Introduction
Sex differences in schizophrenia have been described in almost all features of the illness, including incidence, prevalence, age at onset, symptomatology, course, and in the response to treatment, but only reliably established in age at onset and course [Reference Riecher-Rössler, Butler and Kulkarni1]. Sex-related differences in the illness course might be at least partially mediated by sex-related differences in cognitive functioning [Reference Mendrek and Mancini-Marie2]. Reduced cognitive performance is one of the core features of schizophrenia and an important predictor of outcome [Reference Kahn and Keefe3]. Several studies have shown neurocognitive deficits already in patients with a so-called at-risk mental state (ARMS) for psychosis [Reference Hauser, Zhang, Sheridan, Burdick, Mogil and Kane4]. Furthermore, it has been found that ARMS patients with later conversion to psychosis performed worse at baseline in tests measuring attention/vigilance, speed of processing, verbal and visual learning, and current and premorbid IQ compared with patients who did not convert [Reference Hauser, Zhang, Sheridan, Burdick, Mogil and Kane4]. Consequently, several studies have shown that the prediction of transition to psychosis can be improved by including neurocognitive performance measures into multivariable risk prediction models [4–8].
Cognitive performance is not only dependent on different stages of psychotic disorders, but also on sex. In healthy controls (HC), it is well established that women tend to perform better than men in tasks measuring verbal abilities (d = 0.24; for meta-analysis, see reference [Reference Hyde9]), whereas men tend to outperform women on visual–spatial tasks (d = 0.45; for meta-analysis, see [Reference Hyde9]) [10–12]. Most studies indicate that these differences are also maintained in patients with schizophrenic psychoses (for reviews, see references [Reference Riecher-Rössler, Butler and Kulkarni1,Reference Mendrek and Mancini-Marie2]). Specifically, many studies have shown that women diagnosed with schizophrenia have a better performance in verbal learning and memory [Reference Riecher-Rössler, Butler and Kulkarni1,Reference Zhang, Han, Zhang, Hui, Jiang and Yang13,Reference Bozikas, Kosmidis, Peltekis, Giannakou, Nimatoudis and Karavatos14]. The female advantage in verbal domains has also been found in patients with first-episode psychosis (FEP), while men showed a better performance in tests of reaction time, visual memory, and executive functions [Reference Riecher-Rössler, Butler and Kulkarni1,Reference Ittig, Studerus, Papmeyer, Uttinger, Koranyi and Ramyead10].
The impact of sex on cognitive functioning in ARMS has received considerable attention in the literature in recent years. A meta-regression analysis based on 19 studies assessing neuropsychological performance in 1,188 ARMS patients (women, n = 523; 44%) and 1,029 HC (women, n = 464; 45%) showed a trend-level significance effect of sex on cognitive performance, with females performing relatively better than males [Reference Fusar-Poli, Deste, Smieskova, Barlati, Yung and Howes15]. Our own group investigated sex differences in cognitive functioning in 118 ARMS patients (women, n = 45; 38%), 88 FEP patients (women, n = 32; 36%), and 86 HC (women, n = 41; 47%) [Reference Ittig, Studerus, Papmeyer, Uttinger, Koranyi and Ramyead10]. Women performed better in the domain of verbal learning and memory whereas men showed a shorter reaction time during the working memory task across all groups. However, these differences did not withstand correction for multiple testing. Taken together, existing studies indicate that female patients with psychotic disorders or being at clinical high risk for psychosis do not perform better than males over and above what we see in HC.
To the best of our knowledge, the present study is the first to investigate sex differences in cognitive functioning in a large multinational sample of ARMS patients by using an extended neuropsychological battery and a healthy comparison group. The goal of the study was to elucidate whether sex differences in cognitive functioning differ between ARMS and HC subjects. Based on the evidence above and our own findings, we expected a better performance of women in the domain of verbal learning and memory irrespective of group.
Methods
Setting and recruitment
The neuropsychological data analyzed in this study were collected within the EUropean Gene–Environment Interactions (EU-GEI) study, which aims to identify the interactive genetic, clinical, and environmental determinants of schizophrenia [Reference Kraan, Velthorst, Themmen, Valmaggia, Kempton and McGuire16]. EU-GEI is a naturalistic prospective multicenter study that consisted of a baseline and up to three follow-up time points (at 6 months, 12 months, and 24 months). Data were collected from May 1, 2010 to August 6, 2015. For the current analyses, only baseline data, that is, at intake into the study, were used.
ARMS participants were recruited from 11 Early Detection and Intervention Centers (London, Amsterdam, The Hague, Vienna, Basel, Cologne, Copenhagen, Paris, Barcelona, Melbourne, Saõ Paulo). They were referred to the EU-GEI study by primary health care services, mental health professionals, or themselves or their families.
Control participants were recruited by four of the above-mentioned centers: the Institute of Psychiatry, Psychology, and Neuroscience (IoPPN) in London, the Personal Assessment and Crisis Evaluation Clinic in Melbourne, and the Amsterdam Medical Center and Parnassia, The Hague. They were approached by telephone and through advertisements at educational institutes. In Melbourne, controls were additionally approached at community centers/noticeboards and advertised via online platforms. Controls were matched to the ARMS patients in terms of age, sex, migrant, and ethnic status. All participants were screened with an inclusion/exclusion checklist (see below).
The protocol of the EU-GEI study was approved by the institutional review boards of all study sites. EU-GEI was conducted in accordance with the Declaration of Helsinki. The Medical Ethics Committees of all participating sites approved the study protocol.
Inclusion and exclusion criteria
Inclusion criteria for ARMS patients were: aged 14–45 (most of them were between 18 and 35 years); being at-risk for psychosis as defined by the comprehensive assessment of at-risk mental state (CAARMS) [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell'Olio17]; adequate language skills corresponding to each center; and consent to study participation. The exclusion criteria were: prior experience of a psychotic episode of more than 1-week as determined by the CAARMS [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell'Olio17] and Structural Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM Disorders (SCID)) [Reference Wittchen, Zauding and Fydrich18]; previous treatment with an antipsychotic for a psychotic episode; and IQ < 60.
Inclusion criteria for controls were: aged 18–35; adequate language skills local to each center; no evidence of current or past psychosis (including treatment with antipsychotic medication). Exclusion criteria for controls were similar to those for ARMS participants. Additionally, controls were excluded if they met the criteria for an ARMS status as defined by the CAARMS [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell'Olio17].
Detection procedure
The CAARMS was used to identify ARMS patients [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell'Olio17]. The CAARMS is a semi-structured interview that encompasses psychotic symptoms and a range of other psychopathological symptoms present during the psychosis prodrome. Individuals were classified as being in an ARMS for psychosis if they met at least one of the following risk criteria: (i) attenuated psychotic symptoms (psychotic symptoms subthreshold either in intensity or frequency); (ii) brief limited psychotic symptoms (recent episode of brief psychotic symptoms that spontaneously resolved within 1 week); or (iii) vulnerability group (a first-degree relative with a psychotic disorder or a diagnosis of a schizotypal personality disorder in combination with a significant drop in functioning). The full criteria can be found elsewhere [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell'Olio17].
Assessment of sociodemographic and clinical characteristics
Sociodemographic characteristics (e.g. age, sex, ethnicity) were obtained using the modified Medical Research Council sociodemographic schedule [Reference Mallett19]. Current cannabis frequency was assessed with the modified version of the Cannabis Experience Questionnaire [Reference Barkus, Stirling, Hopkins and Lewis20]. Data on comorbid affective and anxiety disorders were assessed with the SCID [Reference Wittchen, Zauding and Fydrich18]. Psychiatric medication (i.e., use of antipsychotics, antidepressants, and sedatives) was obtained using a medical history questionnaire, designed by the EU-GEI group. The general level of functioning was assessed with the modified version of the Global Assessment of Functioning (GAF) scale [Reference Goldman, Skodol and Lave21].
Classification and assessment of neuropsychology
Neuropsychological performance of each participant was assessed by trained psychiatrists, psychologists, and research assistants. The neuropsychological tests covered the following seven domains: attention/vigilance, reasoning/problem solving, speed of processing, verbal learning, working memory, social cognition, and current IQ. Test scores were assigned to cognitive domains in accordance with Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB) [Reference Green, Nuechterlein, Gold, Barch, Cohen and Essock22]. Tests that are not part of the MCCB were assigned to domains according to their most commonly used function. The following measures were used to cover the cognitive domains of interest:
• Attention/vigilance: Digit Span Forward subtest of the Wechsler Adult Intelligence Scale-third edition (WAIS-III) [Reference Wechsler23];
• Reasoning/problem solving: Beads Task [Reference Huq, Garety and Hemsley24];
• Speed of processing: Digit Symbol Test of the WAIS-III and the Trail-Making Test parts A and B [Reference Battery25];
• Verbal Learning: Rey Auditory Verbal Learning Test [Reference Rey26];
• Working memory: Digit Span Backwards and Arithmetic subtests of the WAIS-III [Reference Wechsler23];
• Social cognition: Degraded Affect Recognition Task [Reference van't Wout, Aleman, Kessels, Laroi and Kahn27] and the Benton Facial Recognition Test [Reference Benton, Silvan, Hamsher, Varney and Spreen28]; and
• Current IQ: Block Design total raw score, the information total raw score and the estimate of the total IQ of the shortened WAIS-III [Reference Wechsler23,Reference Velthorst, Levine, Henquet, De Haan, Van Os and Myin-Germeys29].
Assessment of psychopathology
The Brief Psychiatric Rating Scale expanded version (BPRS-E) [Reference Ventura, Lukoff, Nuechterlein, Liberman, Green and Shaner30] was used to assess psychopathology. Sex differences were investigated using the BPRS total score and the following subscales: BPRS positive symptoms and BPRS negative symptoms [Reference Shafer, Dazzi and Ventura31].
Statistical analyses
All statistical analyses were performed using R [32]. Because observations were nonindependent, that is, observations from the same center were more similar than observations from different centers, sex differences were analyzed using linear mixed effects models including sex and group (ARMS, HC) as a fixed effects factors and randomly varying intercepts per center to account for the clustering in the data. Linear mixed effects models were applied to evaluate the main effects of sex and group (ARMS, HC) as well as their interactions on cognitive functioning. Dependent variables were z-transformed before inclusion to models and sex was included as a binary variable with 0 and 1 describing men and women, respectively. Thus, the regression coefficient for sex described the standardized mean difference (SMD) of women compared with men. The results are presented with and without correction for multiple testing. We used the false discovery rate procedure to adjust p-values for multiple testing [Reference Benjamini and Hochberg33].
Results
Sample description
The sample of the present study consisted of 343 ARMS patients (185 men, 158 women) and 67 HC subjects (34 men, 33 women). Sociodemographic and clinical characteristics of our sample are presented in Table 1. Cannabis use was more frequent in male ARMS patients than female ARMS patients (30.51% vs. 18.46% used cannabis at least a few times per year). With regard to comorbid affective and anxiety disorders, female ARMS patients showed more often a current anxiety disorder as well as posttraumatic stress disorders (PTSD) compared with male ARMS patients. There were no significant sex differences regarding any current affective disorder (i.e., current depressive, manic, or hypomanic episode and dysthymic disorder), neither for ARMS nor for HC. With regard to psychopathology, male ARMS patients showed significantly more severe BPRS “negative symptoms” (p = 0.006) than female ARMS patients. There were no sex differences in ARMS and HC with regard to age, years of education, current psychiatric medication, global functioning, BPRS “positive symptoms” and BPRS “total score.”
Table 1. Sociodemographic and clinical sample characteristics

Abbreviations: ARMS, at-risk mental state; BPRS, Brief Psychiatric Rating Scale; GAF, Global Assessment of Functioning; HC, healthy controls; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder.
Continuous variables are described by means and standard deviation in brackets.
* p < 0.05.
** p < 0.01.
Effects of sex and diagnostic group on cognitive functioning
Means and standard deviations (SD) of the total group, ARMS, and HC are presented in Table 2. Table 3 shows the results of the mixed effects models using neurocognitive performance as the continuous dependent variable and sex as well as group (ARMS, HC) as fixed effects factors. SMDs of the neuropsychological measures are additionally presented in Figure 1.
Table 2. Means and standard deviations of neuropsychological test data in ARMS patients and HC
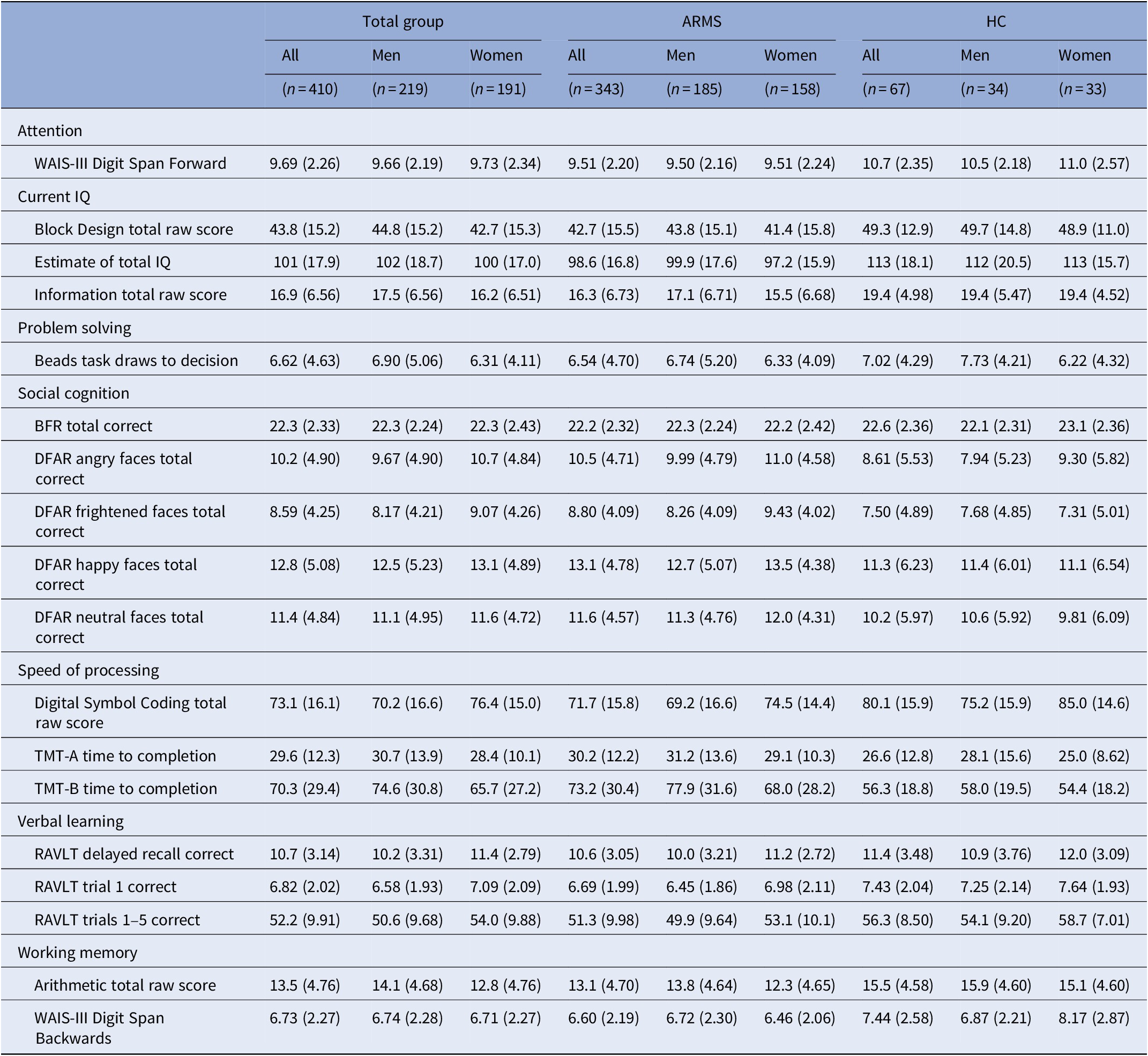
Abbreviations: ARMS, at-risk mental state; BFR, Benton Facial Recognition Test; DFAR, Degraded Facial Affect Recognition Task; HC, healthy controls; RAVLT, Rey Auditory Verbal Learning Test; TMT, Trail Making Test; WAIS, Wechsler Adult Intelligence Scale.
Table 3. p values and coefficients of fixed effects of mixed effects models

Abbreviations: BFR, Benton Facial Recognition Test; coef, y-standardized regression coefficients of fixed effects; DFAR, Degraded Facial Affect Recognition Task; RAVLT, Rey Auditory Verbal Learning Test; TMT, Trail Making Test; WAIS, Wechsler Adult Intelligence Scale.
a Corrected for multiple testing using Benjamini–Hochberg method.
* p < 0.05.
** p < 0.01.
*** p < 0.001.
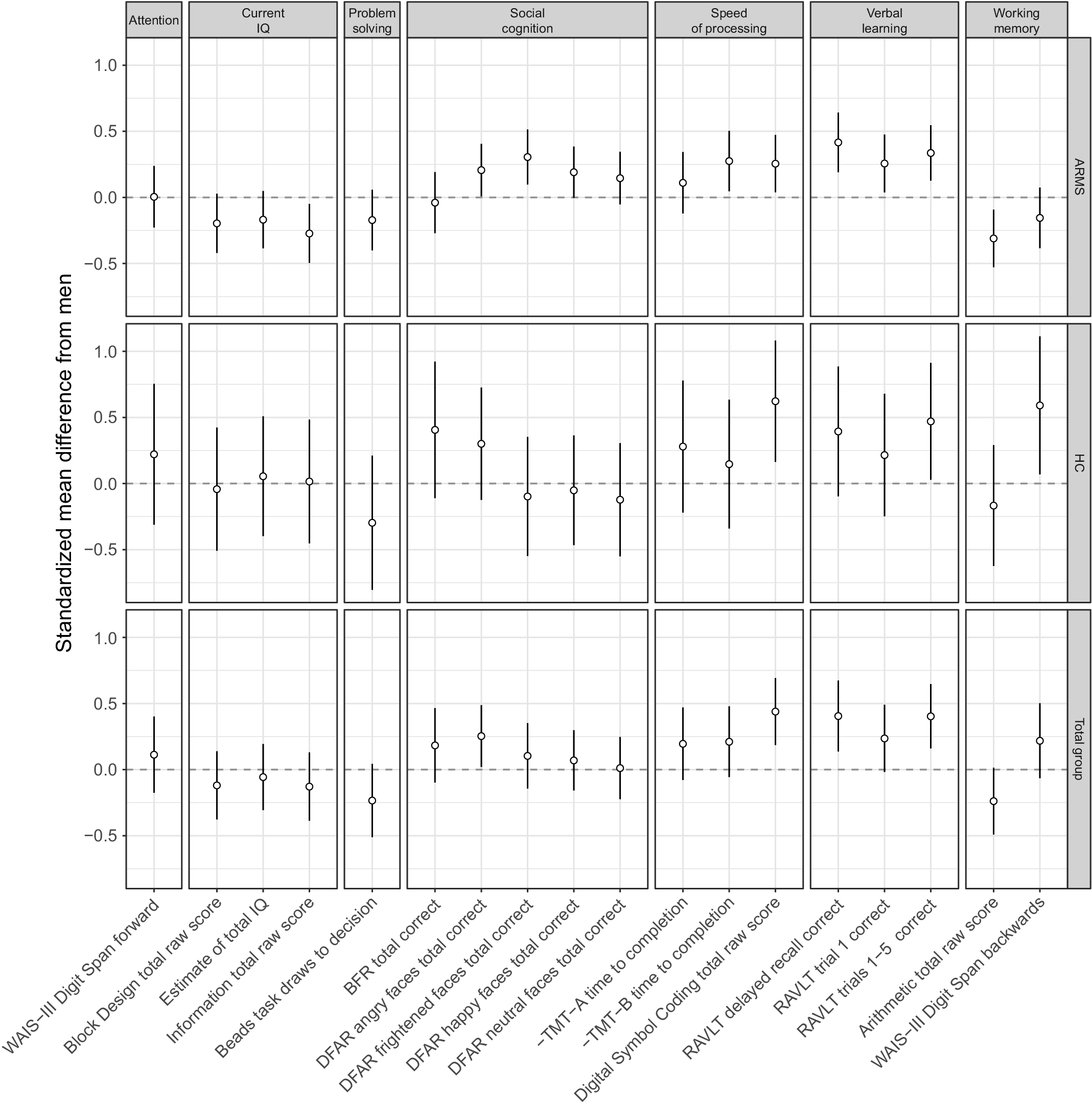
Figure 1. Cognitive performance of women compared with men in at-risk mental state for psychosis individuals and healthy controls. The dotted horizontal line at zero represents the performance of men. Differences are expressed in units of standard deviation and are significant if the 95% confidence interval (vertical line) does not overlap with zero. Variables with a minus sign were reversed so that positive scores always represent good performance. Abbreviations: RAVLT, Rey Auditory Verbal Learning Test; TMT, Trail Making Test; WAIS, Wechsler Adult Intelligence Scale.
In the combined sample of ARMS and HC, women recognized more angry faces in the “Degraded Faces Affect Recognition” social cognition task (p = 0.034, b = 0.25), performed better in the “Digital Symbol Coding” speed of processing task (p ≤ 0.001, b = 0.44) of the WAIS-III, and remembered more words in the “Rey Auditory Verbal Learning Test (RAVLT) delayed recall” (p = 0.003, b = 0.41) and “RAVLT trials 1 to 5” (p = 0.001, b = 0.40) than men. However, after correction for multiple testing, only the differences in “Digital Symbol Coding” and the RAVLT measures remained statistically significant.
Effects of diagnostic group are presented in Table 3. ARMS patients performed significantly worse in all cognitive performance scores, except in all scores of the problem solving and social cognition tasks.
There was one statistically significant interaction between sex and group (ARMS, HC) on the “WAIS-III Digit Span Backwards” working memory task (p = 0.011), which was due to a significantly better performance of female HC compared with male HC (p < 0.026, b = −0.59) and a nonsignificantly worse performance of female ARMS patients compared with male ARMS patients (p = 0.186, b = 0.16). However, this sex × group interaction was no longer significant after correction for multiple testing.
The results did not change, when age or frequent cannabis use (i.e., at least several times per week) were included as covariates.
Discussion
To the best of our knowledge, this is the first study investigating sex-related neurocognitive performance differences in a multinational ARMS sample of this size, using a comprehensive neuropsychological battery and a healthy comparison group. In line with our hypotheses, women showed superior performance in the domain of verbal learning and memory independent of whether they were ARMS patients or HC. Furthermore, women outperformed men on measures of speed of processing (i.e., Digital Symbol Coding total raw score) and social cognition (i.e., Degraded Facial Affect Recognition Task (DFAR) angry faces total correct), whereas men outperformed women on a trend-wise level on a task of working memory (i.e., arithmetic total raw score). Additionally, our results show that ARMS patients displayed alterations in attention, current IQ, speed of processing, verbal learning, and working memory compared with HC. However, we will not discuss this aspect any further since it is not the focal point of the present study.
Finally, we found a sex × group interaction effect on working memory (i.e., WAIS-III Digit Span Backwards), which was due to a significantly better performance of female HC compared with male HC and a nonsignificantly better performance of male ARMS patients compared with female ARMS patients. However, only sex differences in the total group in speed of processing and verbal learning remained significant after correction for multiple testing.
With regard to verbal learning and memory, our finding that the female advantage is equally present in ARMS patients as in HC is in line with previous research [Reference Riecher-Rössler, Butler and Kulkarni1,Reference Fusar-Poli, Deste, Smieskova, Barlati, Yung and Howes15]. Furthermore, it corroborates the findings of an earlier study of our own group that reported no interaction effect between diagnostic group (i.e., ARMS, FEP, HC) and verbal learning and memory [Reference Ittig, Studerus, Papmeyer, Uttinger, Koranyi and Ramyead10].
Regarding processing speed, our finding that women perform better than men is also consistent with earlier findings from the general population [Reference Burns and Nettelbeck34,Reference Jorm, Anstey, Christensen and Rodgers35] and patients with schizophrenia [Reference Vaskinn, Sundet, Simonsen, Hellvin, Melle and Andreassen36,Reference Torniainen, Suvisaari, Partonen, Castaneda, Kuha and Perala37]. To the best of our knowledge, this is the first study examining sex differences in ARMS and healthy subjects by using well-established tests to evaluate processing speed (i.e., Trail Making Test, WAIS-III Digit Symbol subtest). A previous study has investigated sex-related cognitive performance differences in ARMS, FEP and HC but did not include tests specifically measuring processing speed [Reference Ittig, Studerus, Papmeyer, Uttinger, Koranyi and Ramyead10]. However, the authors found a shorter reaction time for men in the working memory task independent of diagnostic group. They explain the findings by a superior working memory performance rather than generally enhanced processing speed in men as no sex differences in reaction time during the Continuous Performance Test and the Go/No-Go subtest of the Test of Attentional Performance (TAP) were detected, while maintaining a comparable overall working memory performance level [Reference Ittig, Studerus, Papmeyer, Uttinger, Koranyi and Ramyead10].
A strength of our study is that we examined sex differences with well-established tests using the classification of the MATRICS panel [Reference Green, Nuechterlein, Gold, Barch, Cohen and Essock22,Reference Nuechterlein, Green, Kern, Baade, Barch and Cohen38]. As the MCCB domains are well known in schizophrenia research, this may help future studies to compare sex-related cognitive performance differences in ARMS and schizophrenic patients. Furthermore, this is the first study to investigate sex differences in cognitive functioning in an ARMS sample of this size.
However, there are some limitations to the present study that need to be acknowledged. Our neuropsychological test battery was originally selected to identify genetic and environmental interactions in psychosis and not specifically to detect sex differences. Accordingly, the test battery did not include other sensitive tasks to detect sex differences such as visuo-spatial tasks. Additionally, the domain of visual learning in the MATRICS consensus battery was not covered. Furthermore, our control group was rather small in comparison to the ARMS group, which reduced the statistical power to detect interaction effects between sex and group. Finally, it is important to note that sex-related cognitive performance differences depend on a wide variety of conditions, for example, the severity of symptoms and especially the fluctuation of estrogen levels during the menstrual cycle in women (for review, see reference [Reference Riecher-Rössler, Butler and Kulkarni1]). There is evidence that high levels of estrogen at the mid-luteal point are associated with better verbal memory and diminished spatial ability [Reference Hampson39]. Thus, it is possible that some effects would have changed if we had measured women at a specific time point during their monthly cycle. Unfortunately, in our study no assessment of the time point during the monthly cycle was performed.
Taken together, our findings indicate that sex differences in cognitive functioning in ARMS patients are very similar to those seen in the general population and in schizophrenia patients.
Acknowledgments
We thank all patients who participated in the study as well as the referring specialists.
Financial Support
This work was supported by the European Union (European Community’s Seventh Framework Program [grant number HEALTH-F2-2010-241909; Project EU-GEI]). M.J.K. was supported by a Medical Research Council Fellowship (grant number MR/J008915/1). N.B.-V. was supported by the Ministerio de Ciencia, Innovación e Universidades (PSI2017-87512-C2-1-R) and the Generalitat de Catalunya (2017SGR1612 and ICREA Academia Award). The French cohort was supported by the French Ministry grant (PHRC AOM07-118) and by Fondation Pierre Deniker (CMLF). B.P.R. was supported by the Netherlands Organization for Scientific (VIDI grant number 91718336).
Conflict of Interest
All authors declare not to have any conflicts of interest that might be interpreted as influencing the content of the manuscript.
Appendix
EU-GEI High Risk Study Group—Author List
Philip McGuire2, Lucia R. Valmaggia3, Matthew J. Kempton2, Maria Calem2, Stefania Tognin2, Gemma Modinos2, Lieuwe de Haan4,7, Mark van der Gaag8,10, Eva Velthorst5,11, Tamar C. Kraan6, Daniella S. van Dam4, Nadine Burger7, Barnaby Nelson12,13, Patrick McGorry12,13, G. Paul Amminger12,13, Christos Pantelis14, Athena Politis12,13, Joanne Goodall12,13, Anita Riecher-Rössler1, Stefan Borgwardt1, Charlotte Rapp1, Sarah Ittig1, Erich Studerus1, Renata Smieskova1, Rodrigo Bressan15, Ary Gadelha15, Elisa Brietzke16, Graccielle Asevedo15, Elson Asevedo15, Andre Zugman15, Neus Barrantes-Vidal17, Tecelli Domínguez-Martínez18, Anna Racioppi19, Lídia Hinojosa-Marqués19, Thomas R. Kwapil20, Manel Monsonet19, Mathilde Kazes21, Claire Daban21, Julie Bourgin21, Olivier Gay21, Célia Mam-Lam-Fook21, Marie-Odile Krebs21, Dorte Nordholm22, Lasse Randers22, Kristine Krakauer22, Louise Glenthøj22, Birte Glenthøj23, Merete Nordentoft22, Stephan Ruhrmann24, Dominika Gebhard24, Julia Arnhold25, Joachim Klosterkötter24, Gabriele Sachs26, Iris Lasser26, Bernadette Winklbaur26, Philippe A. Delespaul27,28, Bart P. Rutten29, and Jim van Os29,30.
Affiliations
1University Psychiatric Hospital, CH-4002 Basel, Switzerland; 2Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London SE5 8AF, United Kingdom; 3Department of Psychology, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London SE5 8AF, United Kingdom; 4Amsterdam UMC, University of Amsterdam, Psychiatry, Department Early Psychosis, Amsterdam, The Netherlands; 5Department of Psychiatry and Seaver Center for Research and Treatment, Icahn School of Medicine at Mount Sinai, New York, USA; 6Mental Health Institute Arkin, Amsterdam, The Netherlands; 7Arkin Amsterdam; 8VU University, Faculty of Behavioral and Movement Sciences, Department of Clinical Psychology and Amsterdam Public Mental Health Research Institute, 1081 BT Amsterdam, The Netherlands; 9Mental Health Institute Noord-Holland Noord, Hoorn, The Netherlands; 10Parnassia Psychiatric Institute, Department of Psychosis Research, 2512 HN The Hague, The Netherlands; 11Early Psychosis Section, Department of Psychiatry, Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands; 12Orygen, The National Centre of Excellence in Youth Mental Health, University of Melbourne, Melbourne, Australia; 13Centre for Youth Mental Health, University of Melbourne, Parkville, Victoria 485 3052, Australia; 14Melbourne Neuropsychiatry Centre, The University of Melbourne, Melbourne, Australia; 15LiNC—Lab Interdisciplinar Neurociências Clínicas, Depto Psiquiatria, Escola Paulista de Medicina, Universidade Federal de São Paulo—UNIFESP, São Paulo, Brazil; 16Depto Psiquiatria, Escola Paulista de Medicina, Universidade Federal de São Paulo—UNIFESP, São Paulo, Brazil; 17Departament de Psicologia Clínica i de la Salut (Universitat Autònoma de Barcelona), Fundació Sanitària Sant Pere Claver (Spain), Spanish Mental Health Research Network (CIBERSAM), Spain; 18CONACYT-Dirección de Investigaciones Epidemiológicas y Psicosociales, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz, Mexico; 19Departament de Psicologia Clínica i de la Salut (Universitat Autònoma de Barcelona), Bellaterra, Spain; 20Department of Psychology, University of Illinois at Urbana-Champaign, Urbana, Illinois, USA; 21University Paris Descartes, GHU Paris Sainte-Anne, C’JAAD, Service Hospitalo-Universitaire, Inserm 1266, Institut de Psychiatrie (CNRS 3557) Paris, France; 22Mental Health Center Copenhagen and Center for Clinical Intervention and Neuropsychiatric Schizophrenia Research, CINS, Mental Health Center Glostrup, Mental Health Services in the Capital Region of Copenhagen, University of Copenhagen, Copenhagen, Denmark; 23Centre for Neuropsychiatric Schizophrenia Research (CNSR) & Centre for Clinical Intervention and Neuropsychiatric Schizophrenia Research (CINS), Mental Health Centre Glostrup, University of Copenhagen, Glostrup, Denmark; 24Department of Psychiatry and Psychotherapy, University of Cologne, Cologne, Germany; 25Psyberlin, Berlin, Germany; 26Medical University of Vienna, Department of Psychiatry and Psychotherapy, Vienna, Austria; 27Department of Psychiatry and Neuropsychology, School for Mental Health and Neuroscience, Maastricht University Medical Centre, 6200 MD 464 Maastricht, The Netherlands; 28Mondriaan Mental Health Trust, 4436 CX Heerlen, The Netherlands; 29Medical University of Vienna, Department of Psychiatry and Psychotherapy; 30Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London SE5 8AF, United Kingdom.









Comments
No Comments have been published for this article.