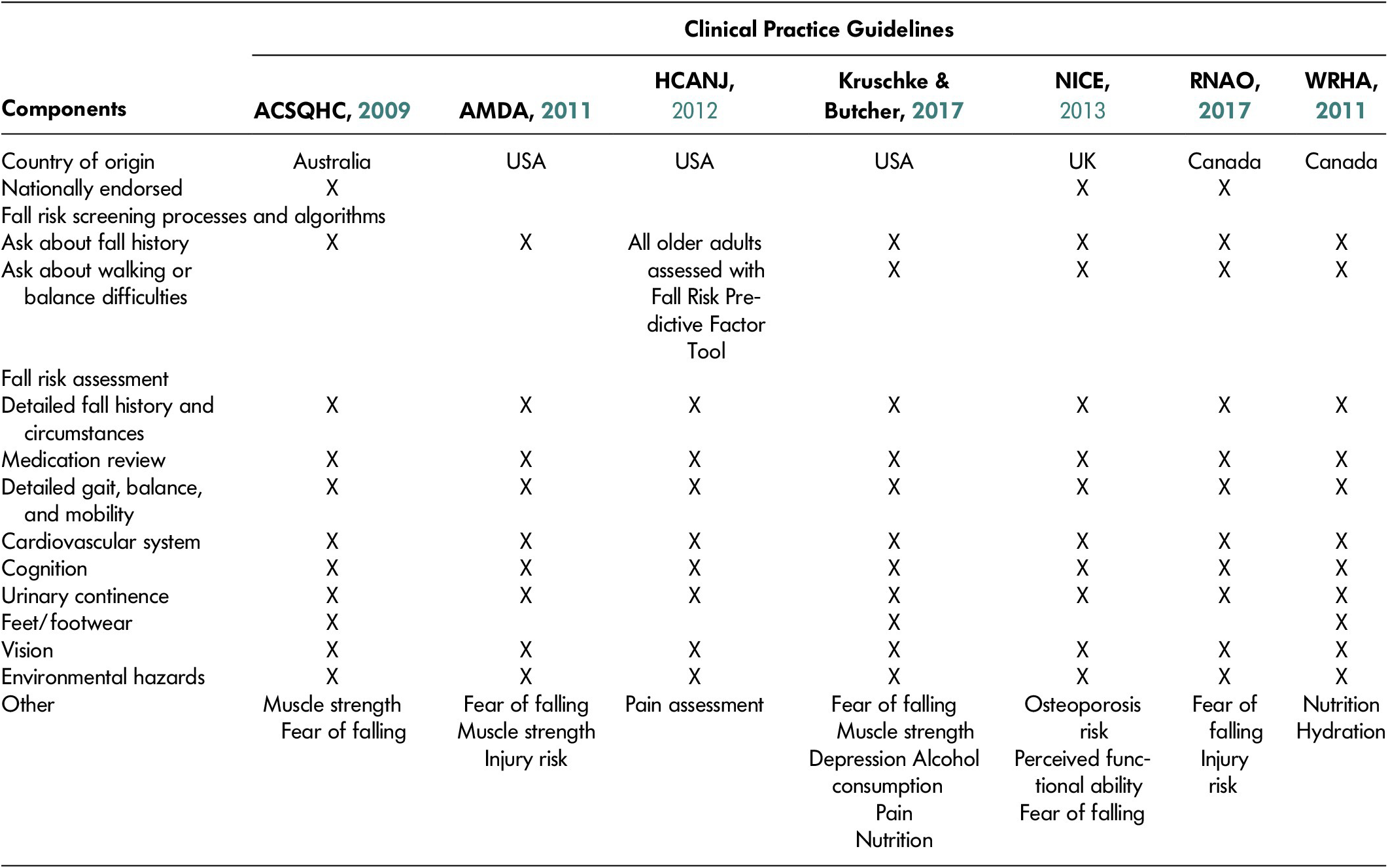
Note. ACSQHC = Australian Commission on Safety and Quality in Health Care; AMDA = American Medical Directors’ Association; CPGs = clinical practice guidelines; HCANJ = Health Care Association of New Jersey; NICE = National Institute for Health and Care Excellence; RNAO = Registered Nurses’ Association of Ontario; WRHA = Winnipeg Regional Health Authority.
Long-term care fall risk assessment
Risk factors for falling were identified using multi-item risk prediction tools in three CPGs (Australian Commission on Safety and Quality in Health Care, 2009; Health Care Association of New Jersey, 2012; Winnipeg Regional Health Authority, 2011). Some CPGs also integrated assessment with care planning as part of an established single assessment process geared towards a holistic approach to management across multiple domains (American Medical Directors’ Association, 2011; Health Care Association of New Jersey, 2012; Winnipeg Regional Health Authority, 2011). An example is the use of the minimum dataset (MDS) that captures comprehensive information about functional and mobility status, cognition, mood and behavioral symptoms, geriatric syndromes, chronic conditions, and medications. A fall care area assessment (CAA) can be triggered during completion of the MDS that prompts further investigation of fall risk factors. The care plan reflects interventions to address any areas of concern.
Seven components of fall risk assessment were common to all long-term care CPGs: focused fall history; medication review; gait, balance, and/or mobility assessment; cognition; vision; urinary continence assessment; and environmental safety (Australian Commission on Safety and Quality in Health Care, 2009; American Medical Directors’ Association, 2011; Health Care Association of New Jersey, 2012; National Institute for Health and Care Excellence, 2013; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Winnipeg Regional Health Authority, 2011). Other areas that were considered included fear of falling, footwear/foot problems, and muscle strength (American Medical Directors’ Association, 2011; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017) osteoporosis, postural hypotension, pain assessment, and nutrition (Health Care Association of New Jersey, 2012; Kruschke & Butcher, Reference Kruschke and Butcher2017; Winnipeg Regional Health Authority, 2011).
Common Screening and Risk Assessment Criteria across General CPGs
Identification of older adults at risk of falls was based on fall history and reported and/or demonstrated abnormalities of gait, balance, and/or mobility in 12 general CPGs (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; American Medical Directors’ Association, 2011; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; US Preventive Services Task Force, 2018; Winnipeg Regional Health Authority, 2011). The other three general CPGs focused on identification of risk factors for all older adults who were considered at risk for falls (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Health Care Association of New Jersey, 2012; Navqi, Lee & Fields, Reference Naqvi, Lee and Fields2009).
In acute care settings, three CPGs cautioned about the use of screening or risk prediction tools to assign inpatient risk (Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; National Institute for Health and Care Excellence, 2013; Registered Nurses’ Association of Ontario, 2017). Two of the three guidelines advised that screening tests should not be used as a stand-alone approach (Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Registered Nurses’ Association of Ontario, 2017) but should occur as part of a more comprehensive assessment.
Among CPGs that identified tests of balance and/or gait as part of fall risk screening process, the Timed-Up-and-Go test was mentioned by nine guidelines (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; Winnipeg Regional Health Authority, 2011). Because screening is intended to be a brief process, time, cost, and practicality are important considerations, in addition to test performance (Table 4).
Table 4: Fall risk screening and assessment tools referred to by clinical practice guidelines

Note. AGS/BGS = American Geriatric Society/British Geriatric Society; ACSQHC = Australian Commission on Safety and Quality in Health Care; NICE: National Institute for Health and Care Excellence; RNAO: Registered Nurses’ Association of Ontario; WRHA: Winnipeg Regional Health Authority
Few multi-item screening tools mentioned the following factors: fall history, cognitive status, medications and balance, and gait and/or mobility (Table 4). It is noteworthy that CPGs often did not explicitly recommend a test/tool but provided information about its performance characteristics in appendices and left decisions about test selection to the care provider.
There was variation across CPGs with regard to components included in fall risk assessments. However, a focused fall history to determine the circumstances of the fall; detailed gait, balance, and/or mobility evaluation; medication review; vision; and environmental safety assessment were common to all CPGs. Fourteen of the 16 guidelines also included cardiovascular assessment and cognitive evaluation (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; American Medical Directors’ Association, 2011; Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Degelau et al., Reference Degelau, Belz, Bungum, Flavin, Harper and Leys2012; Health Care Association of New Jersey,, 2012; Gagnon & Lafrance, Reference Gagnon and Lafrance2011; Kim et al., Reference Kim, Jung, Kim, Kim, Cho and Kim2017; Kruschke & Butcher, Reference Kruschke and Butcher2017; National Institute for Health and Care Excellence, 2013; Naqvi, Lee & Fields, Reference Naqvi, Lee and Fields2009; Registered Nurses’ Association of Ontario, 2017; Shyamala et al., Reference Shyamala, Wong, Andiappan, Eong, Bakshi and Boey2015; Winnipeg Regional Health Authority, 2011). In acute and long-term care settings, most CPGs included urinary continence assessment. Only three CPGs included pain and/or nutrition assessment (Beauchet et al., Reference Beauchet, Dubost, Revel Delhom, Berrut and Belmin2011a; Kruschke & Butcher, Reference Kruschke and Butcher2017; Winnipeg Regional Health Authority, 2011).
Guidelines for Specific Sub-populations with Chronic Neurological Conditions
Two guidelines were identified that covered specific sub-populations (Thurman et al., Reference Thurman, Stevens and Rao2008; van der Marck et al., Reference van der Marck, Klok, Okun, Giladi, Munneke and Bloem2014). Thurman et al. (Reference Thurman, Stevens and Rao2008) provided guidance for neurologists and other staff who manage persons with chronic neurological conditions. They recommended that all persons with the following medical conditions – stroke, dementia, disorders of gait and balance, Parkinson’s disease, peripheral neuropathy – and or risk factors – lower extremity weakness or sensory loss, substantial loss of vision, and using assistive devices – are at increased risk for falls and should be asked about fall history in the previous year. Other risk factors considered include advanced age, arthritis, impairment in activities of daily living, depression, and use of psychoactive medications. It was also recommended that after the standard comprehensive neurological examination that includes evaluation of cognition and vision, if further assessment is required, the following screening measures should be considered: Timed Up-and-Go (TUG) Test or Get Up and Go test, assessment of ability to stand unassisted from a sitting position, and Tinetti Mobility Scale (Thurman et al., Reference Thurman, Stevens and Rao2008).
van der Marck et al. (Reference van der Marck, Klok, Okun, Giladi, Munneke and Bloem2014) developed recommendations for assessment and fall reduction in persons living with Parkinson’s disease. They identified 16 generic risk factors and 15 risk factors specific to persons living with Parkinson’s disease. All risk factors with the exception of visual impairment were recommended to be managed by a multidisciplinary team. Two possible approaches to implementation of the recommendations were proposed (1) one size fits all, and (2) fall type approach (i.e., identification of a specific pattern of falls such as falls preceded by freezing gait or syncope). The former proposes that all clients should be reviewed for all risk factors and managed accordingly, whereas the fall approach tries to identify the fall type for each person. Once a consistent fall pattern can be identified, the approach focusses on the specific risk factors that are implicated. The members of the task force preferred the latter approach. The authors (van der Marck et al., Reference van der Marck, Klok, Okun, Giladi, Munneke and Bloem2014) underscored that further research is needed to test the conceptual recommendation in the target population.
Discipline-Specific Guidelines
Physical therapy
Two CPGs were developed specifically for physical therapists (Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Goodwin & Briggs, Reference Goodwin and Briggs2012). Similar to non-specialized CPGs, fall risk screening recommendations included asking about a history of falls in the previous year, and gait or balance difficulties (Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Goodwin & Briggs, Reference Goodwin and Briggs2012). For individuals who reported a fall or difficulties with gait or balance, screening also included observation for gait or balance impairment (Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Goodwin & Briggs, Reference Goodwin and Briggs2012). The AGILE CPG (Goodwin & Briggs, Reference Goodwin and Briggs2012) described several tests that may be used (e.g., TUG Test, Berg Balance Scale, and Performance Oriented Mobility Assessment) for evaluation.
Avin et al. (Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015) supported the recommendation of several other CPGs that a fall risk assessment is indicated for community-dwelling older adults who screen positive for fall risk. Although the AGILE CPG (Goodwin & Briggs, Reference Goodwin and Briggs2012) did not comment on this issue, they focused on assessment of other novel components, where they recommended that older adults should be asked about their ability to get up after a fall and that they should be observed doing so if they reported that they were able to get up. Similar to other guidelines, this CPG also recommended assessing for fall-related psychological factors (e.g., fear of falling) that impact on confidence, activity restriction, and participation. The Fall Efficacy Scale (FES) and its variants were suggested as appropriate, valid, reliable, and responsive to change following interventions (Goodwin & Briggs, Reference Goodwin and Briggs2012).
Occupational therapy
Two CPGs were intended for occupational therapists and focused on the occupational therapist’s contribution to components of the fall risk assessment within their scope of practice (College of Occupational Therapists, 2015; Leland et al., Reference Leland, Elliott and Johnson2012). Both guidelines emphasized the occupational therapist’s role in home assessment and safety intervention. According to the College of Occupational Therapists (2015), a home hazard assessment and safety intervention should be offered to persons who have fallen or are at high risk of falling (e.g., history of falling, hospitalization for a fall, severe visual impairment, or functional decline). It was also recommended that occupational therapists assess fear of falling because of its link with activity restriction.
Leland et al. (Reference Leland, Elliott and Johnson2012) supported the use of standardized screening tools (e.g. TUG Test, Functional Reach, Fullerton Advanced Balance Scale) to identify an individual’s limitations that are amenable to occupational therapy intervention. These assessments allow the occupational therapist to observe and analyze occupational performance skills. Both guidelines recommended that occupational therapists provide information in an appropriate format to empower self-management and support older adults to remain safe and independent (College of Occupational Therapists, 2015; Leland et al., Reference Leland, Elliott and Johnson2012).
Discussion
The purpose of this scoping review was to describe fall risk screening and assessment approaches across the care continuum and identify gaps where more research is needed to strengthen clinical practice. Our review found similarities across guidelines related to screening and assessment content and process for identifying fall risk among older adults across all care settings. A prior history of falls and gait and balance abnormalities have been associated with increased risk of falling across care settings (Ambrose, Paul, & Hausdorff, Reference Ambrose, Paul and Hausdorff2013; Ganz, Bao, Shekelle, & Rubenstein, Reference Ganz, Bao, Shekelle and Rubenstein2007; Tinetti & Kumar, Reference Tinetti and Kumar2010). These two criteria were commonly applied either independently or sequentially in 19 fall risk screening algorithms. This finding provides reassurance to health care providers and policy makers about implementing screening and assessment recommendations in clinical practice guidelines to identify older adults at risk across care settings. This consistency should also enhance the ability to communicate fall risk across the continuum of care.
Given the heterogeneity in health as well as functional and mobility status of older adults across care settings, it is understandable that there are also differences in approaches recommended across care settings. For example, two guidelines (National Institute for Health and Care Excellence, 2013; US Preventive Services Task Force, 2018) propose alternate strategies for managing fall risk. NICE guidelines for acute care settings caution against the use of risk prediction tests, and regard all older adults at risk of falls, which varies from the approach proposed in most CPGs for community-dwelling older adults. Alternatively, the US Preventive Services Task Force (2018) does not specifically state that community-dwelling older adults should be screened for fall risk; however, they require the physician’s clinical judgement to determine if an older adult appears to be at risk and would benefit from screening followed by an in-depth assessment. These variations highlight the complex and multifactorial nature of falls that compounds identification of persons at risk. It is unlikely that a single test can predict fall risk with complete accuracy; hence a combination of approaches may be useful for determining individual risk (Lusardi et al., Reference Lusardi, Fritz, Middleton, Allison, Wingood and Phillips2017). The ideal configuration of these approaches for each care setting remains unknown; however, from this review, the authors have observed consistency in the evaluation of fall history and either questioning and/or observation of balance and/or gait. It is unlikely that a “one-size fits all” approach will match the varied capacities and circumstances of older adults across settings; but these three factors (asking about fall history and or balance/gait difficulties and observation of balance/gait) appear to be crucial across all settings.
Despite common criteria used in fall risk screening algorithms, recommendations for how to screen for gait, balance, and/or mobility problems varied across guidelines. Some guidelines recommended asking about difficulty with balance, gait, or mobility and/or observation of ambulation (American Geriatrics Society and British Geriatrics Society, 2010, Avin et al., Reference Avin, Hanke, Kirk-Sanchez, McDonough, Shubert and Hardage2015; Kruschke & Butcher, Reference Kruschke and Butcher2017; Registered Nurses’ Association of Ontario, 2017). However, it remains unclear whether one approach (self-report or observation) is superior to the other in fall prediction. This is an area for further research that also has implications for simplification of algorithms, task shifting, and time saving in care settings.
The TUG test was used for quick screening of physical and functional mobility status because of its practical utility and relative ease of administration (Australian Commission on Safety and Quality in Health Care, 2009; American Geriatrics Society and British Geriatrics Society, 2010; Kruschke & Butcher, Reference Kruschke and Butcher2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Thurman et al., Reference Thurman, Stevens and Rao2008). Despite its value as a pragmatic approach to screening, a wide range of cut-off values have been found to discriminate between those who do and those who do not fall across studies (Barry, Galvin, Keogh, Horgan, & Fahey, Reference Barry, Galvin, Keogh, Horgan and Fahey2014; Beauchet et al., Reference Beauchet, Fantino, Allali, Muir, Montero-Odasso and Annweiler2011b). The clinical utility of this test for routine screening versus other approaches such as self-report and/or observation requires further scrutiny. More research is needed to explore the feasibility and value in settings such as long-term care with more complex needs populations.
There is a paucity of literature to guide ideal timing and frequency of screening for fall risk. However, CPGs recommended fall risk screening on admission/initial contact and routinely thereafter. In acute and long-term care settings, CPGs also pointed to the need for reassessment of fall risk with significant changes in health or functional status (Australian Commission on Safety and Quality in Health Care, 2009; Registered Nurses’ Association of Ontario, 2017; Scott et al., Reference Scott, Bawa, Feldman, Sims-Gould, Leung and Tan2010; Winnipeg Regional Health Authority, 2011). Some studies also document that an increased risk for falls occurs during transfers and move to a new environment (Johnson, George, & Tran, Reference Johnson, George and Tran2011; Rice, Ousley, & Sosnoff, Reference Rice, Ousley and Sosnoff2015). These observations emphasize the importance of recognizing critical points of vulnerability during the care journey that warrant vigilance and intervention to prevent falls.
The timing and frequency of fall risk screening and assessment was also influenced by practical considerations such as the need to integrate fall risk screening with other admission and care processes in order to enhance compliance and reduce staff burden of administration. Further work to understand how best to integrate fall risk screening and assessment into person-centered standardized assessments and care processes such as Minimum Dataset-Resident Assessment Instrument (MDS-RAI) and Transferring Lifting Repositioning (TLR) would be beneficial.
There is heterogeneity across guidelines about the components that should be assessed as part of the fall risk assessment in older adults across the care continuum. Guidelines supported inclusion of the following factors: detailed fall history; medication review; balance, gait, and/or mobility; vision; cognitive status; postural hypotension; and environmental assessment for hazards. The multifactorial nature of fall risk requires a comprehensive assessment to identify risk factors tailored to the individual’s specific circumstances and integrated within an interprofessional and holistic approach to care. The integration of fall risk identification into intake/admission assessment including routine history and physical examination would potentially streamline the process of data gathering and improve identification and documentation of fall risks. Although the model for assessment may vary by setting and the health status of the individual, the overlap in components across guidelines suggests potential core domains (i.e., detailed fall history; medication review balance, gait, and/or mobility; vision; cognitive status; postural hypotension; and environmental assessment for hazards) for evaluation across settings. We note that there are similar core domains for both screening and assessment: fall history and balance and gait. Additional components may still need to be considered in particular care settings depending on the population. It is encouraging that current guidelines across disciplines, conditions, and care settings do report a similar set of screening and assessment components. This supports that processes can be the same across the continuum despite variation in tools/tests specific to the needs of the population. More work is needed to further delineate the primary components of the comprehensive assessment and link guidelines to implementation for better outcomes.
The availability of clinical practice guidelines for specific disciplines and conditions is an emerging and encouraging trend. It facilitates shared responsibility and supports enhanced capacity for fall risk screening and assessment across health care providers. More work is needed to expand this nascent body of research, engage more disciplines, and cover more sub-populations with increased risk for falls. Work could be advanced with a unified approach to development of core guidelines that were broadly applicable; individual disciplines and condition-specific considerations could be added as needed.
This review had several strengths including the development of a comprehensive search strategy that covered diverse information sources that were likely to capture clinical practice guidelines and best practice recommendations relevant to multiple disciplines. More recent publications were targeted in order to identify the best current evidence to inform our local work. However, there were some limitations that constrained our findings. Only articles published in the English language were considered for inclusion. There may have been relevant guidelines published in other languages that were missed. Additionally, although the review identified a few guidelines intended for specific subpopulations such as people living with Parkinson’s diseases, the potential exists that others may not been captured without a specific search strategy designed to identify those groups. It was also noted that only three of the guidelines had been revised within the past 5 years. This suggests that limited current evidence might be available to inform practice. Guidelines were developed in high-income countries; hence applicability for low-income and resource-limited settings should be questioned. The overwhelming emphasis of existing guidelines on implementation of interventions offered limited information on the topic of the scoping review. There was also considerable uncertainty because of limited evidence in some areas such as ideal frequency of screening.
Conclusions
There were 22 CPGs and best practice recommendations that inform care providers across the continuum of care; although most pertained to community-dwelling older adults. Approaches to screening for fall risk consistently included history of falls and reported and/or demonstrated gait, balance, and/or mobility impairment. Although components included in the fall risk assessment varied, guidelines emphasized the need for an individualized approach to risk reduction with identification of risk factors and implementation of appropriate interventions. More research is needed to identify the ideal frequency for ongoing screening and assessment across settings. Work is also needed to support implementation and sustainability of guidelines and identify the factors influencing health care providers’ ability to incorporate best practices in their care settings.










