Introduction
Malnutrition, including wasting or low weight-for-height, stunting or low height-for-age, and underweight or low weight-for-age, micronutrient deficiencies, and overweight/obesity, are public health problems that can affect children aged less than 60 months. While the number of stunted children worldwide has decreased in recent years, the number of overweight children has increased, and the total number of children affected by stunting and overweight is approximately 189 million(1). The World Health Organization (WHO) in 2019 reported that undernutrition and overweight/obesity coexist together in more than one-third of low- and middle-income countries(Reference Popkin, Corvalan and Grummer-Strawn2). Given the potential for both ends of the malnutrition spectrum to affect neurodevelopment, it is important to consider them together.
Malnutrition leads to economic, social and health issues for families, at the community and national level(3). More importantly, severe undernutrition – defined as severe stunting (below height-for-age z-score (HAZ) minus three standard deviations (−3 SD)) and severe underweight (below weight-for-age z-score (WAZ) minus three standard deviations (−3 SD))(Reference de Onis, Borghi, Siyam and Pinol4) – impair children’s development in the short (delayed cognitive, behavioural and motor development), medium (lower intelligence quotient (IQ) and school/academic achievement) and long term (human capital), mostly in low- and middle-income countries(Reference Grantham-McGregor, Cheung and Cueto5–Reference Miller, Murray and Thomson8). It is currently unclear whether overweight and obesity impact neurodevelopment and cognition or, vice versa, whether neurodevelopmental deficits impact overweight and obesity, or both.
Despite the reduction in stunting over the last decade(1), there still exists a need to better understand if there are opportunities to mitigate the negative, long-term impact of stunting on human capital development. It is also currently unclear whether interventions can be targeted at specific aspects of neurodevelopment and cognition, taking into consideration the timing of malnutrition with the timing of cognitive neurodevelopment in early childhood. More information is also needed to understand the aspects of neurodevelopment and cognition that are affected among overweight/obese children in order to design specific interventions.
As most existing reviews discuss undernutrition and overweight/obesity separately, this scoping review was designed to extract information on both conditions from the published literature, to study their impact as compared with normo-nourished children aged 0–60 months on cognitive neurodevelopmental aspects (cognition, behavioural, motor and emotional development) in early, mid and later life. Undernutrition is defined as stunting (HAZ < −2 SD) and underweight (WAZ < −2 SD), while overweight is defined as 2 SD > WAZ < 3 SD and obesity as WAZ ≥ 3 SD)(Reference de Onis, Borghi, Siyam and Pinol4). This combined approach will conceivably allow for a more holistic view of the situation commonly found in many countries across the world.
Methods
This review followed the consistent approach of a scoping review to compile findings from studies with different designs and methodologies to answer the stated critical research questions(Reference Munn, Peters and Stern9). The research questions are as follows: (i) Which developmental aspects are affected by obesity/overweight and undernutrition during the first 60 months of life? (ii) What other factors can modify these outcomes? (iii) Which factors can mitigate the impact of obesity/overweight and undernutrition on neurodevelopment and cognition? (iv) Is the effect on cognitive neurodevelopment partly or fully reversible? and (v) What are the implications for intervention strategies?
Literature published from 1 January 2009 to 31 October 2019 in the PubMed and Cochrane databases was retrieved using formulated search terms. The title and abstract of each article retrieved were screened based on the inclusion criteria by all authors. A simple grading of controlling study biases using JADAD criteria for randomised controlled studies, Newcastle Ottawa Scale for cohort studies, and National Heart, Lung and Blood Institute (NHLBI) criteria for observational cross-sectional studies were then conducted by five authors (A.S., M.Y.J., P.B.K., L.M. and J.G.) to select studies for further qualitative analyses (Tables 1 and 2). References of relevant narrative reviews (cross-references) were also examined to search for further studies that met the inclusion criteria. J.G. and L.M. then independently extracted data from the identified full-text articles. Data extraction tables incorporated important information from eligible full texts to allow the extraction of significant information for the review.
Table 1. Key findings from retrieved observational studies on growth and the impact on neurodevelopment and cognition

Table 2. Key findings from retrieved interventional studies on undernutrition and the impact on neurodevelopment and cognition

Results and discussion
Descriptive summary of included studies
From the ninety-one articles originally identified through the search strategy, twenty-six full-text articles were selected after a review of cross-references in eligible narrative reviews. The full text was used for information extraction and grading for quality assessment (Fig. 1).

Fig. 1. PRISMA 2009 flowchart diagram.
Information was categorised based on the type of study and nutritional status of the children (Tables 1 and 2) as well as by factors influencing the impact of nutritional status on cognitive neurodevelopment (Table 3). Information was extracted from fourteen observational studies (undernutrition (n = 8 articles), normo-nutrition (n = 5 articles) and overweight/obesity (n = 1 article), four intervention trials (undernutrition (n = 2 articles) and normo-nutrition (n = 2 articles)), four systematic reviews (undernutrition (n = 1 article), normo-nutrition (n = 2 articles) and overweight/obesity (n = 2 articles)) and four meta-analyses (all on undernutrition). All publications on under- and normo-nourished children were conducted in low- to middle-income countries, while all articles about overweight/obese children reported data from high-income countries. No intervention study was retrieved on overweight/obese children. Approximately 85 % (n = 22) of the retrieved literature had good quality in controlling bias.
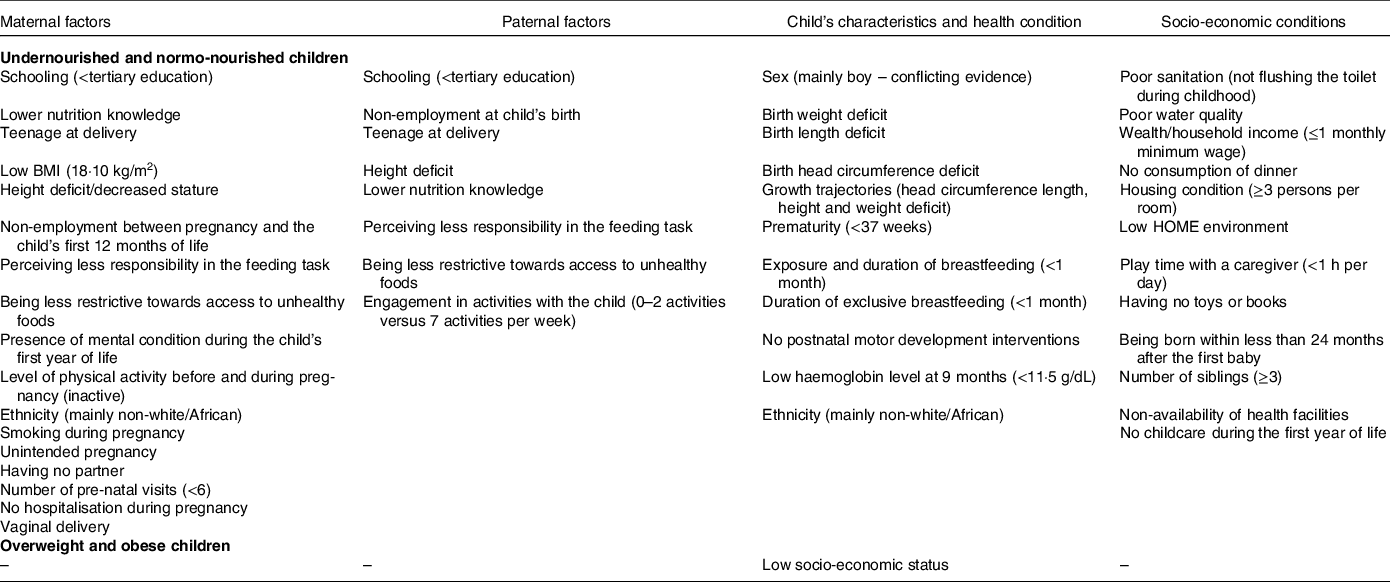
Table 3. Factors influencing suboptimal growth in neurodevelopment and cognition

HOME, Home Observation for Measurement of the Environment
To the best of our knowledge, this review complements previous meta-analyses and systematic reviews(Reference Sudfeld, McCoy and Danaei6–Reference Miller, Murray and Thomson8) and includes a wider spectrum of suboptimal nutritional status (ranging from mild/moderate to severe underweight and stunting to overweight/obesity) during the first 60 months of life on various neurodevelopment aspects (cognition, motor development, temperament, socio-economic status, and academic achievement) that manifest from infancy through school-age to adulthood (Fig. 2). This review also covers observational longitudinal cohorts and interventional studies with nutrition- and non-nutrition-related interventions on the outcomes of interest.
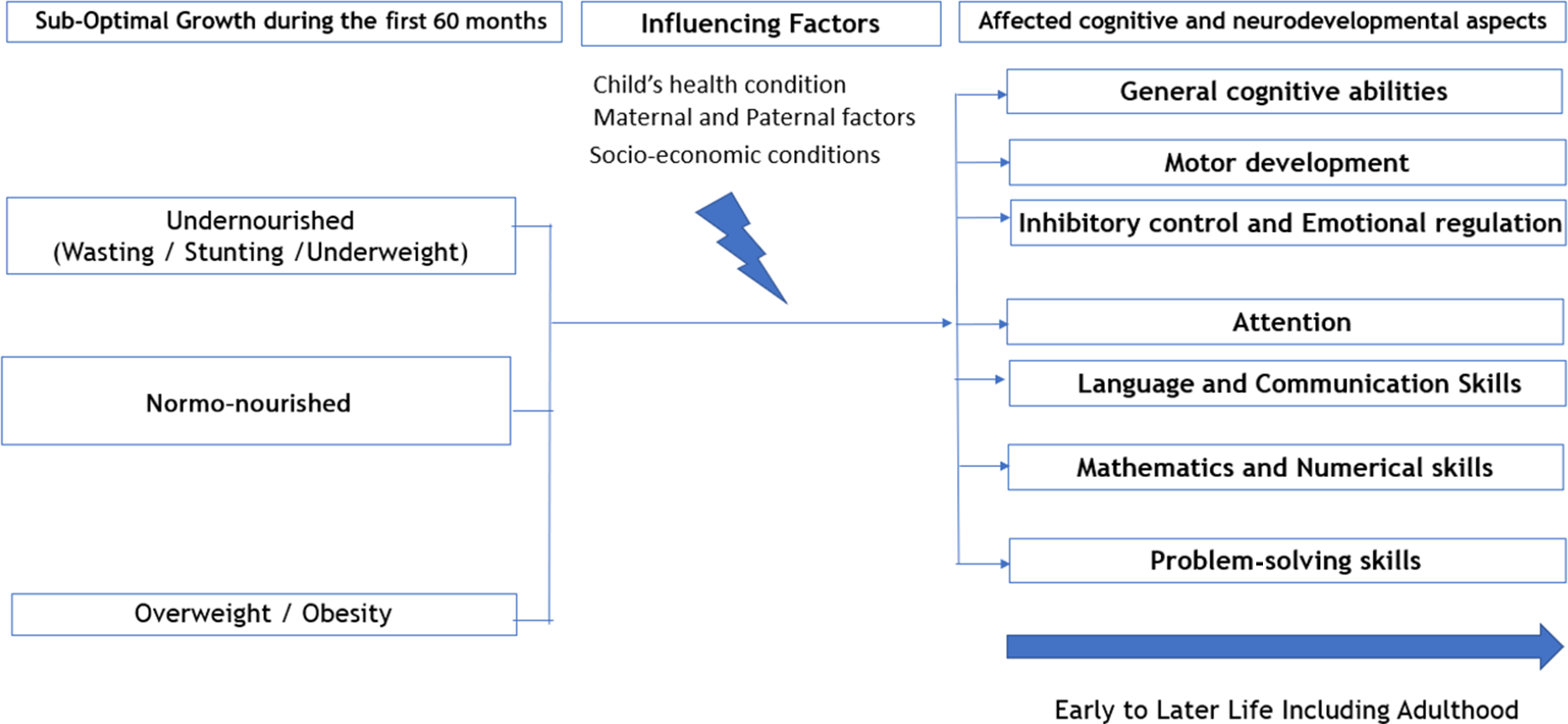
Fig. 2. Impact of suboptimal growth in early childhood on developmental-related aspects.
The importance of monitoring weight, length and head circumference during the first 24 months of age
From the reviewed studies, length-for-age z-scores (LAZ) and height-for-age z-scores (HAZ) (anthropometric measures of stunting in children) were associated with various elements of cognitive functioning, such as attention span, time to proper walking, mathematics and language abilities in early life, and income and choice of partner/age at marriage in later life (Table 1). It was reported that healthy infants in the highest quartile of neonatal weight-, length- and head circumference-gain during the first 4 weeks of life had higher IQ scores at 6 years of age than those in the lowest quartile(Reference Camargo-Figuera, Barros and Santos10).
From a longitudinal study in the Philippines, regardless of HAZ categories at 6 months (defined as moderate/severe stunting (HAZ < −2), mild stunting (−2 ≤ HAZ < −1), at risk of stunting (−1< HAZ < 0), or normal height (HAZ ≥ 0)), more gain (or less loss) in HAZ after the age of 6 months was positively associated with cognitive function at 11 years of age. In addition, changes in HAZ from 6 to 24 months and changes in HAZ from 24 months to 11 years were also positively associated with cognitive ability at 11 years in the same study(Reference Cheung and Ashorn11). These outcomes are similar to the results among children in Bangladesh. In this study, cognitive impairment was associated with poverty, birth condition and postnatal growth that started at 7 months of age and worsened up to 64 months when it became even more substantial(Reference Hamadani, Tofail and Huda12). The impact of the timing of stunting is still unclear. One study reported that stunting in the second year of life is more harmful than stunting before 12 months of age(Reference Mendez and Adair13). Another study reported that higher HAZ at 4–6 years of age among healthy Malaysian children significantly contributed to higher cognitive function after controlling for socio-demographic background, parent’s nutrition knowledge and dinner consumption (DR2 = 0·009, DF = 18·605, p < 0·001)(Reference Mohd Nasir, Norimah and Hazizi14).
Evidence for the impact of underweight and stunting on the development of emotional skills is largely variable across the identified studies. Two meta-analyses that described data from lower- and middle-income countries showed the limited influence of undernutrition on a child’s attachment, emotionality, social competence and temperament(Reference Sudfeld, McCoy and Danaei6,Reference Miller, Murray and Thomson8) . However, in a study among Bangladeshi children aged 6–24 months comparing undernourished (n = 212) and better-nourished (n = 108), it was reported that severely underweight children (WAZ < −2) were less sociable, less attentive, and more fearful and had more negative emotional traits than normo-nourished children. The effect size of these temperament differences, which were assessed using validated interviewer-administered questionnaire to parents, were small to moderate(Reference Baker-Henningham, Hamadani and Huda15). There is evidence, therefore, that underweight and stunting impact social skill development. Low HAZ and WAZ correlated strongly with children having less schooling or needing a longer time to complete schooling(Reference Crookston, Schott and Cueto16), and in later life, with lower income and living in a less conducive environment, such as having a higher number of pregnancies and having the first child at a younger age(Reference Hoddinott, Behrman and Maluccio17).
Improvements in linear growth and potential window of opportunity for neurodevelopment and cognitive abilities recovery
This review further strengthens the importance of the first 1000 days of life as a window of opportunity for rescuing neurocognitive deficits. It was reported that HAZ velocity between 6 and 24 months among undernourished children is positively associated with cognitive function(Reference Cheung and Ashorn11) and that every 1-unit increase in HAZ before the age of 24 months is associated with a higher increment in motor, communication and cognitive ability scores at 26–80 months of age compared with a 1-unit increase in HAZ after 24 months of age(Reference Sudfeld, McCoy and Danaei6, Reference Crookston, Schott and Cueto16).
Data from the Young Lives cohort in Ethiopia, India, Peru, Cambodia and Vietnam indicated that children who were in the recovered group (stunted at 12 months of age but not stunted at 8 years of age) had better academic achievement (maths scores, receptive vocabulary scores, and reading comprehension scores) than those who stayed persistently stunted(Reference Crookston, Schott and Cueto16). However, their academic achievement was still lower than those who had never been stunted. This finding is consistent with the finding from another cohort in Malawi, which reported that those who had recovered from stunting had better academic achievements at 11 years of age than those who were persistently stunted from age 4 to 8 years(Reference Sunny, DeStavola and Dube18). Based on the above, it appears likely that the period in which neurocognitive deficits can recover following appropriate interventions goes beyond the age of 2 years, up until 8 years of age, which is in line with prefrontal cortex development and ongoing synaptogenesis at that age(Reference Grantham-McGregor, Cheung and Cueto5). Interestingly, another study reported that children who were stunted at 24 months of age and experienced catch-up growth often did worse on cognitive tests at 4–5 years of age than children who were never stunted and did almost as poorly as children who had remained stunted(Reference Casale, Desmond and Richter19). This finding appears to contradict previously stated findings from the Young Lives and Malawi cohorts. It is important to note, however, that the exact definition of ‘catch-up’ plays a critical role in this observation. Recently, five definitions were formulated for ‘catch-up growth’, ranging from lenient to strict: I: increase in HAZ; II: recovery from stunting (HAZ at 5 years > −2); III: increase in height-for-age difference; IV: recovery from stunting and increase in height-for-age difference; and V: recovery from stunting with a stricter cut-off point, where HAZ falls within ‘normal’ range (HAZ at 5 years > −1)(Reference Desmond and Casale20). The observation reported above is based on definitions I–IV of ‘catch-up’. Thus, the term ‘catch-up’ should be carefully defined when determining the optimal goal for catch-up growth to recover neurodevelopment and, consequently, cognitive ability in later life.
The importance of interventions in improving cognitive outcomes among undernourished children
Seven publications assessed the effectiveness of intervention studies in improving cognitive outcomes among undernourished children. The publications covered three randomised controlled trials, two systematic reviews and two meta-analyses. The overall quality of these studies was judged as good when considering the risk for bias (Table 2).
Stunted children with high levels of plasma homocysteine and those who were younger than 24 months at the end of the follow-up period showed the largest improvement in gross motor function and problem-solving skills after being supplemented with vitamin B12 on a daily basis(Reference Kvestad, Taneja and Kumar21). In contrast, the effect of the vitamin/nutrition intervention on recovering or maintaining normal neurodevelopment and cognitive deficits in normo-nourished children remained inconclusive(Reference Prado, Larson and Cox7,Reference Kvestad, Taneja and Kumar21,Reference Rosado, Lopez and Garcia22) . No benefits in growth or cognitive performance were reported among 422 healthy children aged 12–24 months receiving daily multi-micronutrient supplementation (iron and zinc)(Reference Rosado, Lopez and Garcia22). This finding is in contrast with an intervention trial in which multiple micronutrients were supplemented (vitamins B12, A, C, folic acid and iron), with and without responsive stimulation, for approximately 20 months among 1489 mother–child pairs in Pakistan. In this study, children who were exposed to the enhanced nutrition intervention had, regardless of their nutrition status, significantly higher developmental scores (cognitive, language and social–emotional scales) at 12 months than the control group(Reference Yousafzai, Rasheed and Rizvi23). Another group of children who received responsive stimulation had significantly higher developmental scores on the cognitive, language and motor scales at 12 and 24 months of age and on the social emotional scale at 12 months of age than the control group. In comparison, the treatment effect on cognition, language and motor development at 24 months was moderate to large for responsive simulation and was low to moderate for the enhanced nutrition group(Reference Yousafzai, Rasheed and Rizvi23). This study also found that linear growth in children exposed to enhanced nutrition was significantly greater at 6 and 18 months compared with those not exposed to enhanced nutrition(Reference Rosado, Lopez and Garcia22).
A recent systematic review and meta-analysis that assessed the impact of nutrition with or without stimulation interventions concluded that parent-led responsive learning, more than nutrition supplementation, appeared to have a stronger influence on the neurodevelopment of children aged 0–60 months(Reference Prado, Larson and Cox7). This systematic review, which was based on seventy-five retrieved studies from various databases, reported that the pooled effect of these supplementations is one-fourth smaller than the pooled effect size of responsive care and learning opportunities on cognitive, language and motor scales. The review also suggested that postnatal multiple nutrient supplementation can improve linear growth in children and, to a smaller extent, cognitive development and socio-temperament, while interventions promoting responsive care and learning opportunities affect only cognitive development but not linear growth(Reference Prado, Larson and Cox7).
The impact of overweight/obesity on neurodevelopment and cognition
Only one cross-sectional study and two systematic reviews that were retrieved described the impact of overweight/obesity on cognitive neurodevelopmental aspects(Reference Morano, Colella and Caroli24–Reference Reinert, Po’e and Barkin26) (Table 1). All studies seemed to point towards a more limited impact of overweight/obesity on aspects of neurodevelopment and cognition in the studied affluent populations in contrast with those describing the impact of undernutrition. All retrieved literature demonstrated that attention, executive control (inhibitory control, working memory, reward sensitivity, and impulsivity) and gross motor skills were the most affected areas.
A study among overweight Italian children showed poorer gross motor skills in overweight children than their normal-weight peers(Reference Morano, Colella and Caroli24), while other systematic reviews reported poorer executive control and more difficulty with inhibition in overweight children than in healthy weight children(Reference Liang, Matheson and Kaye25,Reference Reinert, Po’e and Barkin26) . There is a suggestion of directionality in the association between obesity and executive function. Children with lower executive function are speculated to have lower self-regulation of energy intake and decreased participation in physical activity, which leads to or potentiates overweight or obesity. It was also reported that low executive function stimulates excess adiposity, leading to exacerbating decrements in executive function in childhood(Reference Hayes, Eichen and Barch27). On the other hand, various studies have shown that child obesity or early-life adiposity reduces executive function via several biological mechanisms. Pro-inflammatory cytokines produced by adipose tissue can stimulate inflammatory pathways in all age categories, leading to cognitive development deficits, and dysregulation of appetite-regulating hormones could further harm cognitive skills(Reference Reinert, Po’e and Barkin26). Although there is limited affected cognitive neurodevelopmental areas reported in these affluent populations, the effect may be more diverse and pronounced in less-affluent societies. In conclusion, poor gross motor skills, which are correlated with less physical activity(Reference Liang, Matheson and Kaye25) and reduced attention span(Reference Liang, Matheson and Kaye25,Reference Reinert, Po’e and Barkin26) , should be taken into consideration when designing intervention programs for these overweight/obese children.
Factors influencing the impact of suboptimal growth on neurodevelopment and cognition
From the literature, there seem to be similarities in influencing factors between undernutrition and overweight/obesity on cognitive neurodevelopment, but far more research is needed to further understand the latter. These factors can be classified into maternal and paternal factors, child characteristics and health conditions, and socio-economic factors (Table 3).
Several pregnancy-related maternal parameters, such as maternal weight gain and smoking, have been consistently reported to increase the impact of suboptimal growth on cognitive neurodevelopment in addition to infant condition at birth, such as low birth weight and short length at birth, suggesting the importance of prenatal nutrition and maternal health for later life(Reference Hamadani, Tofail and Huda12,Reference Baker-Henningham, Hamadani and Huda15,Reference Casale, Desmond and Richter19,Reference Walker, Chang and Younger28,Reference Nguyen, DiGirolamo and Gonzalez-Casanova29) .
The influence of sex on suboptimal growth and cognitive neurodevelopment appeared conflicting in the literature; normo-nourished and undernourished girls had slightly higher intelligence scores(Reference Camargo-Figuera, Barros and Santos10), social maturity(Reference Casale, Desmond and Richter19), and manageability(Reference Baker-Henningham, Hamadani and Huda15) than boys with the same nutritional status. In contrast, another study found that normo-nourished boys tended to have higher intelligence score as compared with normo-nourished girls(Reference Mohd Nasir, Norimah and Hazizi14).
Particularly among undernourished children, it appeared that parents with a low level of education and nutritional knowledge, those who perceived less responsibility in the parenting task, or those who were less restrictive towards access to unhealthy foods had children who experienced suboptimal growth with resultant impaired cognitive development(Reference Sudfeld, McCoy and Danaei6,Reference Mohd Nasir, Norimah and Hazizi14) .
Diet quality was demonstrated to be a positive predictor of improved cognitive outcomes in these children(Reference Sudfeld, McCoy and Danaei6,Reference Mohd Nasir, Norimah and Hazizi14) . For instance, food fortified with calcium, iron, zinc, vitamin B2 and protein was associated with improved cognitive outcomes because of the probable role of these nutrients in early brain development(Reference Prado, Larson and Cox7,Reference Yousafzai, Rasheed and Rizvi23) . In contrast, a lack of dietary protein may delay or inhibit brain and cognitive development(Reference Sudfeld, McCoy and Danaei6,Reference Kristjansson, Francis and Liberato30) . On that note, recent evidence proposed supplementation of animal protein, in particular cow’s milk, as an essential component of a child’s diet to prevent undernutrition and to improve cognition(Reference Pimpin, Kranz and Liu31–Reference Lee, Singh and van Liefde33).
Low socio-economic status was reported to be correlated with the impact on neurodevelopment and cognition among undernourished and overweight/obese children in several studies(Reference Sudfeld, McCoy and Danaei6,Reference Camargo-Figuera, Barros and Santos10,Reference Yousafzai, Rasheed and Rizvi23,Reference Walker, Chang and Younger28,Reference Nguyen, DiGirolamo and Gonzalez-Casanova29,Reference Smithers, Golley and Mittinty34,Reference Miller, Lee and Lumeng35) . The Home Observation for Measurement of the Environment (HOME) parameter was used as a proxy indicator of socio-economic status. It was developed to measure responsiveness and stimulation in the home environment and parental behaviours. HOME consisted of questions, among others, on homeownership and possession of books and toys. The tool needs to be validated to accommodate sociocultural differences(Reference Nguyen, DiGirolamo and Gonzalez-Casanova29,Reference Bradley36) .
Limitations and strengths of the review
First, chronic illnesses and hospital malnutrition were excluded, although they could have a similar impact on overall developmental aspects. A second limitation is that the HOME instrument as an indicator of socio-economic status must be adjusted to various sociocultural conditions in each group or country. In addition, the statistical significance of pooled effects of all studies combined was not calculated, as this review is of scoping nature and not a systematic review. Furthermore, the search strategy may have missed some relevant papers because of the search scope that limited peer-reviewed research papers to those published in the past decade only. To overcome this issue, reviewing reports outside the peer-reviewed literature (i.e. grey literature) should be done in the future.
One of the strengths of this scoping review is that it expeditiously provides comprehensive and updated scientific evidence for healthcare professionals and policymakers. The synthesised evidence may allow key stakeholders to plan and to execute necessary intervention programs for preventing and managing suboptimal growth, with a focus on achieving optimal cognitive potential in young children. In addition, this scoping review was conducted using specific methodological approaches that would allow more accuracy in literature screening with less bias. A cross-referencing of eligible studies from retrieved narrative reviews enhanced the completeness of the evidence and enabled the retrieval of information on not only the populations that experience undernutrition and overweight/obesity but also the general population that identified children with faltering growth. It also enabled the retrieval of studies from various geographical areas (low- to high-income studies) as well as studies on various developmental deficits. Emphasis had been hitherto placed on the impact of malnutrition in children on morbidity and mortality; in contrast, this review points to the quality of life that may be affected by suboptimal nutrition on neurodevelopment and cognition. From a public health perspective, prevention of childhood malnutrition must be addressed not only by economic empowerment but also through health promotion and education as well as policy.
Consideration for future research and actions:
-
1) More studies should be conducted on the impact of nutritional/behavioural interventions in overweight/obese children on neurodevelopment and cognition, especially in low-income countries, as the currently retrieved literature all came from high-income countries. Overweight/obesity in childhood is on the rise and can coexist with undernutrition within the same population, for example, as seen in India and Indonesia. Approximately, 39 and 7 million children under the age of 5 years are stunted in India and Indonesia,respectively, and more than 3.6 million children in the same age group areoverweight and obese in these two countries. This amounts to a total of around 50 million children who are at risk of suboptimal neurodevelopment and cognitivefunction(3). In addition to the negative consequences of undernutrition, an increase in childhood obesity prevalence can lead to adverse long-term consequences on human capital in these countries.
-
2) Intervention studies for both undernutrition and overweight/obesity must assess the association between these nutritional statuses and cognitive neurodevelopment, as most interventions usually focus only on providing nutrients related to brain development and not for optimal growth and vice versa as also suggested by Prado et al.(Reference Prado, Larson and Cox7). For example, several recently published studies and systematic reviews assessed the impact of animal-based food supplementation or milk interventions on either growth among stunted children or only cognitive neurodevelopment, but not on both aspects simultaneously(Reference Pimpin, Kranz and Liu31,Reference Sjarif, Yuliati and Iskandar32) .
-
3) Optimally, any program or intervention for growth monitoring in the community or hospital settings should engage a multidisciplinary team of health care professionals. Depending on the local conditions, such a team could consist of nutritionists, general practitioners, paediatricians and/or behavioural specialists(37). Multidimensional approaches involving various relevant stakeholders need to address all issues simultaneously as the root causes are quite complex. These could include improving housing and sanitation levels, ensuring parental job security and adequate social welfare, improving parental education attainment and nutritional knowledge, and providing access to adequate nutrient intakes for catch-up growth among underweight or stunted children as well as to affordable healthy food for those who are overweight/obese especially those in the low socio-economic category. Actions taken should tackle both undernutrition and overweight/obesity concurrently – not just one or the other – to ensure successful and comprehensive outcomes in terms of childhood growth and cognitive neurodevelopment.
Conclusion
Undernutrition and overweight/obesity during the first 60 months of postnatal life affect the cognitive neurodevelopmental trajectories of children later in life. Weight and length/height need to be monitored even beyond 24 months of life to enable early recognition of growth retardation/deviations and to allow appropriate and timely interventions to address their negative neurodevelopmental and cognitive impacts. Given the Global Nutrition Targets for 2025(38), intervention programs should leverage multidimensional approaches that address not only childhood undernutrition but also overweight/obesity and improve socio-economic conditions. Nutrition interventions for catch-up growth among undernourished children can potentially recover neurocognitive development up to the age of 8 years, particularly in those whose nutrition status have improved. These specific, targeted and simultaneous interventions may be key to safeguarding future human capital, especially in countries with a high prevalence of stunting, overweight/obesity or both.
Declarations
Acknowledgements
The authors thank Content Ed Net Singapore for providing editorial and medical writing assistance in retrieving relevant publications and the development of the first drafts of the manuscript.
Funding
FrieslandCampina supported the retrieval of relevant publications and the development of the early first manuscript drafts by Content Ed Singapore. None of the authors received an educational grant from FrieslandCampina to participate in the writing.
Author contributions
All authors were involved in setting the concept, objective and selection criteria for the review. All authors were also involved in the selection of eligible articles based on titles and abstracts. A simple grading of controlling study biases was then conducted by five authors (A.S., M.Y.J., P.B.K., L.M. and J.G.). Afterwards, L.M. and J.G. selected eligible articles based on full texts. All authors provided agreement on the final included articles. All authors participated in data extraction, synthesis and interpretation. All authors provided inputs and agreed on the final version of the manuscript.
Competing interests
Verena Tan was an employee of FrieslandCampina at the time of the manuscript’s development. Leilani Muhardi and Jan Geurts were employees of FrieslandCampina at the time of the manuscript’s development, submission and revision.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.