Introduction
Admission to nursing home is a frequent surrogate for poor outcome in stroke research, but a more fulsome characterization of patients after institutionalization is lacking.Reference Krueger, Koot, Hall, O’Callaghan, Bayley and Corbett1,Reference Reeves, Bushnell and Howard2 Further, sex differences in patient characteristics and care needs at entry to nursing home following stroke and subsequent survival are not well understood,Reference Reeves, Bushnell and Howard2–Reference Gattringer, Ferrari and Knoflach4 but quantifying these potential differences may help to improve and individualize care after stroke.
Women are more likely than men to be admitted to nursing home following a stroke.Reference Reeves, Bushnell and Howard2–Reference Petrea, Beiser, Seshadri, Kelly-Hayes, Kase and Wolf5 Women tend to be older than men at the time of their first stroke and present with more severe strokes, which may explain some of the difference in nursing home admissions.Reference Reeves, Bushnell and Howard2,Reference Lisabeth, Reeves and Baek6,Reference Phan, Reeves and Blizzard7 However, there may be other contributing factors. Living alone or without a spouse is associated with an increased need for nursing home placement after stroke, and some studies suggest that increased levels of social support may delay institutionalization.Reference Lisabeth, Reeves and Baek6,Reference Katz, Kabeto and Langa8,Reference Blackburn, Albright and Haley9 In stroke populations, women are more prone to social isolation than men because they are older, less likely to be married, and more likely to be living alone.Reference Reeves, Bushnell and Howard2,Reference Bushnell, Reeves and Zhao10 It is not clear if women are more likely to be institutionalized than men after stroke because they are more functionally disabled poststroke or if women are more likely than men to lack sufficient social support to enable their return to the community. If women are observed to have fewer care needs than men at admission to nursing home after stroke and lower mortality, interventions to promote community reintegration may be needed.
We aimed to determine whether sex differences exist in the characteristics, care needs, and survival of new nursing home residents admitted after stroke. We hypothesized that women may have fewer care needs and lower mortality than men and that they may be older, less likely to be married, and more likely to be living alone prior to nursing home admission.
Methods
We used linked population-based administrative and clinical data to identify adult patients (aged 18–110 years) discharged alive from an acute care hospital following stroke between April 1, 2011 and March 31, 2016, and who were subsequently admitted to a nursing home within 180 days. Patients with ischemic stroke and intracerebral hemorrhage were identified using the International Classification of Diseases 10th Revisions (ICD-10) codes H34.1, I63.x, I64.x, and I61.x coded as the most responsible diagnosis.Reference Kokotailo and Hill11 Patients were followed until March 31, 2018. We excluded patients who were not residents of Ontario, those without a valid health insurance number, patients living in a nursing home prior to stroke, as well as those with any stroke events occurring in-hospital during an admission for a different health condition.
Health administrative datasets (Supplementary Table S1) were linked using unique encoded identifiers and analyzed at ICES. We used the Resident Assessment Instrument-Minimum Data Set version 2.0 (RAI-MDS 2.0) to determine care needs upon admission to nursing home. Patients without a RAI-MDS 2.0 assessment within 14 days of admission to a nursing home were excluded. These databases have been used extensively in health services research.Reference Juurlink, Preyra and Croxford12
The primary outcomes were care needs measured using validated clinical and functional scales in the RAI-MDS 2.0, including the Activities of Daily Living Hierarchy Scale (a 6-point scale with scores ≥ 3 indicating total dependence requiring extensive supervision), the Depression Rating Scale (a 14-point scale with scores ≥ 3 indicating the presence of depressive disorder symptoms), the Cognitive Performance Scale (a 6-point scale with scores ≥ 2 indicating the presence of cognitive impairment), the Aggressive Behaviour Scale (12-point scale with scores ≥ 1 indicating the presence of aggression), the Pain Scale (a 3-point scale with scores ≥ 1 indicating the presence of pain), the Index of Social Engagement (a 6-point scale with scores < 6 indicating lower levels of engagement), the Changes in Health, End-stage Disease, and Signs and Symptoms Scale (5-point with scores ≥ 2 indicating health instability and risk of poor outcomes).Reference Morris, Fries and Morris13–Reference Maclagan, Maxwell and Gandhi17 Frailty status was assessed using a 72-item index derived using a cumulative deficits approach from items in the RAI-MDS 2.0 and categorized as 0.0–0.3 = non-frail or pre-frail versus >0.3 = frail.Reference Maclagan, Maxwell and Gandhi17,Reference Campitelli, Bronskill and Hogan18 The secondary outcome of all-cause mortality was assessed following nursing home admission until March 31, 2018. The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act.
Statistical Methods
Patient characteristics were described by sex using proportions for categorical variables and medians and interquartile ranges (IQRs) for continuous variables. We calculated unadjusted prevalence ratios and associated 95% confidence intervals (CIs) for care needs comparing women to men in all patients admitted to a nursing home following stroke discharge. These estimates were also stratified by age (categorized as 18–64, 65–74, 75–84, and over 85 years), marital status (categorized as married vs. not married, including patients who were never married, widowed, separated, divorced, and unknown status), and baseline living situation (living alone vs. not).
We investigated sex differences in all-cause mortality after admission to nursing home by plotting Kaplan–Meier survival estimates in men and women and comparing them using the log-rank test. Survival curves were plotted for the overall cohort and stratified by age. We used propensity score matching to account for differences in characteristics at admission to nursing home between men and women.Reference Austin19 The propensity score was estimated using a logistic regression model, in which sex was regressed on all measured baseline covariates, including sociodemographic characteristics, comorbidities, care needs, and care trajectories, including whether the patient had been admitted to inpatient rehabilitation, complex continuing care, readmitted to acute care, or utilized home care services between discharge from acute care and admission to nursing home. Men and women were matched on age (± 2 years) and the logit of the propensity score, using calipers equal to 0.2 of the standard deviation of the logit of the propensity score.Reference Austin20 Characteristics of men and women before and after matching were compared using standardized differences.Reference Austin21 Standardized differences of <0.1 were used to indicate adequate balance. The rate of all-cause mortality was compared between men and women in the matched sample using a Cox proportional-hazards regression model in which the hazard of all-cause death was regressed on sex. Each individual was followed from nursing home admission until death or the end of the study period on March 31, 2018 (at which point they were censored), whichever came first. A robust variance estimator was used to account for the matched nature of the sample.Reference Austin22 All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Among 54,545 patients discharged alive after stroke, 4853 were newly admitted to nursing home within 180 days. After excluding patients who were nonresidents of Ontario (n = 6) and those who did not have a full RAI-MDS 2.0 assessment within 14 days of admission to nursing home (n = 16), analyses were performed on 4831 (8.9%) patients, of whom 60.9% were women. Table 1 shows the baseline characteristics of the cohort by sex. Compared to men, women were older (median age [IQR]: 84 years [78, 89] for women vs. 80 [71, 86] years for men), less likely to be married (21.9% women vs. 50.4% men), and more likely to live alone at baseline (20.8% women vs. 16.9% men). Sex differences in care trajectories between discharge from acute care and admission to nursing home are shown in Supplementary Table S2.
Table 1: Baseline characteristics of patients with stroke newly admitted to nursing homes by sex (n = 4831)

IQR = interquartile range; SD = standard deviation; S-Diff = standardized differences; COPD = Chronic Obstructive Pulmonary Disease.
Standardized differences of <0.1 indicate adequate balance.
a Includes patients who were widowed, divorced, separated, never married, and unknown status.
At nursing home admission, women were more likely than men to be frail (62.1% women vs. 53.7% men), have unstable health (21.3% women vs. 14.7% men), experience symptoms of depression (22.8% women vs. 18.3% men) and pain (48.4% women vs. 39.9% men, Table 2). Women were less likely than men to exhibit aggressive behaviors (31.3% women vs. 35.9% men). The prevalence ratios and 95% CI for care needs comparing women to men for the overall cohort are shown in Figure 1, and stratified analyses by age, marital status, and baseline living situation are shown in Supplementary Table S3.
Table 2: Health services care needs at nursing home admission by sex (n = 4831)
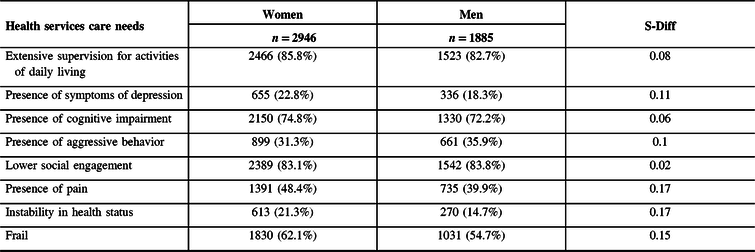
S-Diff = standardized differences.
Standardized differences of <0.1 indicate adequate balance.

Figure 1: Prevalence ratios of care needs among newly admitted nursing home residents with stroke in Ontario, Canada, comparing women to men (n = 4831).
The median follow-up time was 2.33 years (IQR: 0.98, 3.73) for women and 2.31 years (IQR: 0.91, 3.73) for men. The overall median survival following nursing home admission was 2.9 years, 95% CI (2.7, 3.1). In the unadjusted age-stratified analyses, there was no sex difference in the Kaplan–Meier survival analysis among patients younger than 75 years of age, but women had lower mortality than men among those aged 75 years or older (Figure 2).

Figure 2: Age-stratified Kaplan–Meier survival curves of men and women with stroke after admission to nursing home (n = 4831).
Following propensity score matching, 1364 pairs were matched (Supplementary Table S4) and included 46.3% of women and 72.4% of men in the original cohort. Men and women were well balanced in their baseline characteristics, care needs, and health care utilization, except for the length of stay in inpatient rehabilitation (median days [IQR]: 47 [31, 65] women vs. 50 [34, 72] men). In the propensity-score-matched analysis, women had a lower hazard of mortality compared to men (hazard ratio 0.85 and 95% CI [0.77, 0.94], p < 0.001, Figure 3).

Figure 3: Survival following nursing home admission in propensity-score-matched cohort of men and women with stroke (n = 1364 pairs).
Discussion
The majority of stroke survivors newly admitted to nursing home were women. Compared to men, women were more likely to be living alone prior to their stroke and less likely to be married. Women had lower mortality than men over time, but they had more care needs. Our results suggest that simply evaluating the need for nursing home admission as a surrogate for poor outcome without understanding the care needs at admission or the subsequent survival incompletely captures the experience of the most severely disabled stroke survivors and may particularly underestimate the burden of stroke on women.
Sex differences in stroke care delivery have been previously described and span issues of prevention, access, and outcomes. For example, women with atrial fibrillation are less likely to receive oral anticoagulation or more likely to be treated with conservative doses compared to men,Reference Jonsson, Ek and Kremer23,Reference Avgil Tsadok, Jackevicius, Rahme, Humphries and Pilote24 women with minor strokes are at higher risk of misdiagnosisReference Newman-Toker, Moy, Valente, Coffey and Hines25 and those with severe strokes are less likely to be treated with intravenous thrombolysis despite similar eligibility criteria.Reference Reeves, Bhatt, Jajou, Brown and Lisabeth26,Reference Reid, Dai, Gubitz, Kapral, Christian and Phillips27 Whether closing these gaps in stroke care can decrease the number of women requiring nursing home or reduce their care needs at nursing home admission deserves dedicated evaluation.
Quantifying sex differences in the care needs at admission to nursing home may help identify opportunities to improve care. Consistent with prior reports, we found that women were more likely than men to report symptoms of pain and depression, two potentially treated symptoms.Reference O’Donnell, Diener, Sacco, Panju, Vinisko and Yusuf28,Reference Park and Kim29 Pain after stroke can be related to musculoskeletal conditions, neuropathic in nature, as well as due to complications of immobility, such as pressure ulcers or reflex sympathetic dystrophy.Reference Delpont, Blanc, Osseby, Hervieu-Begue, Giroud and Bejot30 Symptoms of depression after stroke are associated with the severity of disability and pain, and may be potentially influenced by patient preferences for end-of-life care, which may differ in men and women.Reference Duffy, Jackson, Schim, Ronis and Fowler31 Understanding why women are more likely to experience these symptoms in nursing home than men may help tailor treatments to individual needs and improve quality of life.
We found that women had decreased mortality over time compared to men in the propensity-score-matched cohort. The survival advantage in women has been also reported in residents admitted to nursing home for non-stroke conditions.Reference Buchanan, Wang, Ju and Graber32,Reference Luppa, Luck, Weyerer, Konig and Riedel-Heller33 However, only 46.3% of the women in the total cohort were matched to men. The age-stratified survival curves indicated that only women aged 75 years and older had lower mortality than men.
An important strength of the current study is the use of a population-based patient sample in the setting of a universal health care system with mandatory reporting of health services and standardized clinical assessments in nursing home. Our study nevertheless had several limitations. We were not able to determine advanced care directives, which are important for understanding long-term survival and may be different for men and women.Reference Duffy, Jackson, Schim, Ronis and Fowler31 We did not have information on caregiver supports in the community, race/ethnicity, stroke severity, stroke etiology, or quality of life measures, as these are not available in administrative data.Reference Yu, Holodinsky and Zerna34 While financial incentives may motivate the overestimation of care needs, we do not think that any potential misclassification of care needs would differentially affect men or women.Reference Sukul, Hoffman and Nuliyalu35 Finally, we were only able to examine baseline differences after admission to nursing home and did not have data on subsequent treatment or interventions once admitted. We also acknowledge that there are other important care needs in nursing home, such as pressure ulcers or malnutrition, that we have not included in the current study. Instead, we used validated composite scores that have shown to be predictive of clinical outcomes, such as a 72-item frailty index, which incorporates many aspects of resident care needs.
Conclusion
More women than men were newly admitted to nursing home after stroke and they had higher care needs despite lower mortality. We identified pain and depression as two potentially treatable symptoms that disproportionately affect women. Residents newly admitted to nursing home following stroke survive for a substantial length of time. Improving the care and quality of life of nursing home residents with stroke is an important subject of future study.
Acknowledgments
This research was conducted with support from the Ontario Neurodegenerative Disease Research Initiative through the Ontario Brain Institute, an independent nonprofit corporation, funded partially by the Ontario government. ICES is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the Ontario Brain Institute, ICES, the Ontario MOHLTC, or CIHI is intended or should be inferred. MKK and PCA are supported by Mid-Career Investigator Awards and RHS is supported by a Clinician-Scientist Phase II Award from the Heart and Stroke Foundation of Canada and holds a grant from the Ontario Brain Institute.
Conflicts of Interest
The authors report no conflicts of interest.
Statement of Authorship
AYXY, LCM, PCA, MKK, RHS, and SEB conceived and designed the study. CD carried out the statistical analysis. AYXY and LCM drafted the manuscript. All authors contributed to the data interpretation and manuscript revision. All authors approve of the submitted manuscript.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2019.335









