Introduction
Cognitive behavioural therapy (CBT) is considered a first-line treatment for a range of mental health problems (Gratzer, Reference Gratzer2020) and training as a CBT therapist has become a popular career choice for many psychology graduates and health and social care professionals (Moya, Reference Moya2022). Uptake of training places has been influenced in part, by the roll-out of the adult Improving Access to Psychological Therapies (IAPT) programme in England back in 2008 (see Clark, Reference Clark2011) known more recently as Talking Therapies for Anxiety and Depression (TTAD; National Collaborating Centre for Mental Health, 2019). Additionally, ‘The Matrix’ in Scotland (National Health Service Education for Scotland, NES, 2011) and ‘Matrics Cymru’ in Wales, recommend CBT as the main evidence-based treatment for several mental health disorders (National Psychological Therapies Management Group and Public Health Wales, 2016) leading to increasing numbers choosing to train in this modality.
IAPT expanded over subsequent years to include both children and young people’s and severe mental health problems training routes, and some clinical psychology doctorates now include a CBT training pathway (Rodwell et al., Reference Rodwell, Kent and Hale2023). Funding for CBT training posts varies across the United Kingdom and for those who can access them, it provides individuals with opportunities for career development, such as moving from secondary to primary care or a job with a higher pay banding. Once accepted onto training courses, novice practitioners are often taught a homogeneous curriculum informed by NICE guidelines, national accrediting body standards and disorder-specific models (e.g. BABCP, 2023; National Institute for Health and Clinical Excellence, 2009; Ehlers & Clark, Reference Ehlers and Clark2000). Except for the clinical psychology route, courses usually take place over one or two years, and trainees must balance the acquisition of considerable theoretical learning about CBT models and interventions (‘declarative knowledge’) with displays of emerging practical aptitude and skill (‘procedural knowledge’) in their work with clients (Bennett-Levy, Reference Bennett-Levy2006; Liness et al., Reference Liness, Beale, Lea, Byrne, Hirsch and Clark2019).
Who trains in CBT and what problems do they encounter along the way?
With a higher number of trainees being recruited, the demographic of candidates has broadened since the inception of IAPT, as practitioners move from professional backgrounds such as clinical psychology, mental health nursing, social work, occupational therapy, counselling and non-‘core professions’ such as Psychological Wellbeing Practitioner (PWP; Liness et al., Reference Liness, Beale, Lea, Byrne, Hirsch and Clark2019). The demands of transitioning to CBT have been described in a comedic fashion as ‘cognitive therapy training stress disorder’ (Worthless et al., Reference Worthless, Competent and Lemonde-Terrible2002), yet the process is hypothesised to invoke a range of schematic, interpersonal, intrapersonal, emotional and contextual challenges (Robinson et al., Reference Robinson, Kellett, King and Keating2012; Roscoe et al., Reference Roscoe, Bates and Blackley2022; Wilcockson, Reference Wilcockson2020; Wilcockson, Reference Wilcockson2022; Wolff and Auckenthaler, Reference Wolff and Auckenthaler2014). For example, high-intensity CBT training is often high-intensity by name and by nature, typically consisting of a three day per week placement, workplace and university-based supervision, written assignments and audio or video assessment of therapeutic skills (Owen et al., Reference Owen, Crouch-Read, Smith and Fisher2021). Previous research has identified both common role transition difficulties and those that are unique to different professional groups during training and post-qualification (Wilcockson, Reference Wilcockson2020; Wilcockson, Reference Wilcockson2022).
Common and profession-specific challenges during training
Loss of identity
For those undertaking CBT training there are likely to be role transition challenges that are both shared (e.g. loss of identity, professional competence), and specific to each profession. PWPs for example, lose a high level of familiarity with low-intensity formulations and interventions and a certain style of working with clients (e.g. didactic with emphasis on psychoeducation). In contrast, CBT training often involves the adoption of a different style of client interaction, with more emphasis on guided discovery and collaboration (Padesky, Reference Padesky1993; Roscoe et al., Reference Roscoe, Bates and Blackley2022). Others will be giving up a role of seniority (e.g. mental health nurses) and with it, role power (e.g. where they supervised others and now face the prospect of being the supervisee again; Corrie and Lane, Reference Corrie and Lane2015; Rønnestad and Skovholt, Reference Rønnestad and Skovholt2003). Moving to a work context such as TTAD, some trainees can face the loss of support from working in a multi-disciplinary team, more common in secondary care (Robinson et al., Reference Robinson, Kellett, King and Keating2012). Furthermore, the context in which one trains might impact upon the speed of the transition. For example, many CBT therapists will start ‘afresh’ in new teams and in new areas where it is easier to relinquish previous job activities. This is not always the case with some CBT training courses such as those that train eating disorders clinicians, where practitioners continue to hold dual roles (e.g. nurse ‘case manager’ and trainee CBT therapist) (Robinson et al., Reference Robinson, Kellett, King and Keating2012).
Feeling ‘deskilled’
There are very few studies that have been conducted on role transition during CBT training, and those that exist have tended to use small sample sizes ranging from six to 20 participants. For example, Robinson et al. (Reference Robinson, Kellett, King and Keating2012) conducted semi-structured interviews with (n=6) mental health nurses who had completed IAPT ‘high-intensity’ training. Thematic analysis revealed a general sense of participants feeling deskilled early in the training course. One of the sub-themes ‘clinging to old roles’ captured a tendency for some participants to resort to using ‘safety-seeking behaviours’ (e.g. using nursing skills) when they felt anxious or lacking in confidence. Elsewhere, Wilcockson (Reference Wilcockson2020) analysed reflective reports from (n=21) former IAPT trainees and used grounded theory to develop models of role transition for different professional groups. For example, in the nursing group, there was a sense that CBT was a natural career progression, yet CBT was more technically and emotionally demanding than they had anticipated. Specific aspects of nursing practice such as knowledge of medications were maintained through the role transition process.
Orientation to CBT
Trainees who are coming from another psychotherapeutic orientation (e.g. person-centred counselling) have been found to experience value conflicts, with CBT theories raising questions about one’s ontological and epistemological positioning (Neimeyer and Morton, Reference Neimeyer and Morton1997). For example, CBT is typically associated with a rationalist/positivist worldview due to its alignment with diagnostic classification systems and emphasis on psychometric measures to evaluate therapeutic outcomes (Lee et al., Reference Lee, Neimeyer and Rice2013; Neimeyer and Morton, Reference Neimeyer and Morton1997; Wilcockson, Reference Wilcockson2020) and with empiricism due to the collaborative basis of behavioural experiments that are undertaken during therapy (Bennett-Levy et al., Reference Bennett-Levy, Westbrook, Fennell, Cooper, Rouf and Hackmann2004). Conversely, person-centred counselling is thought to be more closely aligned to a constructivist worldview where there is greater focus on meaning making, development of insight and a non-directive style (Lee et al., Reference Lee, Neimeyer and Rice2013). Wilcockson (Reference Wilcockson2020) found that the transition for counsellors was characterised by conflicts of identity and values, with overt resistance to some aspects of CBT theory and practice or the target-based ethos of TTAD. Conversely, the Knowledge, Skills & Attitudes (KSA) group in this study, largely consisting of PWPs, experienced an easier transition by displaying a largely positive attitude towards CBT and the training process, despite feeling less confident in their skills.
Epistemological fit with CBT
In a study of German trainees, Wolff and Auckenthaler (Reference Wolff and Auckenthaler2014) explored the psychological processes that are involved in what they describe as ‘theoretical orientation development’. Twenty trainees were interviewed and data analysis using grounded theory showed that, rather than being a linear process towards becoming a CBT therapist, trainees were seen as ‘constructing jugglers’ who were constantly defining and re-defining their understanding of CBT as training progressed. Their ‘CBT identity’ was in constant flux, influenced by clinical experiences that either blurred or narrowed the boundaries of what they considered to be acceptable in terms of CBT methods. Importantly, two distinct groups of trainees emerged from the data – those who identified as ‘CBT therapists’ and those who identified as ‘psychotherapists’. The former held positive beliefs about CBT prior to training, suggesting a good epistemological ‘fit’ with its theories and methods. Conversely, the latter were more likely to enter training due to being unable get a place on a course of a different modality (e.g. psychodynamic) and to home in on the perceived limitations of the approach.
Competing ‘selves’
In terms of knowledge and skill acquisition, the ideal ‘CBT therapist self’ will contain sufficient declarative knowledge of models and techniques (Bennett-Levy, Reference Bennett-Levy2006), as well as demonstrating competence in a range of procedural skills (e.g. Roth and Pilling, Reference Roth and Pilling2007). The transition from their previous professional role also includes adequate socialisation to the values and norms of CBT culture including concordance with CBT supervision (e.g. preparing specific questions, bringing recording of therapy sessions) and engagement in routine outcome monitoring (administering psychometric questionnaires to track improvement or otherwise). In short, old ways of conceptualising mental health problems and of treating specific disorders are not forgotten but are voluntarily relinquished to make room for the new emerging knowledge and skills and identity as a CBT therapist. In an attempt to understand factors that help and hinder the development of guided discovery (GD) skills during training, Roscoe et al. (Reference Roscoe, Bates and Blackley2022) developed an online questionnaire and analysed the responses of (n=18) CBT trainees. Grounded theory was used to develop a model that hypothesised barriers to GD skill acquisition, most notably the concept of ‘competing selves’ whereby a ‘previous professional self’ (e.g. PWP) competes with the emerging ‘CBT therapist self’ (see Bennett-Levy, Reference Bennett-Levy2006) upon exposure to new learning experiences. In moments of self-doubt, trainees would abandon the use of Socratic dialogue and resort to didactic ‘teaching’ of methods to clients.
Negative attitudes towards CBT, misconceptions and ‘therapist drift’
In addition to the expected adjustment processing of transitioning from one career to another, a range of negative attitudes toward CBT (e.g. ‘It is too hard to implement in real life settings’) have been identified amongst CBT therapists and trainee clinical psychologists (Parker and Waller, Reference Parker and Waller2017; Rodwell et al., Reference Rodwell, Kent and Hale2023). Dislike towards or discomfort with key elements of CBT such as agenda setting, homeworking setting, Socratic dialogue and the weighing of patients have been documented previously (D’Souza et al., Reference D’Souza Walsh, Davies, Pluckwell, Huffinley and Waller2019; Waller and Turner, Reference Waller and Turner2016; Waltman et al., Reference Waltman, Hall, McFarr, Beck and Creed2017). Alternatively, some therapists have misconceptions of CBT models or treatment plans that are never corrected during training or supervision (e.g. Murray et al., Reference Murray, Grey, Warnock-Parkes, Kerr, Wild, Clark and Ehlers2022) whilst others develop very rigid interpretations of CBT (e.g. reliving can only be used with PTSD) and fail to utilise meta-competences in their practice (Butler et al., Reference Butler, Fennell and Hackmann2010; Campbell-Lee et al., Reference Campbell-Lee, Barton and Armstrongin press; Roth and Pilling, Reference Roth and Pilling2007). If these beliefs are not addressed within training or supervision there is the possibility of ongoing ‘therapist drift’ (Waller, Reference Waller2009) where CBT therapists consciously or unconsciously omit key aspects of treatment. For example, Bell et al. (Reference Bell, Mackie and Bennett-Levy2015) found that recently qualified CBT therapists rarely used imagery with clients, and there is growing research that shows a propensity for therapists to avoid exposure-based interventions when working with panic disorder, obsessive compulsive disorder and post-traumatic stress disorder (e.g. Deacon et al., Reference Deacon, Farrell, Kemp, Dixon, Sy, Zhang and McGrath2013; Meyer et al., Reference Meyer, Farrell, Kemp, Blakey and Deacon2014; Meyer et al., Reference Meyer, Kelly and Deacon2020).
In summary, CBT training poses both universal and profession-specific challenges for individuals. The personal and previous professional ‘selves’ of a trainee may act as roadblocks to CBT skill development. Accordingly, it is of increasing importance to further examine the characteristics of those choosing to train in CBT given that issues such as role transition resistance, values conflicts, negative beliefs about CBT and therapist drift are known to affect competence and adherence to evidence-based practice. One area that has received little attention is what motivates individuals to train in a particular theoretical orientation (Arthur, Reference Arthur2000).
Study aims
Whilst existing research by Wilcockson (Reference Wilcockson2020, Reference Wilcockson2022) has identified some of the role transition challenges for different professional groups (e.g. counsellors) during training and post-qualification, there are no studies to our knowledge that examine the primary motivations of individual practitioners’ decisions to train in CBT. The present study is concerned with exploring why individuals choose to engage in CBT training, instead of other therapeutic modalities (e.g. psychodynamic). Given that a proportion of those engaging in CBT training experience negative beliefs about the modality, values conflicts, and resistance to implementing key aspects of treatment, it is of interest to understand what motivates them to do so in the face of these challenges. As little exists within the CBT literature on this topic, the aim was to develop a theory of motivational factors and from this, develop a conceptual model to provide trainers and supervisors with a shared language that can be used within workshops or supervision.
Method
Participants
A total of (n=43) qualified CBT practitioners were recruited from a variety of sources initially from the first author’s professional network (email distribution lists of former trainees, other CBT course tutors). Theoretical sampling led to further recruitment via workshop attendees, and social media platforms. All participants used a weblink to the online surveys platform where they were provided with a study information sheet and consent form. In terms of demographics, 91% were female and participants ranged from being qualified less than a year (34%), up to 10 years and over (18%); 66% were BABCP accredited and whilst the majority were from England (91%) with the Northwest being the highest (77%), there was representation across the Midlands, South West, South East and East of England, Scotland and Wales. In comparison with earlier studies (Robinson et al., Reference Robinson, Kellett, King and Keating2012; Wilcockson, Reference Wilcockson2020), this research aimed to capture the experiences of a broader number and range of professionals (notably occupational therapists and social workers), from different institutions to reduce the possibility of the training or supervision style being responsible for therapist attitudes and experiences. Qualified CBT therapists were targeted based on the rationale that they will have had some time to reflect on the entirety of their training experience in a way that those still undertaking courses would not. Previous professional roles were as follows: PWP or equivalent, e.g. graduate mental health worker (41%), mental health nurse (19%), counsellor (11%), occupational therapist (4%), social worker (4%), assistant psychologist (2%) and ‘other’ (e.g. counselling psychologist) (19%). There were no clinical psychologists or psychiatrists that took part.
Design
A questionnaire was developed that involved participants answering eight open-ended questions (see Table 1). Questions were chosen which focused on three related areas: (1) understanding motivations to train, expectations of training and reasons for continuing to work as a CBT therapist; (2) gauging aspects of CBT that have been mastered and aspects that continue to present challenges (e.g. if there is any resistance to theory, models, or interventions as per the extant literature); and (3) identifying factors that have aided role transition. Questions were selected on the basis that they might reveal the impact that certain motivations have on perceptions of CBT (e.g. that CBT is less emotionally demanding than other modalities) or of learning CBT. In addition, demographic information was collected to aid the identification of any patterns in responses to questions by professional group. Whilst surveys lack the opportunity to probe participants for elaborations on answers, they have several advantages. The first is that as a format, an online questionnaire is less time consuming than an interview or focus group, thus potentially more attractive to participants. The use of social media platforms also enables the researcher to reach beyond their professional contacts, recruiting more geographical diverse participants (Braun et al., Reference Braun, Clarke, Boulton, Davey and McEvoy2021). Secondly, the anonymity from the researcher fosters more openness and honesty, especially for participants who might have trained at the institution where the first author taught and supervised at the time of data collection.
Table 1. Open-ended survey questions

Data analysis
Grounded theory (GT; Glaser and Strauss, Reference Glaser and Strauss1967) was deemed the most appropriate method for model development as Stern (Reference Stern1980) states that ‘the strongest case for the use of grounded theory is in investigations of relatively unchartered waters’ (p. 20). There now exist several schools of thought within GT and the approach to this study was influenced by the work of Charmaz (Reference Charmaz2006). Data analysis began with line-by-line coding of all 43 responses to each question with a series of ‘gerunds’ being developed from this process (Ward et al., Reference Ward, Gott and Hoare2017). The next step was a constant comparison of the provisional sub-categories before discussing these with the second author. As an inductive approach, it is recommended that when using this methodology, researchers should refrain from exploring the extant literature until after the data analysis has been undertaken. This is not always feasible, and, in this study, the lead researcher was an experienced CBT trainer and had undertaken previous research related to CBT training, therefore total blindness to the literature was not possible. It was decided that a more extensive literature search would be delayed until after the memo-writing stage (e.g. the Wolff and Auckenthaler, Reference Wolff and Auckenthaler2014 paper was not read until after the initial coding and categorisation).
Researcher reflexivity
It is important for qualitative researchers to acknowledge how their own experiences and attitudes may influence question selection and subsequent data analysis (Patnaik, Reference Patnaik2013). As a CBT trainer and supervisor, the lead author is primarily concerned with investigating practical problems within supervision and training and generating pragmatic solutions.
Epistemolgically and ontologically, they identify with pragmatism and for pragmatic researchers, solutions are more important than the quest for ultimate truths (Morgan, Reference Morgan2014). The focus on what is helpful gives the pragmatic researcher freedom to explore methods that will provide the most helpful avenues of enquiry. The first author also recognises their ‘insider-outsider’ position as both a researcher, CBT therapist and former CBT trainee (Dwyer and Buckle, Reference Dwyer and Buckle2009). For these reasons, several ‘bracketing’ measures were employed including memo-writing, a research diary, and discussions with the second author (Tufford and Newman, Reference Tufford and Newman2012). Data analysis was largely completed by the first author, with the second author (a psychologist who does not practise CBT) tasked with checking the codes for reliability. Following comparison and discussion, a range of amendments were made to provisional categories and sub-categories. Finally, a more extensive literature review was undertaken by the first author around the topics of role transition, therapist skill development, epistemic style, and negative attitudes towards CBT.
Results
Core category: alignment with CBT
The analysis showed that the various motivations to train in CBT could be subsumed under the core category of ‘alignment with CBT’. This was supported by the identification of two distinct groups of therapists: ‘CBT endorsers’ (n=20) and ‘career enhancers’ (n=21) with (n=2) negative cases identified. Four inter-related categories and eight sub-categories were developed (see Table 2).
Table 2. Overview of categories and sub-categories
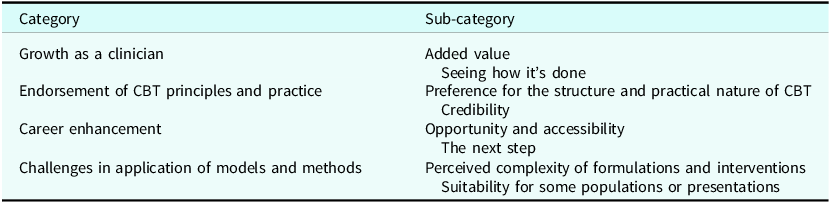
Figure 1 shows a diagrammatic representation of the model that was developed from the core and sub-categories. The model hypothesises that as individuals begin their CBT training, pre-disposing factors such as one’s epistemic style may create a natural alignment for some trainees with the theories and methods underpinning CBT (as was the case for the CBT endorsers). These participants frequently referred to being drawn to the evidence base and the structure or practical nature of CBT. In contrast, the career enhancers were more likely to view CBT as an opportunity to work with different populations, become affiliated with a professional group or switch to a more favourable role. The data indicated the existence of both universal (relevant to all participants) and group-specific motivational factors. The model also hypothesises that alignment towards CBT is a bi-directional process. For example, the types of clinical cases and the perceived quality of workshops and supervision during training can inhibit skill development or exacerbate negative beliefs about CBT (e.g. that it does not work for certain populations), thus potentially reducing motivation. A selection of participant comments are included below to give examples of each category, sub-category and their relationships within the model.

Figure 1. Preliminary grounded theory model of the motivational factors involved in training as a CBT therapist.
1: ‘Growth as a clinician’
This category contains both universal factors that appear to enhance motivation to train in CBT (‘added value’) and experiences that are seen to inhibit skill development, potentially weakening one’s alignment with CBT. Overall, participants from both groups felt that undertaking CBT training would lead to some form of personal growth. For example, many viewed the training as helping them to expand their knowledge and skills as a mental health practitioner or therapist.
1a: Added value
Participants responses centred on internal (self) and external (client-based) rewards. CBT qualification was seen to improve employment prospects for some, whilst for others, CBT qualification added something to their skillset (e.g. feeling more competent than in previous roles) For example, some of those who had worked as mental health nurses viewed CBT as superior, with one participant commenting that they:
‘See more improvement than in nursing’ (P37)
Some rewards were both internal and external, with tangible changes in clinical outcomes (e.g. recovery rates) a significant pull to CBT for occupational therapists:
‘I have seen real change with people reclaiming their lives in ways I did not with OT alone’ (P3, occupational therapist)
Several participants also spoke of factors related to CBT interventions that were of significant benefit to their clients. For example, with some participants who had worked as PWPs prior to training, ‘high-intensity’ CBT led to a more notable cognitive shift for their clients:
‘Feeling like something was missing for some clients’ (P16)
P21, another former PWP, spoke of their CBT client experiencing ‘lightbulb’ moments:
‘Seeing clients grasp a concept and apply it and be proactive to build on their learning. Seeing client distress reducing’ (P21)
For another, practising CBT gave them an opportunity to see the positive effects of non-pharmacological approaches:
‘It works and empowers people often without medication’ (P13)
Counsellors also viewed CBT in a positive light as evidenced by the experience of P26:
‘I was attracted to the structure of the approach and focus on the here and now. I was frustrated by the lack of structure and emphasis on non-directivity in counselling and I wanted to be able to support patients with evidence-based techniques and strategies and play a more active role as therapist than was possible as a counsellor’ (P26, counsellor)
Being able to work with a wider range of disorders and the need to constantly improve their skills were also strong motivations. In particular, new or complex clinical presentations were viewed by some as opportunities to develop as a CBT therapist:
‘It keeps me on my toes. While I become more experienced and confident, there is always a new way that a patient will present and new skills to hone’ (P2, PWP)
Whilst several participants discussed some perceived shortcomings in aspects of CBT formulation or treatment, there was a sense that when it is applied to appropriate clients, there is real job satisfaction:
‘When it goes well it works fantastically and the reward is huge’ (P20, PWP)
1b: Seeing how it’s done
The second sub-category that affected participants’ growth as clinicians was related to their exposure to shadowing of therapy sessions and modelling of formulations or interventions. The opportunities to ‘see how it is done’ were insufficient according to several participants. Limited access to seeing how qualified practitioners (tutors, supervisors or workplace peers) might draw out specific formulations or deliver certain interventions featured heavily and was perceived to delay skill development:
‘Having experienced staff demonstrate and show clinical skills and show their videos of clinical work’ (P22, mental health nurse)
It was noteworthy that several PWPs who were already familiar with the set-up of IAPT services and had likely been supervised by CBT therapists in their previous roles, also commented on the need for:
‘… more time and practical support in terms of having more opportunities to shadow qualified practitioners or watch video recordings of sessions’ (P35, PWP)
Others stressed the importance of university input and wanted to see more extensive demonstrations by tutors before being asked to role-play methods that were being taught in training:
‘More visual sessions of CBT in practice following the theory before role playing it ourselves’ (P23, other)
2: Endorsement of CBT principles and practice
This category relates to group-specific factors and captured two of the main attractions to CBT for ‘the endorsers’.
2a: Preference for the structure and practical nature of CBT
Firstly, these therapists frequently spoke of their preference for the hallmarks of CBT such as its use of structure (e.g. agenda setting and homework) and the practical nature of sessions (teaching the client skills or testing out predictions):
‘The practical nature of CBT was appealing as it enables the person to take some control over making positive changes’ (P18, PWP)
For one therapist, formerly a mental health nurse, there was a sense that CBT complimented previous ways of working:
‘CBT seemed credible and fitted with how I could make sense of a case load of clients when working as a CPN. I also liked the idea of clients having practical skills to use’ (P22, mental health nurse)
2b: Credibility
The second ‘pull’ of CBT was the evidence base which offered credibility, perhaps in contrast to other modalities, but this was not stated directly. For endorsers, CBT was superior to pharmacological approaches:
‘The evidence that CBT is more effective than medications in the treatment of depression, anxiety, and other mental disorders’ (P1, other)
Several participants simply stated ‘evidence based’ as an attraction to CBT, whilst some mentioned the use of scientific methods in developing protocols (e.g. being developed from randomised controlled trials) as being important to them.
3: Career enhancement
This category captures the views and experiences of the ‘career enhancers’ group. The primary motivations cited by these therapists was related to pay, accreditation and progression in their careers.
3a: Opportunity and accessibility
Several participants appeared to have chosen to undertake CBT training primarily because there was the opportunity to do so:
‘The course was funded and was a paid training position’ (P30, PWP)
Another participant commented on how CBT training provided an exit route out of the NHS:
‘It was a way to qualify as a therapist which enabled me to leave the NHS. It was also the only training opportunity offered to me’ (P4, social worker)
P6, an assistant psychologist in their previous role, appeared to hold multiple motivations, with some level of epistemological fit but also a pragmatism in their choice due to perceived employment prospects post-qualification:
‘The evidence base. The clear training structure. The appeal that there will always be jobs in CBT’ (P6, assistant psychologist)
3b: The next step
For those already working in TTAD (or IAPT when they trained), becoming a CBT therapist felt like the next step after gaining skills and experience in the PWP role:
‘It felt like a natural progression from the role of PWP. I was attracted to the opportunity to be creative and curious with clients whilst also focusing on supporting them in making changes. The balance of working with the past whilst working in the present. It also allowed me to work with a range of disorders within IAPT’ (P2, PWP)
For those outside of IAPT, CBT was seen as either complimentary or the intended destination from the beginning epitomised by P5:
‘… only studied nursing to get to CBT’ (P5, mental health nurse)
Others described CBT as building upon existing skills that were acquired in previous professional roles:
‘CBT felt like a positive way to build on my OT skills’ (P12, occupational therapist)
4: Challenges in application of models and methods
The final category reflected the challenges that both groups experienced when applying CBT in routine clinical practice. Locus of control appeared to be of significance here as the endorsers seemed to struggle more with their understanding (internal locus of control) of formulations or techniques and perceived this to be a barrier to their effectiveness as CBT therapists. This is captured in the sub-category ‘perceived complexity of formulations and interventions’.
4a: Perceived complexity of formulations and interventions
There were numerous examples of ‘CBT endorsers’ experiencing challenges with:
‘Understanding and explaining formulations’ (P32, PWP)
Participants seemed to struggle with knowing how much information was ‘enough’ to collate or present to a client in a formulation. This was highlighted in relation to longitudinal data:
‘Formulations feel complex to me still. Getting enough historical information but not to the point of overload’ (P31, occupational therapist)
Length of time qualified did not necessarily lead to more confidence in formulating. Whilst P32 and P31 were qualified less than a year, P9 who had been qualified for over 10 years commented that:
‘I wish I was better at formulating. I do it all the time, but fairly simply’
P9 did not elaborate on their response to reveal which aspects of formulation they struggled with or what a ‘fairly simple’ formulation would consist of. Participants also mentioned difficulties with specific disorders and associated interventions:
‘Find PTSD reliving anxiety provoking and have delayed doing this in the past. Self esteem another area have not had any training in but need to treat at times’ (P33, PWP)
Finally, P38 suggested that the length of training was too short and that extending all high-intensity training courses to two years might help trainees to develop more proficiency in models that they are expected to learn:
‘I think my only difficulty with CBT training is 1 year isn’t sufficient. I think the training should be 18 months to 2 years to really be proficient in cognitive and behavioural models’ (P38, PWP)
4b: Suitability for some populations or presentations
In contrast to the self-doubt experienced by the endorsers, the enhancers appeared to locate the problem within the models, methods, or clients themselves; for example, viewing CBT as being unfit for the diverse populations that they were working with. Several enhancers voiced what they perceived to be the shortcomings of CBT and scepticism about how well it works with specific client populations or in certain contexts:
‘It is difficult to adapt some protocols and make it inclusive for some groups of people like neurodiverse clients’ (P35, PWP)
P35 did not elaborate on which protocols were difficult to adapt or what adaptions they would want to be made (e.g. longer sessions). For another participant, they felt that trying to deliver CBT within an IAPT context was a challenge to the development of a strong enough therapeutic alliance:
‘Lack of opportunity at times for relationship building when used in IAPT format. Much prefer private practice where time can be taken’ (P7, other)
There was also a sense that disorder-specific models were a poor match for the clients that therapists were being asked to treat and the impact on recovery rates was of concern to some:
‘The models not being enough to help with certain presentations but still being expected to get them into recovery’ (P3, PWP)
P3 did not expand upon which models they felt were insufficient and which clinical presentations led to them feeling this way. Another former PWP (P16) spoke of a demotivating effect on having a lower recovery rate in their role as a CBT therapist:
‘As a PWP, I had a good recovery rate – not so now. I can find and take little wins, however I feel that I am not [doing] enough, which can become demotivating’ (P16)
A target-based environment also featured in P20’s response as they spoke of feeling the pressure from patients themselves to ‘cure’ them despite having to work with co-morbidity:
‘Expectations from patients to be cured through high intensity therapy. Multiple presentations not fitting directly in to one protocol’ (P20)
Finally, P1 offered a more balanced summary of CBT and how it is applied and with whom:
‘Rather than CBT itself, it has been delivering certain CBT techniques in some group of patients that I have, on occasion, found challenging’ (P1, other)
Discussion
There is an increasing body of research, focused on therapist characteristics and their relationship with fidelity to CBT, clinical competence and treatment outcomes (e.g. Fletcher and Delgadillo Reference Fletcher and Delgadillo2022; Nissen-Lie et al., Reference Nissen-Lie, Rønnestad, Høglend, Havik, Solbakken, Stiles and Monsen2017; Roscoe and Taylor, Reference Roscoe and Taylor2023; Speers et al., Reference Speers, Bhullar, Cosh and Wootton2022; Waller and Turner, Reference Waller and Turner2016). Previous studies have identified factors such as clinician intolerance of uncertainty, self-esteem, negative beliefs about CBT, collusion, perfectionism, therapist schemas and personality traits that may warrant dedicated attention within training courses and supervision (Delgadillo et al., Reference Delgadillo, Branson, Kellett, Myles-Hooton, Hardy and Shafran2020; Haarhoff, Reference Haarhoff2006; Parker and Waller, Reference Parker and Waller2017; Presley et al., Reference Presley, Jones and Newton2017; Simpson-Southward et al., Reference Simpson-Southward, Waller and Hardy2018). The present study is the first to explore the motivations to train as a CBT therapist and how this might impact on how one practises CBT. Whilst we have some understanding of the challenges involved in transitioning from previous roles during CBT training (Robinson et al., Reference Robinson, Kellett, King and Keating2012; Roscoe et al., Reference Roscoe, Bates and Blackley2022; Wilcockson, Reference Wilcockson2020), little was known as to why individuals choose CBT as a career pathway over other therapeutic modalities.
The aim of this study was to develop a theory and related model that was grounded in the data. Following data analysis, two distinct groups of therapists were identified. The first held a primary motivation that appeared to relate to a strong endorsement of the core principles of CBT, with these individuals being referred to as ‘CBT endorsers’. The second type of primary motivation was to advance or enhance one’s career and these individuals became known as ‘career enhancers’. This dual profile of CBT trainees fits with the Wolff and Auckenthaler (Reference Wolff and Auckenthaler2014) study, where participants were identified as being either CBT therapists or ‘psychotherapists’ based on their pre-existing attitudes towards CBT. In the present study, the endorsers were characterised by their preference for structure and trust of the evidence base, indicating a strong epistemological alignment with CBT (Lee et al., Reference Lee, Neimeyer and Rice2013). Participants in this group tended to view CBT as a superior treatment to what they had applied in previous clinical roles (e.g. as mental health nurses or occupational therapists). This echoes the findings of Wilcockson (Reference Wilcockson2017, Reference Wilcockson2020) who found that mental health nurses aspire towards CBT. Professional background was less important in the findings within the present study in terms of which group participants were grouped under. PWPs for example, whose prior training and subsequent work culture (e.g. use of diagnostic classification and psychometric outcome monitoring) might suggest a more natural alignment with CBT theories and interventions, were almost evenly spread between the endorsers and enhancers. Similarly, accreditation, age, and length of time qualified were not significant factors across the two groups. Research by Arthur (Reference Arthur2000) found that different ‘epistemic styles’ are associated with therapists from cognitive behavioural and psychodynamic orientations, and this may help to explain endorsement or otherwise. For example, in the current study, several of the career enhancers’ responses were indicative of a more ‘constructivist’ worldview, whereas CBT endorsers’ comments were suggestive of a rationalist epistemic style (Lee et al., Reference Lee, Neimeyer and Rice2013). These contrasting epistemic styles might have implications for the acceptability of CBT theories and interventions for some trainees. For example, the generic cognitive model that underpins most contemporary CBT protocols postulates that distorted thinking is the main causal factor in emotional distress and behavioural disturbance (Moorey, Reference Moorey2023). Therapists who have a strong constructivist leaning might resist this notion, believing that social circumstances are more important factors, therefore feeling hopeless about the benefits of CBT to certain client groups (Moloney and Kelly, Reference Moloney and Kelly2004).
The endorsers and enhancers also differed in the challenges they faced learning CBT and applying it in clinical practice. Enhancers were more likely to hold negative beliefs about CBT, with several participants stating that it is ill-suited to more complex clinical presentations or for working with neurodivergence. Parker and Waller (Reference Parker and Waller2017) developed the Negative Attitudes to CBT Scale (NACS), which contains items related to the belief that CBT does not work well for minority groups or co-morbid cases. Those who identified as psychodynamic clinicians scored higher on the NACS than CBT therapists; however, other therapist characteristics were found to be of significance such as clinician anxiety and self-esteem.
Irrespective of grouping, most therapists experienced similar struggles during training (e.g. both ‘endorsers’ and ‘enhancers’ mentioned a paucity of opportunities to witness CBT being delivered or modelled by tutors, supervisors, or qualified peers). It has long been recognised that different training methods are necessary for developing the declarative, procedural, or reflective systems (Bennett-Levy, Reference Bennett-Levy2006). For example, in a study of 120 participants, Bennett-Levy et al. (Reference Bennett-Levy, McManus, Westling and Fennell2009) found that modelling and role-play were rated as being the most helpful in developing procedural skills. Participants in the current study perceived a lack of shadowing opportunities and an insufficient amount of modelling to delay skill development. Insufficient opportunities to ‘see how it is done’ may account for both the negative beliefs held by the enhancers (or exacerbation of them) and the self-doubt experienced by the endorsers. Being able to witness an experienced therapist translate a diagram in a book or paper to a real-life client is likely to increase confidence in the real-world application of models (Gyani et al., Reference Gyani, Shafran, Rose and Lee2015). Similarly, observing CBT being adapted to specific populations challenges notions about it being it being rigid or culturally insensitive (Beck, Reference Beck2016).
The reasons why enhancers held more negative attitudes towards CBT remain unclear, although they appeared to mostly relate to CBT as it is applied within TTAD. Several participants referred to the context in which CBT training took place (e.g. P3, P7 and P16), where restricted session numbers and expectations for recovery rates were perceived to have had a negative impact on their experience of learning to apply CBT. This partly fits with the findings of Wilcockson (Reference Wilcockson2017) in that what was then known as IAPT, CBT delivered within that context was considered mechanistic, superficial, and placing little value on therapeutic alliance. Scepticism about the real-world applications of the disorder-specific protocols has also been found in the wider literature. For example, in a study which looked at what IAPT trainees do post-qualification, Liness et al. (Reference Liness, Lea, Nestler, Parker and Clark2017) found that 34% of their survey respondents did not use protocols such as those indicated in NICE guidance or recommendations in the Roth and Pilling competency framework.
Resistance to aspects of CBT may affect the trajectory of the emerging CBT ‘therapist self’ and this process could be explained by the concepts of assimilation and accommodation (Piaget, Reference Piaget and Gabain1948). In short, individuals enter CBT training with existing schemas of what CBT is. These schemas are likely to be influenced by direct or indirect experiences of CBT (experiencing it as a client, observing colleagues, reading books, opinions of trusted others) and act as filters for what the trainee pays attention to. Assimilation involves fitting new information to existing knowledge (e.g. if one starts off with the belief that CBT is invalidating), methods that are demonstrated in lectures or supervision are compared against what is already held to be true. Accommodation on the other hand, involves the development of new schema where the information is accepted by the trainee (e.g. one can be focused with clients through agenda setting yet still compassionate and validating). For participants in the present study, a combination of case complexity and limited opportunities for observation during a crucial time in skill development may reinforce old schemas and delay or impede new schema development, necessary for developing confidence and competence in CBT.
Practice implications
The findings in this study, together with the existing literature, suggest that it might be important for CBT trainers and supervisors to explicitly target ‘personal self’ factors (e.g. motivations, pre-conceptions about CBT, role transition challenges, epistemological positioning) in addition to developing the ‘therapist self’ (Arthur, Reference Arthur2000; Bennett-Levy, Reference Bennett-Levy2006; Roscoe and Taylor, Reference Roscoe and Taylor2023; Wilcockson, Reference Wilcockson2020; Wilcockson, Reference Wilcockson2022). Recommendations for ways to incorporate these into curriculum content or supervision sessions are provided below.
Epistemic style
In light of the findings in the current study and extant literature, it could be useful for course tutors to explicitly discuss the degree to which CBT trainees ‘buy into’ the theories and interventions they are being taught and the efficacy of CBT (Carlsson et al., Reference Carlsson, Norberg, Sandell and Schubert2011; Wolff and Auckenthaler, Reference Wolff and Auckenthaler2014). Epistemic style might influence the degree to which one holds positive or negative beliefs about CBT. Failure to address one’s core view of the world could have implications for the use of specific models or interventions, pre-disposing some trainees to the risk of therapist drift (Waller, Reference Waller2009). Overt discussions during training that explore therapist epistemic style may help to make sense of inert resistance to key aspects of CBT that can be then explored further in supervision. Readers are directed to the recent paper by Moorey (Reference Moorey2023) that addresses this topic.
Using measures of epistemic style and therapist attitudes to CBT
Measures have been developed that postulate a range of therapist attitudes associated with alignment to CBT methods and principles (e.g. Deacon et al., Reference Deacon, Farrell, Kemp, Dixon, Sy, Zhang and McGrath2013; Meyer et al., Reference Meyer, Farrell, Kemp, Blakey and Deacon2014). For example, the Therapist Attitudes Questionnaire has been used to identify epistemic style (DiGiuseppe and Linscott Reference DiGiuseppe and Linscott1993). Other measures can highlight specific difficulties during training such as the Therapist Beliefs about Exposure Scale (Deacon et al., Reference Deacon, Farrell, Kemp, Dixon, Sy, Zhang and McGrath2013) and the Negative Attitudes towards CBT Scale (Parker and Waller, Reference Parker and Waller2017) that may lead to therapy-interfering behaviours if left unaddressed (Waller, Reference Waller2009). Whilst the intention is not to use these as an exclusion criterion for training access, these measures could be administered during supervision or within lectures early in training to normalise and create opportunities to explore the significance of certain beliefs on therapists’ practice of CBT (Lee et al., Reference Lee, Neimeyer and Rice2013). The degree to which these measures have made it into CBT training programmes or supervisory practice is unknown, but our experience discussing these in workshops suggests they are rarely utilised (Roscoe, Reference Roscoe2023b).
Increasing access to training methods that deepen one’s understanding of CBT
The updated high-intensity course curriculum includes more time dedicated to skills practice and has mandated the inclusion of co-therapy, where trainees deliver treatment sessions alongside a qualified peer. The logistics of this have not been set out and services will need time to implement this effectively. Anecdotal experience suggests that access to shadowing is inconsistent, and it would be important for supervisors and qualified therapists to reflect on their own willingness to increase access to live or recorded sessions for trainees. Another promising avenue of skill development is through self-practice and self-reflection (SP/SR), which many courses are beginning to embed within their curricula (Freeston et al., Reference Freeston, Thwaites and Bennett-Levy2019). SP/SR allows CBT therapists to develop ‘meta-competences’ by learning the models and interventions ‘from the inside out’, thus creating opportunities to appreciate the nuances of adapting them to the individual (Bennett-Levy et al., Reference Bennett-Levy, Thwaites, Haarhoff and Perry2014; Thwaites et al., Reference Thwaites, Bennett-Levy, Davis, Chaddock, Whittington and Grey2014).
Tailoring supervision to the needs of the individual
Supervision would seem to be the most logical medium for exploring the issues identified in this study (see Rakovshik and McManus, Reference Rakovshik and McManus2013); however, there was no mention of specific strategies employed by supervisors (e.g. administering a therapist attitudes questionnaire) to assist participants with role transition. The degree to which CBT supervisors explore role transition, negative beliefs about CBT, epistemic style or values conflicts is unknown although the supervision and wider psychotherapy training literature suggests it is uncommon (Carlsson et al., Reference Carlsson, Norberg, Sandell and Schubert2011; Roscoe and Taylor, Reference Roscoe and Taylor2023). For example, whilst the Robinson et al. (Reference Robinson, Kellett, King and Keating2012) study found that trainees valued supervision as a means of managing role transition, it does not appear that the supervisors were specifically asking trainees about role transition challenges and how they might adapt supervision for trainees by their professional group. Providing trainees with a reflective space to work through their intrapsychic challenges (e.g. examining competing beliefs about CBT) could assist in both normalising and working through matters of theoretical orientation. Figure 2 (The Three A’s) provides a brief yet focused discussion tool that supervisors or course tutors can use for troubleshooting aspects of training that are interfering with learning at regular points through the course. This includes a non-exhaustive list of questions that prompt discussion on aspects of training and orientation experiences that were evident in the data. Finally, supervision of supervision might assist with supervisor skill development in these areas and readers are directed to Roscoe (Reference Roscoe2023a) for further suggestions on how to address role transition within CBT training and supervision, and Pugh and Margetts (Reference Pugh and Margetts2020) for examples of how to make CBT supervision generally more active and experiential.

Figure 2. The Three A’s supervision prompt tool.
Limitations
As with all qualitative studies with relatively small sample sizes, there are several limitations to note. Firstly, the generalisability of these findings should be treated with caution. Whilst participants were drawn from a broad range of professional backgrounds, the overall number cannot be seen as representative of the population that practise CBT. For example, clinical psychologists were not represented in this study. It is possible that this group of psychological professionals did not view this survey as relevant to their experience learning CBT as, unlike other groups they are not relinquishing their professional identity when they undertake CBT training. For example, although CBT is now a mandated component of their core training and available as a distinct pathway during doctoral studies, they do not cease to be or work as clinical psychologists when they train in CBT in the way that a social worker does. Nevertheless, it would be useful for future research to explore the processes of CBT skill development and epistemic alignment of this professional group.
Secondly, the gender of participants (91% female) may have had an impact on the findings. Whilst anecdotal evidence from teaching on CBT training courses and research samples (e.g. Liness et al., Reference Liness, Lea, Nestler, Parker and Clark2017) points to a greater number of females in the CBT workforce, a higher number of male participants could have generated different categories. Thirdly, ethnicity was not explored, nor the role of cultural attitudes to CBT or the significance of the cultural background of participants (Beck, Reference Beck2016). A recent study by Vekaria et al. (Reference Vekaria, Thomas, Phiri and Ononaiye2023) found supervisees from racially or ethnically minoritised backgrounds perceived white supervisors to lack cultural competence, thus weakening the supervisory relationship. Feeling invalidated and unsafe supervision might prevent supervisees, especially those in training, from discussing role transition difficulties or values conflicts (Ladany et al., Reference Ladany, Hill, Corbett and Nutt1996).
Fourthly, it is important to stipulate that the motivations held by participants might not be fixed (e.g. could change based on work context) and may not be mutually exclusive (e.g. the enhancers might also endorse CBT, and vice versa). Negative case analysis (see Kolbe, Reference Kolbe1984) found one exception where a participant gave both endorsement and career enhancement related statements as dual motivations; however, most of the responses to the questions in this survey indicated a single primary motivator.
Finally, a limitation of online surveys is that participants cannot be probed to elaborate on their responses (e.g. their understanding of specific questions or how their alignment with CBT has changed over time). Furthermore, it is often said that individuals who have unresolved difficulties in their own lives are drawn to working in counselling or psychotherapy (e.g. the concept of the ‘wounded healer’). Responses to Question 1 did not reveal any ‘unconscious’ motivations to train as a therapist (see Barnett, Reference Barnett2007); however, these might have been revealed through semi-structured interviews or focus groups (e.g. Wilcockson, Reference Wilcockson2022).
Conclusion
CBT has become a popular career choice for many health professionals, yet little was known about why individuals choose to train in CBT, or the implications of their decision. This study had three key aims: (1) to identify common motivations to train and if there were any noticeable patterns in responses; (2) to consider if there was a relationship between specific motivations and the experience of learning and practising CBT; and (3) to develop a tentative model to assist trainers and supervisors in being able to discuss challenges related to motivational factors. As with the Wolff and Auckenthaler (Reference Wolff and Auckenthaler2014) study, two distinct groups of therapists were identified and are referred to as ‘CBT endorsers’ and ‘career enhancers’. The model, derived from participant data, seeks to highlight both universal and group-specific challenges to CBT skill acquisition. Whilst the endorsers appeared to be drawn to the structure and evidence base of CBT, ‘career enhancers’ held more negative beliefs about CBT, particularly its suitability for working with complexity or neurodiversity. The data did not generate a direct hypothesis for these differences; however, the wider literature indicates that the epistemic style of individuals may underpin a natural alignment with CBT.
Further research is required before these groups can be considered representative of CBT therapists. Future research might consist of semi-structured interviews to allow for a more detailed exploration of the lived experience of CBT therapists to gain a deeper understanding of motivations and how these impact on clinical practice (Smith et al., Reference Smith, Flowers and Larkin2009). At present, there is no evidence to suggest that endorsing CBT structure or style is related to therapist adherence or competence. Research might also look to examine if there is a relationship between epistemic style and clinical outcomes within CBT training or in patient recovery rates. Recommendations have been made as to how CBT tutors and supervisors might incorporate the study findings into lectures, curriculum design or supervision.
Key practice points
-
(1) Specific motivational factors may be associated with the delivery of and engagement in core CBT formulation and interventions.
-
(2) Epistemic style appears to be related to the difficulties that are experienced by therapists when applying CBT.
-
(3) Discussing motivations openly in training and supervision might help therapists to explore the impact of their epistemic style.
Data availability statement
The data that support the findings of this study are available upon reasonable request.
Acknowledgements
The lead author is grateful to Frances Roscoe for helpful comments on earlier drafts of this paper.
Author contributions
Jason Roscoe: Conceptualization (lead), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (lead), Writing – original draft (lead), Writing – review & editing (lead); Susan Wilbraham: Data curation (supporting), Formal analysis (supporting), Supervision (supporting).
Financial support
The authors received no funding for this piece of research.
Competing interests
The authors have no competing interests with respect to this paper.
Ethical standards
The authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. Ethical approval was granted by University of Cumbria, reference number 21/38. Participants provided consent to take part in this research and for the results to be published.









Comments
No Comments have been published for this article.