- NDNS
-
National Diet and Nutrition Survey
- YPFA
-
Young Person's Food Atlas
Challenges in dietary assessment
The challenges of assessing dietary intake in any population are well recognised and well documented. Common problems encountered include under-reporting( Reference Goris, Meijer and Westerterp 1 ), subject selection bias and recording bias( Reference Livingstone, Prentice and Strain 2 ). Traditional ‘Gold Standard’ dietary assessment methods, such as weighed food intakes, can be costly and impractical with high levels of participant burden resulting in poor response and low completion rates. Subconscious and/or intentional changes to diet in order to facilitate recording are also commonly reported( Reference Berg, Jonsson and Conner 3 ).
Measuring dietary intake of children brings numerous additional challenges( Reference Livingstone and Robson 4 ). Young children are unlikely to have the cognitive skills to be able to recall their food intake, may not have basic writing skills and are likely to have very limited knowledge of food names, food types and details of food preparation. With skilled interviewing young children may be able to give a description of the food based on colour, taste and texture and may be able to answer questions such as ‘was the food made in a pan on top of the cooker or inside the oven?’, but to achieve any degree of accuracy reports need to rely on a parent or carer.
Assessment is further complicated by the number of people likely to be involved in caring for the child. Parents’ knowledge of foods consumed out of the home may be limited and nursery/school staff are unlikely to be able to provide accurate reports on the many children in their care.
Perhaps the most challenging issue in this age group, however, is estimating or measuring the amount of food leftover. This is particularly true for the preschool age group where food leftovers are likely to be on the floor or soaked into clothes making it challenging for even the most diligent parent to provide an accurate estimate of the amount leftover, and so consumed. Including an estimate of the amount leftover by young children is, nevertheless, very important as they may leave a substantial proportion of the food served to them. Analysis of the National Diet and Nutrition Survey (NDNS) data shows children under age 4 years left approximately 10 % of all foods served to them and that this varied by food type from 39 % of baked potatoes to 0 % of shop bought milkshake( Reference Gregory and Lowe 5 ).
It has been reported that from age 8 years onwards there is a rapid increase in children's ability to provide accurate reports of their dietary intake( Reference Livingstone and Robson 4 ) and research suggests that children may be able to respond to a 24-h dietary recall by the age of about 10 years( Reference Baranowski and Domel 6 , Reference Domel 7 ). Children aged 10 years and over are more likely to have the cognitive skills and writing skills to report their own food intake. They may have some of the food knowledge required, although they still may not be able to provide detailed information on food type and preparation methods. This is arguably also true of many adults. The key challenge with adolescents is likely to be engaging participants in the process and engendering interest and motivation. It may be more difficult for adolescents to report their food intake due to the increased amount of time spent away from home where foods consumed may be forgotten. In addition, adolescents may not wish their parents to know what they have been eating and some may have a preoccupation with weight( Reference Bandini, Cyr and Must 8 ).
The method used will vary depending on the amount of detail required on the diet and time period of interest. The present paper gives a summary of some of the dietary methods available for assessing food intake in children; this summary is followed by more in-depth accounts of two such tools developed at Newcastle University.
Summary of dietary assessment methods for young children (age 10 years and under)
A number of dietary assessment methods have been used in assessing the dietary intakes of children aged 10 years or younger. These methods rely on a parental report of the child's intake and may include reports from additional carers such as nursery staff or observation by researchers.
Magarey et al. ( Reference Magarey, Golley and Spurrier 9 ) developed the 28-item Children's Dietary Questionnaire. Designed to be quick and easy to complete, it assesses intake patterns in either the previous week or 24 h of selected foods chosen to be markers of a healthy diet. The tool demonstrated acceptable reliability and relative validity for assessing group level dietary patterns but is not suitable for assessing intake at the individual level.
The Food Assessment in Schools Tool is a simple tool designed to be used by non-specialists to assess the dietary intake of large groups of children aged 3–7 years. The diary incorporates elements of the food diary and food frequency methods( Reference Adamson, Griffiths and Carlin 10 ). It was designed for assessment of large groups of children in a school setting but not to place any burden on the school. Trained lay observers (e.g. parent helpers) record consumption during school time and parents or carers record consumption at other times. There is no estimation of individual portion size; rather all foods are linked to age- and gender-specific average portions derived from the NDNS( Reference Gregory and Lowe 5 ). The relative validity of 4 d Food Assessment in Schools Tool was assessed by comparison with 4-d weighed intakes. Food Assessment in Schools Tool was found to underestimate total daily intake of fruit and vegetables slightly (−0·2 portions) with limits of agreement from an underestimate of 38 % to an overestimate of 24 %.
The Child and Diet Evaluation Tool is also a combined food diary and a food frequency tool designed for use with children aged 3–7 years. It is completed prospectively by the parent along with school staff and other carers. Again each item on the tick list is linked to age- and gender-specific portion sizes. Comparison against a 1-d semi-quantitative food diary found good correlation for both foods (range = 0·44–0·89) and nutrients (range = 0·41–0·68) and a low level of misclassification. There was a tendency to overestimate the intake of fruit and vegetables (+45 g, equivalent to about 0·5 portions) with limits of agreement from an underestimate of 157 % to an overestimate of 200 %. Parent and teacher evaluation of the tick list was very positive( Reference Cade, Frear and Greenwood 11 ).
The multiple pass 24-h dietary recall method has been used with parents of preschool children aged 0–47 months( Reference Butte, Fox and Briefel 12 ). In a study to assess the feasibility of two 24-h dietary recalls with parents of preschool children, Trolle et al.( Reference Trolle, Amiano and Ege 13 ) concluded that the 24-h recall was best combined with a food record book for recording foods consumed out of the home, at nursery or friends’ houses and that information from other carers was required for most interviews with portion size estimated by picture books or household measures.
In a pilot for the recent Diet and Nutrition Survey of Infants and Young Children the use of graduated containers, cups and measuring spoons was investigated as an alternative to weighed intakes for preschool children. Parents were asked to keep a 4-d diary using the containers and a 4-d weighed food diary for comparison. The mean intakes for weighed and estimated methods were found to be very similar. Perhaps surprisingly the majority of parents in this small sample (n 50) said they preferred the weighed method as they felt it was more accurate; however, this was a sample of volunteers who agreed to keep a 4-d weighed diary and therefore are unlikely to be a representative sample of the population( Reference Delve, West-Sadler and Foster 14 ). For the estimated method, the pots and spoons were deemed useful, especially for measuring soft foods but they were less useful for finger foods such as cubes of cheese and pieces of toast. The main Diet and Nutrition Survey of Infants and Young Children survey which followed this pilot employs a 4-d food diary kept by the parent or guardian with portion size estimated using household measures and food photographs( Reference Lennox, Sommerville and Ong 15 ).
In the Irish National Pre-School Nutrition Survey( Reference Walton 16 ) parents were asked to keep a 4-d food diary with portion sizes weighed or estimated using the Young Person's Food Atlas (YPFA, described in detail later)( Reference Foster, Hawkins and Adamson 17 ). Four-day food diaries were also used in a study to assess potential exposure to migrants from food packaging, where detailed information on the foods consumed and their packaging were required at the individual level( Reference Foster, Mathers and Adamson 18 ). Foster et al. ( Reference Foster, Hawkins and Adamson 17 ) asked parents of children aged 6 months–6 years to complete a 4-d food diary with portion-size estimation using food photographs( Reference Nelson, Atkinson and Meyer 19 ) and conducted observation in nursery or school.
In their paper ‘Recommendations for a trans-European dietary assessment method in children between 4 and 14 years’, Andersen et al. ( Reference Andersen, Lioret and Brants 20 ) recommend a structured food record with photographs and household measures for 4–6 year olds, and for children aged 7 years and above repeated 24-h recalls with the parent and child supported by a food record booklet for recording the details of foods consumed outside the home. For both methods, they recommend portion sizes estimated by a combination of photographs and household measures( Reference Andersen, Lioret and Brants 20 ).
Summary of dietary assessment methods for self-completion by older children (age 11 years and over)
Authors quote a range of ages after which children are capable of accurately reporting dietary information. This is to be expected since the minimum age for self-completion of a dietary assessment method by children will depend on the method itself. A young child able to respond to a 24-h recall for example may struggle with a more demanding method such as the FFQ, which requires the cognitive skills to average consumption over time( Reference Baxter 21 ). It is inevitable that the levels of accuracy which can be expected will be lower with children of younger age. It is necessary to accept the limitations that age and associated conceptual ability may impose on studies with young children. The consensus indicates that by age 8–10 years children may provide a more accurate account of their intake than their parents or other adults( Reference Livingstone and Robson 22 – Reference Domel 24 ).
The US Department of Agriculture National Health and Nutrition Examination Survey collects nutritional data using 24-h recalls with portion size estimated using household measures and a food models book, and children aged 12 years and over respond for themselves( 25 ). There may be a tendency for children to overestimate energy intake by the 24-h recall method( Reference Burrows, Martin and Collins 26 ). The UK NDNS uses a 4-d food diary with weights estimated using household measures and food photographs, and children aged 12 years and over keep a diary of their own intake. Both estimated and weighed food diaries with children aged 12–18 years may be associated with underestimation of energy intake( Reference Burrows, Martin and Collins 26 – Reference Bratteby, Sandhagen and Fan 28 ). Photographic food records kept on a mobile phone have been used successfully in children aged 11–15 years( Reference Boushey, Kerr and Wright 29 ).
A preference for methods which utilise technology over pen and paper methods has been found( Reference Boushey, Kerr and Wright 29 , Reference Boushey, Kerr and Wright 30 ). With this in mind a number of groups have developed computer-based 24-h recalls, a summary of which is given in Table 1.
Table 1. Summary of computer-based dietary assessment methods for children
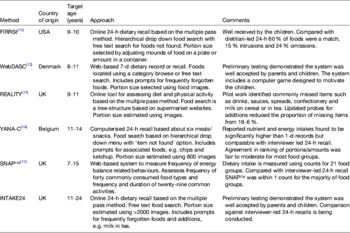
Baranowski et al. ( Reference Baranowski, Islam and Baranowski 31 ) developed Food Intake Recording Software System (FIRRSt) which is a computerised 24-h recall for use with children aged 9–10 years. The system is based on a multiple pass 24-h recall and has child-friendly animated characters to guide the child through tasks. When compared against a dietitian-led 24-h recall 60 % of the foods reported using FIRRSt were a match, 15 % were intrusions (i.e. reported in FIRRSt but not in the dietitian-led recall) and 24 % of foods were omitted (i.e. reported in the dietitian-led recall but not in FIRRSt( Reference Baranowski, Islam and Baranowski 31 ).
In Europe, Vereecken et al. ( Reference Vereecken, Covents and Matthys 34 ) have developed a computerised 24-h recall for use with adolescents aged 11–14 years (young adolescents’ nutrition assessment on computer (YANA-C)). The system is structured about six eating occasions, including both meals and snacks, and takes the volunteers through the previous day's activities. The relative validity of YANA-C was compared against 1-d food records and interviewer- led 24-h recalls. Nutrient and energy intakes were found to be significantly higher in YANA-C in comparison with the food record, but not in comparison with the interview. Agreement in ranking portions/amounts was found to be fair to moderate for most food groups( Reference Vereecken, Covents and Matthys 34 ).
WebDASC is a web-based, 7-d record or recall method for children aged 8–11 years developed in Denmark( Reference Biltoft-Jensen, Trolle and Christensen 32 ). The system includes a computer game with high score list designed to motivate the children to complete their recall. The Rowett Energy intake And Lifestyle Internet Tool for You (REALITY) is designed for completion by children aged 9–11 years. It is an internet-based tool for assessing both diet and physical activity and is based on the multiple pass 24-h recall( Reference Jackson 33 ). The system is designed to gather information on foods and portion sizes to assess energy and nutrient intakes and also type and duration of physical activity.
The Synchronised Nutrition and Activity Programme (SNAP™) is a system for use with children aged 7–15 years old. This web-based method is not designed to measure nutrient intakes but rather the ‘frequency of energy balance-related behaviours’ at the group level. The system assesses frequency of consumption of forty commonly consumed food types and the frequency and duration of twenty-nine common activities (including sedentary activities such as watching television or reading a book)( Reference Moore, Ells and McLure 35 ).
Portion-size estimation with/for children
One of the key challenges in dietary assessment is reducing the burden on the participant to improve recruitment and completion rates while maintaining a reasonable degree of accuracy of the data collected. One method of reducing the burden to the participant is to use portion-size assessment tools to obtain an estimate of the amount of food consumed. Food photographs have been developed and validated for use with adults( Reference Nelson, Atkinson and Meyer 19 ). However, research has shown that adult food photographs are not suitable to use with children( Reference Foster, Matthews and Nelson 36 , Reference Frobisher and Maxwell 37 ).
Between ages 4 and 7 years children become more accomplished at classifying objects by size, shape and colour( Reference Shaffer 38 ). A number of the skills required to estimate portion size are not fully developed until age 10–11 years. These include size constancy (the realisation that although an object appears smaller if further away it is actually the same size), conservation (the ability to recognise that size remains the same when the appearance of the object changes( Reference Goswami 39 ), e.g. tall thin container v. short broad container) and reversibility (the ability to undo an action by mentally doing the reverse, e.g. mentally unpouring a liquid from one container and being able to imagine it in the original container.)
Development and validation of the Young Person's Food Atlas
The YPFA is a book of photographs for use in assessing the portion size of foods consumed by children aged 18 months–16 years developed by the Human Nutrition Research Centre at Newcastle University, UK. To maximise utility, three separate versions of the atlas for use with children of preschool age (18 months–4 years), primary school age (4–11 years) and secondary school age (11–16 years) were developed. The foods selected and portion sizes depicted in the tool are based on the foods and portion sizes recorded by children taking part in the NDNS carried out in Great Britain( Reference Gregory and Lowe 5 , Reference Gregory, Collins and Davies 40 ). The top 100 foods in each age group were included based on the frequency of consumption, weight of consumption and contribution to energy intake. This resulted in the tools being suitable for use in the estimation of portion size for about 85 % of the weight of food consumed by children in the recent NDNS study( Reference Gregory and Lowe 5 ). The YPFA includes 2055 high-quality images of 104 different foods.
It was originally intended that the range from the 5th to the 95th centile of weights consumed would be presented following the format of the Adult Food Atlas( Reference Nelson, Atkinson and Meyer 19 ). However, the 5th centile for weight consumed was very small for a number of foods. Children rarely consume all the food served to them and therefore may never have seen the amount of food they consumed. Working with visual perception psychologists, the decision was taken to produce images for the estimation of the amount of food served and the amount leftover. A further change was to present seven weights from the 5th to the 95th centile of weight served which were calculated as equal increments on a log scale. The portion sizes are presented on a log scale as sensory systems respond in a logarithmic fashion to objects in the external world( Reference MacMillan, Creelman and Wiley 41 ). If the increments between a range of photographs are of equal gram weight (e.g. 10 g increments) it is more difficult to detect the difference between the two largest portion photos, e.g. 60 and 70 g (a difference of +17 %) than between the smallest two, e.g. 10 and 20 g (a difference of +100 %).
The photographs are in two main formats: (1) for foods which do not come in predetermined amounts, for example broccoli (Fig. 1), seven portions for estimation of amount served and seven portions for estimation of amount leftover are presented; (2) for foods which come in predetermined amounts, such as bread rolls, biscuits and cakes, guide photographs are used which show a range of the common portion sizes available (Fig. 2).
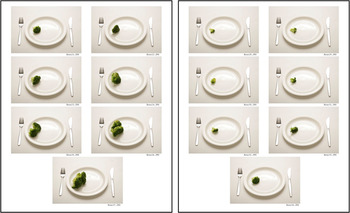
Fig. 1. (colour online) Example of seven portion photographs for estimation of amount served and leftover.

Fig. 2. (colour online) Example of guide photograph showing range of portion sizes available.
The photographs were first tested in a pilot study with 210 children aged 4–16 years. The absolute validity of children's estimates of portion size was assessed during a feeding study where children were provided with twenty-two foods, over several days, to consume at school( Reference Foster, Matthews and Lloyd 42 ). The foods were prepared to be specific portion sizes and any leftover food was weighed. Children estimated the portion size of each food using the food photographs the following day. Accuracy of children's estimates of portion size using age-appropriate photographs was not significantly different from that of adults( Reference Foster, Matthews and Nelson 43 ).
Following on from this, the relative validity of YPFA when used to estimate portion size during a nutritionist-administered interview following a 4-d non-weighed food diary, was explored. Children (n 360) aged between 18 months and 16 years were recruited along with their parent/guardian to keep a 4-d weighed food diary of all the foods and drinks consumed. The children and parent/guardian of all the primary and secondary school-aged children were then interviewed separately on the fifth day. For children of preschool age the interviews were conducted with the parent and also if applicable with nursery staff (carer). During the interview respondents were asked to give an estimate of the portion size of each food served and an estimate of any food leftover. The portion size of each food selected by the child or adult was then compared with the amount of food recorded in the weighed diary.
The precision of estimates obtained from children was seen to improve with age and this is perhaps to be expected given the cognitive development, which occurs through the age range of children in this study. By age 10 or 11 years the children were as accurate and precise as their parents in their estimates of portion size. The difference in the mean daily energy intake was an underestimate of 5 % compared with the weighed diary for estimates made by the 11–16 year olds. The limits of agreement (within which 95 % of estimates lie) were from an underestimate of 37 % to an overestimate of 43 %. Parents also underestimated energy intake by 5 % on average but the limits of agreement were wider from an underestimate of 40 % to an overestimate of 49 % (Table 2)( Reference Foster and Adamson 44 ). (YPFA is available free of charge from http://www.orderline.dh.gov.uk)
Table 2. Accuracy and precision of estimates of intake using the Young Person's Food Atlas (YPFA) by 11–16 year olds and their parents( Reference Foster and Adamson 44 )
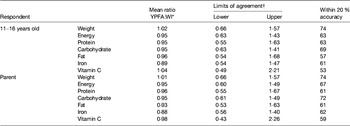
* Mean ratio is the Food or Nutrient intake reported using the YPFA divided by the Food or Nutrient intake reported using the Weighed food diary (WI).
† Limits of agreement (within which 95 % of estimates lie) are calculated as mean ratio −2sd and mean ratio +2sd.
Development of INTAKE24 an online 24-h dietary recall tool for 11–24 year olds
An online 24-h recall system that incorporates the portion-size images from the YPFA has been developed. INTAKE24 (formerly known as SCRAN24) is a self-completed computerised 24-h dietary recall system originally designed for use with children aged 11–16 years( Reference Foster, Hawkins and Delve 45 ). The system has been further developed and adapted for use with 11–24 year olds. The development of the system was an iterative process informed by four cycles of user testing. Evaluation methods including task completion measures, eye-tracking studies( Reference Duchowski 46 ) (which help identify areas of the system which the participants find confusing), think aloud techniques( Reference Jääskeläinen, Gambier and Van Doorslaer 47 ) (where the person talks through what they are thinking as they complete the recall) and post-task completion semi-structured interviews. In addition, interviewer-led 24-h recalls were conducted at the end of each round of testing to feed into the development of the system by identifying commonly missed foods and drinks. The system is based on a multiple pass 24-h recall and includes placeholders for various meals and snacks. These are displayed in chronological order; however, the user can choose to complete them in any order they wish. Each meal has a placeholder for drinks separately from foods in order to prompt people to remember this commonly forgotten element of intake. Foods are entered as free text in the ‘quick list’ phase of the recall and the user is then asked to match each food to a food in the database. Once the food type has been selected the user is asked to estimate portion size using the portion images. The default portion shown is the median portion and the size can be increased or decreased by clicking on the thumbnails or using the ‘I had less’ or ‘I had more’ buttons (Fig. 3). The system includes a series of prompts for items commonly consumed together. A final summary asks the respondent to confirm the list of foods and to have a final check for any forgotten items before submitting the recall. The recall takes about 20 min to complete. Nutrient reports can be automatically generated which include daily intakes of energy and key nutrients and food groups on an individual basis (by food, by meal and by day) and for groups of people. A relative validation against interviewer-led 24-h recalls is being conducted.
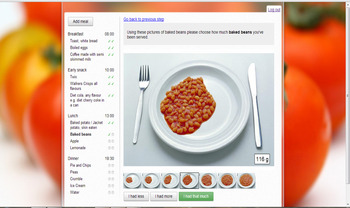
Fig. 3. (colour online) Portion size estimation screen.
Conclusions
A recent review of studies examining the validity of dietary assessment methods with children against doubly labelled water studies suggested that the 24-h recall, conducted with parents and covering at least a 3-d period is the most accurate method for reporting energy intake in children aged 4–11 years and that for younger children weighed food records provided the best estimate( Reference Burrows, Martin and Collins 26 ). Burrows et al. highlight that small sample size and inconsistencies in interpretation of the results hamper the comparison( Reference Burrows, Martin and Collins 26 ).
Additionally, there are difficulties due to inappropriate statistical methods used to assess agreement in method comparison and validation studies with a focus on group means and correlation without taking into account the precision of the method. Correlation is often used to demonstrate agreement between two methods when in fact it simply measures the strength of linear association between the methods and provides no information on magnitude of bias. Two methods may be highly and significantly correlated but one may consistently give results which are three times higher than the other.
Validation studies often compare one method against another more established method (a relative validation rather than an absolute validation). Doubly labelled water is an objective measure for validation of energy but does not give information on the vast range of foods consumed to obtain that energy intake. Likewise, biomarkers can validate the intake of specific foods or nutrients only. Observation and feeding studies mean intakes of food items and portion size can be validated in a controlled environment; however, this is only really feasible in a school or institutional setting. Ultimately, we want to know the validity of dietary assessment methods when used in a free-living environment.
Further work is required to develop ways of recording dietary intake in children which move towards that ideal with minimum perturbation of the habitual dietary behaviour of the child. Methods should not rely heavily on the child's memory, literacy or motivation and should not be prohibitively expensive. Technology such as Microsoft SenseCam( Reference Hodges, Williams and Berry 48 ) may offer the opportunity to obtain an objective measure of the foods children eat.
It is important when assessing the validity of any method of measuring dietary intake in young children that we accept the limitations that the subject's cognitive skills impose. Collecting an absolutely accurate record of intake may be impossible but by tailoring dietary methods to the specific needs of the population under investigation the accuracy of children's dietary reports can be greatly improved.
Acknowledgements
The portion sizes for the YPFA were calculated by Karen Barton, University of Dundee. The YPFA team included Stephanie Clutterbuck, Geraldine Crimmens, Adrian Hawkins and Jessica Reilly. INTAKE24 was developed by Ivan Poliakov, Dan Jackson and Patrick Olivier (Newcastle University's Culture Lab) and Jennifer Delve and Emma Simpson (Institute of Health and Society). Ethical approval for the studies was granted by Newcastle University Ethics Committee. The Authors declare no conflict of interest.
Financial Support
Development and validation of the Young Person's Food Atlas was funded by the Food Standards Agency. Development of INTAKE24 was funded by Food Standards Agency Scotland.
Conflicts of Interest
The Food Standards Agency had no role in the design, analysis or writing of this article.
Authorship
The manuscript is an overview of a presentation by Dr Emma Foster at the Irish Section Meeting of the Nutrition Society at Dublin Technical College, Dublin in June 2013. The manuscript was composed by Emma Foster and reviewed and edited by Ashley Adamson.









