A 33-year-old man with no known medical history presented to the hospital with bruising and a diffuse petechial rash. He was found to have aplastic anemia, with hospital course complicated by septic shock requiring intubation, pressors, management with broad-spectrum antibiotics and antifungals, and multiple packed red blood cell and platelet transfusions. Following extubation, he was briefly delirious, for which magnetic resonance imaging (MRI) was obtained, showing scattered areas of susceptibility artifact, compatible with microhemorrhages in the subcortical deep white matter and cerebellum, with an unusual predominance in the corpus callosum. Restricted diffusion was seen in the genu and splenium of the corpus callosum (Figure 1). The patient gradually recovered and was discharged home.
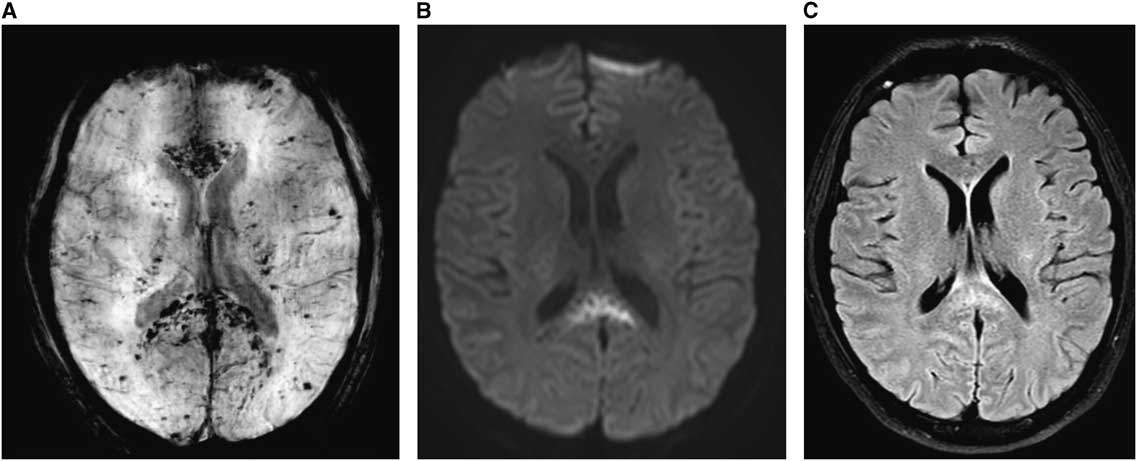
Figure 1 (A) Susceptibility-weighted images (SWI): innumerable scattered areas of susceptibility artifacts, compatible with microhemorrhages predominantly in the corpus callosum. (B) Diffusion-weighted images (DWI): splenium of the corpus callosum demonstrates restricted diffusion. (C) T2 FLAIR: hyperintensity in splenium correlating to the region of restricted diffusion.
Microhemorrhages affecting the deeper structures of the brain are not unusual in the setting of shock and thrombocytopenia due to dysregulation of cerebral blood flow and blood–brain barrier breakdown.Reference Sharshar, Annane, de la Grandmaison, Brouland, Hopkinson and Françoise 1 However, microhemorrhaging predominantly affecting the corpus callosum is a rare finding, sometimes associated with high-altitude cerebral edema (HACE).Reference Fitsiori, Nguyen, Karentzos, Delavelle and Vargas 2 Radiographic and neuropathological studies in HACE show lesions in the splenium and the genu of the corpus callosum, though not to the degree seen in our patient.Reference Kallenberg, Dehnert and Dörfler 3 Similar findings have also been reported in extracorporeal mechanical oxygenation (ECMO),Reference Shah and Armstrong 4 though in our patient it likely stemmed from severe disease burden, inflammation, and platelet dysfunction.
It is unclear why the corpus callosum is particularly susceptible to injury in these conditions. It has been postulated to result from a relative lack of adrenergic tone causing overperfusion due to hypoxic vasodilation and autonomic dysregulation.Reference Oster, Doherty, Grant, Simon and Cole 5
Statement of Authorship
Syed Shabbir was responsible for study concept and design. Elina Melamed was responsible for study concept and design. Mark Milstein was responsible for critical revision of the manuscript for intellectual content.
Disclosures
Syed Shabbir, Elina Melamed, and Mark Milstein hereby declare that they have no conflicts of interest to disclose.





