Introduction
Sudden unexpected death in epilepsy (SUDEP) is an important direct epilepsy-related cause of death in people with epilepsy. The incidence of sudden death is 20 times higher in patients with epilepsy compared to the general population. Reference Shankar, Cox, Jalihal, Brown, Hanna and McLean1 The incidence of SUDEP in adults is 1.2 (0.64–2.32) per 1000 patient-years. The incidence of SUDEP in children has been reported to vary between 0.22 and 1.17 per 1000 patient-years in various studies, with a higher incidence in children with refractory epilepsy (3.8/1000). Reference Nickels, Grossardt and Wirrell2–Reference Sveinsson, Andersson, Carlsson and Tomson5 In a recent publication on the North American SUDEP registry, 27% of the 237 patients with SUDEP were reported to be less than 16 years of age. Reference Verducci, Hussain and Donner6 The authors also noted the presence of SUDEP in 7 (3%) cases with well-controlled epilepsy. Thus, the risk of developing SUDEP is not limited to patients with frequent or uncontrolled generalized tonic–clonic seizure (GTCS). Reference Verducci, Hussain and Donner6
The exact pathophysiological mechanisms are not known, but postictal-disturbed cardiac or respiratory physiology is postulated to lead to death. Both prediction and prevention of SUDEP still remain a big challenge. Till date, the proposed SUDEP preventive strategies include effective epilepsy control (medical or surgical), evaluating and managing ictal or postictal cardiorespiratory distress, nocturnal supervision, and drugs such as selective serotonergic reuptake inhibitors, and opiate and adenosine antagonists which may help to prevent central apnea. Reference Pensel, Nass, Taubøll, Aurlien and Surges7
In a recent Cochrane review, except for low-quality evidence of preventive effect of nocturnal supervision for SUDEP, no evidence was found for the effectiveness of seizure detection devices, safety pillows, early surgical evaluation, serotonin reuptake inhibitors (SSRIs), educational programs, and opiate and adenosine antagonists in preventing SUDEP in patients with epilepsy. Reference Maguire, Jackson, Marson and Nevitt8
Conducting randomized controlled trials for evaluating modalities to prevent SUDEP is not feasible; hence, alternative surrogate endpoints such as emergency room attendance, injuries, post-seizure apnea, and heart rate variability (HRV) have been used. Reference Vilella, Lacuey and Hampson9,Reference Myers, Bello-Espinosa and Symonds10 Population-based interventions in communities with SUDEP registries may be needed to establish the role of SUDEP preventive interventions.
SUDEP counseling of adult patients and parents of children with epilepsy is recommended, Reference Galli, Vignoli, Canevini, Cerioli and Vegni11 but unless preventive strategies are explained, such counseling may lead to panic and anxiety among caregivers and patients. The present review intends to provide an insight into the potential ways of SUDEP prevention.
Identifying Patients at Risk
The MORTEMUS study highlighted the role of centrally mediated postictal respiratory and cardiac compromise as a key mechanism leading to SUDEP. Reference Ryvlin, Nashef and Lhatoo12 Intrinsic brain mechanisms leading to or associated with seizure termination have been postulated to lead to a centrally mediated neurovegetative breakdown and postictal generalized electroencephalogram (EEG) suppression. Reference Pensel, Nass, Taubøll, Aurlien and Surges7,Reference Ryvlin, Nashef and Lhatoo12 Animal studies have implicated postictal dysfunction of brainstem structures which control autonomic functions, which can lead to sudden cardiorespiratory arrest in SUDEP. Reference Mueller, Nei and Bateman13–Reference Holt, Arehart, Hunanyan, Fainberg and Mikati15
The first crucial step toward SUDEP prevention is to correctly identify the subgroup of people with epilepsy who are at high risk for developing SUDEP. This can be done by evaluating the patient using safety checklists, inventories such as SUDEP-7 inventory, and genetic testing, and by studying specific EEG changes which have been associated with SUDEP. Reference Pensel, Nass, Taubøll, Aurlien and Surges7,Reference Walczak, Leppik and D’Amelio16,Reference Sun, Perera, Henley, Ashby and Shankar17
Checklist and Inventory
Past studies have highlighted the possible role of 17 factors associated with increased risk of SUDEP, some of which are potentially modifiable. These form the background of the seizure and SUDEP safety checklist. This is a 10-minute risk assessment tool which can be used in daily practice in epilepsy clinics for screening patients who are at high risk of developing SUDEP. These checklists are also available on mobile applications. Reference Shankar, Newman, McLean, Anderson and Obe18–20 However, no critical analysis of checklists and inventories is available till date.
These factors include sleeping in prone position, unclear treatment history, primary generalized epilepsy, increasing seizure frequency, compliance issues, alcohol problem, subtherapeutic antiepileptic drug (AED) levels, lack of night surveillance, duration >15 years, early-onset epilepsy, frequent AED changes, use of anxiolytic medication, intellectual disability (ID), male gender, patients on antidepressants and on carbamazepine, and increasing seizure severity. Reference Shankar, Newman, McLean, Anderson and Obe18–20
Of the 17 risk factors, 7 are potentially modifiable. These are unclear treatment history, poor adherence to medication, subtherapeutic medication levels, alcohol misuse, no night surveillance, sleeping in the prone position, and increasing seizure frequency (p < 0.001). Non-modifiable risk factors included duration of epilepsy and the presence of GTCSs. Reference Shankar, Walker and McLean21
In a study on the association between SUDEP-7 inventory and HRV, the SUDEP-7 score was found to be inversely and significantly associated with HRV. The results suggest that older age, longer duration of epilepsy, and the presence of ID may increase the risk of SUDEP through their direct influence on decreasing the vagus nerve-mediated HRV. Reference Novak, Miller, Markovic, Meymandi and DeGiorgio22,Reference DeGiorgio, Miller and Meymandi23
Genetic Factors
Understanding the genetic basis for SUDEP is important in identifying patients and family members at risk. In a recent study, an exome-based analysis of cardiac arrhythmia, respiratory control, and epilepsy genes was performed in 61 patients with SUDEP. Reference Bagnall, Crompton and Petrovski24 De novo mutations were identified in 28/61 cases (46%). Four patients (7%) had mutations in common genes responsible for long QT syndrome, 9 (15%) had candidate pathogenic variants in dominant cardiac arrhythmia genes, and 15 (25%) had mutations or candidate pathogenic variants in dominant epilepsy genes. No gene reached genome-wide significance with rare variant collapsing analysis. DEPDC5 (p = 0.00015) and KCNH2 (p = 0.0037) were among the top 30 genes identified. Reference Bagnall, Crompton and Petrovski24
EEG Markers
Postictal generalized EEG suppression (PGES) is the term used for diffuse EEG “flattening” after seizure cessation. It is defined as postictal unilateral or bilateral EEG suppression of >1-second duration occurring immediately or within 30 seconds of seizure cessation with an amplitude of <10 mV. Reference Lhatoo, Faulkner, Dembny, Trippick, Johnson and Bird25 PGES is usually seen after GTCS. In a retrospective study of 48 epilepsy cases, 27% (13) of those who had GTCS had PGES followed by postictal slowing. Reference Seyal, Bateman and Li26 The reported occurrence of PGES after convulsive seizures is 40%–60% in patients with generalized convulsive seizures as compared to 1%–2% in cases with focal seizures. Reference Lhatoo, Faulkner, Dembny, Trippick, Johnson and Bird25,Reference Urges, Strzelczyk, Scott, Walker and Sander27
In some SUDEP patients, EEG recordings after terminal seizures had demonstrated PGES. Reference Donner, Camfield, Brooks, Buchhalter, Camfield and Loddenkemper3,Reference Pensel, Nass, Taubøll, Aurlien and Surges7 These findings have initiated the debate over its potential role as a predictor of future SUDEP risk and also in the pathophysiology of SUDEP, wherein the initiating event is considered as “electrocerebral shutdown.”
Longer duration (> 50 seconds) PGES are associated with increased risk of SUDEP. Reference Novak, Miller, Markovic, Meymandi and DeGiorgio22,Reference Urges, Strzelczyk, Scott, Walker and Sander27 Children with PGES had higher SUDEP-7 scores than children without PGES. Reference Lhatoo, Faulkner, Dembny, Trippick, Johnson and Bird25 Increased risk of PGES in children has been noted in sleep, with shorter duration of clonic phase, symmetric tonic extension posturing, and terminal burst suppression after seizure. Reference Donner, Camfield, Brooks, Buchhalter, Camfield and Loddenkemper3
Effective Epilepsy Treatment
An important measure for SUDEP prevention is effective epilepsy treatment and seizure control. Reference Pensel, Nass, Taubøll, Aurlien and Surges7 This can be achieved using appropriate AED, timely presurgical referral in drug refractory cases, and surgery in candidates meeting the surgical criteria.
A meta-analysis (2011) of adult patients with refractory epilepsy reported that patients receiving an add-on AED had a sevenfold lower risk of SUDEP (0.9/1000 vs. 6.9/1000 patient-years) as compared to patients receiving an add-on placebo. Reference Ryvlin, Cucherat and Rheims28
Another important step is patient education regarding drug compliance and adherence, lifestyle modification to avoid seizure-triggering factors such as sleep deprivation, stress, and excess alcohol intake, and educating them about care plans for seizure clusters (rescue medicine) and home management of seizures. Appropriate advice regarding AED use during gastrointestinal illness, intercurrent illness, concomitant use of other drugs, use of oral contraceptive pills, and pregnancy should be given.
Surgical removal of epileptogenic zone is effective seizure control treatment, but its role in SUDEP prevention is debatable. Studies have reported that failed surgical candidates have higher risk of SUDEP. Reference Salanova, Markand and Worth29–Reference Sperling, Harris, Nei, Liporace and O’Connor31 But there is no strong evidence to support this. It is likely that patients failing temporal lobe surgery may have their epileptogenic zone involving extratemporal brain regions which control cardiorespiratory functions, leading to increased risk of SUDEP post-surgery. Reference Ryvlin32–Reference Ryvlin, Montavont and Kahane34 Hence, delineation of the epileptogenic zone and appropriate surgical management is of paramount importance..
Detect Seizures and Cardiorespiratory Distress
As SUDEP is known to follow a seizure, seizure detection and effective termination may help to prevent the postictal cardiorespiratory compromise and thus prevent SUDEP. This can be achieved by the following measures:
Nocturnal Supervision
Past studies have highlighted the role of nocturnal supervision for detecting seizures and reported it to be protective. Reference Pensel, Nass, Taubøll, Aurlien and Surges7,Reference Langan, Nashef and Sander35,Reference Nashef, Fish, Garner, Sander and Shorvon36 Combined use of nocturnal supervision with seizure detection devices may enable more effective seizure detection, but evidence to prevent SUDEP is lacking.
Disadvantages of nocturnal supervision include high false-positive or negative detection rates, effect on quality of life issues, and cultural acceptance. In addition, one must also be aware of the fact that the intervention by a witness does not necessarily preclude the occurrence of SUDEP. Though turning the patient from prone to recovery position after GTCS may reverse respiratory compromise, more effective resuscitation may be needed.
Seizure Detection Devices
A variety of seizure detection devices are currently available. Though these may be effective in detecting seizures, some are marketed as being helpful to prevent SUDEP though the evidence for the same is lacking. Use of these devices should be individualized according to patient preference, seizure profile (nocturnal, generalized, and frequency), and overall risk of SUDEP. More extensive clinical investigation and trials are needed to find out their appropriate role in the SUDEP prevention algorithm. Reference Pensel, Nass, Taubøll, Aurlien and Surges7
Prone Position and SUDEP
SUDEP cases are more often found prone, but extrapolating this observation to sleeping prone as a contributing factor has no supportive evidence. A recent systematic review and meta-analysis of 253 cases of SUDEP reported that approximately 73.3% of patients were found in prone position (95% confidence interval [CI] 5 65.7%, 80.9%, p < 0.001). Prone position was observed in 85.7% (95% CI 5 74.6%, 93.3%) of patients aged < 40 years of age (95% CI 5 74.6%, 93.3%). The likely possible mechanism suggested is that turning to prone position during GTCS followed by postictal apnea (commonly associated with PGES) leads to obstructive apnea. In addition, prone position is associated with impaired arousal. Reference Liebenthal, Wu, Rose, Ebersole and Tao37 However, as the prone positioning occurs during the seizure, a “back-to-sleep campaign,” such as that for SIDS prevention, may not be very helpful. Most experts believe that individuals with epilepsy turn in their sleep or turn with a GTCS making the bedtime sleep position irrelevant.
For SUDEP prevention, if the seizure is witnessed, turning patient from prone to lateral recovery position and stimulating the patient may help.
Prevent Airway Obstruction
Safety Pillows
Latex safety pillows (ventilated foam pillows) may reduce the contribution of prone position toward postictal cardiorespiratory distress and prevent obstructive apnea. Reference Pensel, Nass, Taubøll, Aurlien and Surges7,Reference Devinsky38 However, no studies are available to support their role in SUDEP prevention.
Reduce Central Hypoventilation
Serotonergic Drugs – SSRI
Lower brainstem serotoninergic nuclei play an important role in the regulation of respiration. Serotonin neurons in the brainstem sense rising carbon dioxide and low pH, thereby stimulating breathing and arousal. Reference Richter, Manzke, Wilken and Ponimaskin39 Abnormalities of serotonergic neurons have been previously reported in SIDS and in a mouse model of SUDEP, thereby highlighting possible role of selective serotonin receptor inhibitors (SSRIs) for SUDEP prevention. Reference Pensel, Nass, Taubøll, Aurlien and Surges7,Reference Uteshev, Tupal, Mhaskar and Faingold40–Reference Faingold, Tupal and Randall42 Use of SSRIs may decrease the risk of potential apnea.
In animal studies, fluoxetine has been shown to prevent the occurrence of fatal seizure-induced apnea in SUDEP. Reference Faingold, Randall, Mhaskar and Uteshev41–Reference Faingold, Randall, Zeng, Peng, Long and Feng44 . In a retrospective study, it was seen that postictal hypoxemia was significantly less frequent in patients with drug refractory partial epilepsy receiving SSRIs as compared to those who were not on SSRIs. Reference Batemal, Li, Lin and Seyal45
Two double-blind, randomized, placebo-controlled trials (NCT02569970, NCT02929667) are underway (results awaited) to assess the efficacy of Fluoxetine against seizure-induced central apnea.
Reduce Adenosine and Endogenous Opioid-Induced Brainstem Depression
Inhibitors of Opiate and Adenosine Receptors
Seizure activity induces massive release of endogenous opioids and adenosine which helps in seizure termination. But their excessive release can lead to postictal apnea. The opioid antagonist naloxone may potentially reduce the occurrence of postictal apnea. A randomized control trial, ENALEPSY (NCT02332447) study, on postictal naloxone is presently underway (recruitment completed and results awaited) to assess the efficacy of naloxone in reducing the severity of the postictal central respiratory dysfunction after GTCS.
Animal studies have reported that treatment with caffeine may directly prevent apnea and cardiopulmonary suppression by blocking A1Rs as well as A2ARs in brainstem, thus preventing SUDEP. Reference Faingold, Randall, Mhaskar and Uteshev41 A recent study has shown improved survival in mice model from 23.75 ± 1.35 minutes to 54.86 ± 6.59 minutes (p < 0.01) when caffeine is given 5 minutes after the seizure onset. Reference Shen, Li and Boison46 However, caffeine has proconvulsant effect and can aggravate the duration, frequency, or severity of seizures and is not recommended. Reference Shapira, Zohar, Newman, Drexler and Belmaker47
Cardiac and Diaphragmatic Pacing
Cardiac and diaphragmatic pacing are potential SUDEP prevention modalities which need to be explored. Standard cardiac pacing prevents brain hypoperfusion but may not reverse respiratory failure which might require diaphragmatic pacing or phrenic nerve stimulation.
Preventing SUDEP in the Epilepsy Monitoring Unit (EMU)
SUDEP and near-SUDEP have been reported from EMUs. Reference Ryvlin, Nashef and Lhatoo12,Reference Sanchez-Larsen, Fernandez-Perez, Principe, Ley and Rocamora48 Special attention should be given to all patients admitted to the EMU for elective VEEG monitoring. Apart from providing basic care, systematic monitoring for ictal/postictal cardiorespiratory compromise is a crucial part of their management.
Systematic monitoring using electrocardiography and SpO2 devices with appropriate alarms should be done. EMU should have organization of emergency codes. The staff should be trained to quickly identify ictal/postictal cardiorespiratory distress and start resuscitation whenever needed. Animal studies have highlighted the role of postictal oxygen therapy for SUDEP prevention. Reference Venit, Shepard and Seyfried49 Oxygen should be started in patients with postictal respiratory distress or decreased oxygen saturation. Precautions should be taken, while tapering the AEDs as rapid withdrawal may induce seizures. Many patients undergoing epilepsy surgery workup have their AED tapered while admitted to the EMU. In a recent study of 25 patients with SUDEP (11 monitored, 5 non-monitored, and 9 near-SUDEP), in 9 (36%) patients AEDs were reduced by more than 50% and in 5 (20%) patients AEDs were completely withdrawn. This suggests a possible role of rapid withdrawal in promoting the terminal seizure and associated cardiorespiratory arrest. Reference Holt, Arehart, Hunanyan, Fainberg and Mikati15
Conclusion
SUDEP remains a significant cause of epilepsy-associated mortality in adult and children patient population and its prevention remains a big challenge. Identifying patients at risk, attaining good seizure control using appropriate AED and early surgical referral along with training caregivers in home management of seizures, and detecting seizures and cardiorespiratory arrest are potential ways of reducing SUDEP-related mortality (Figure 1).
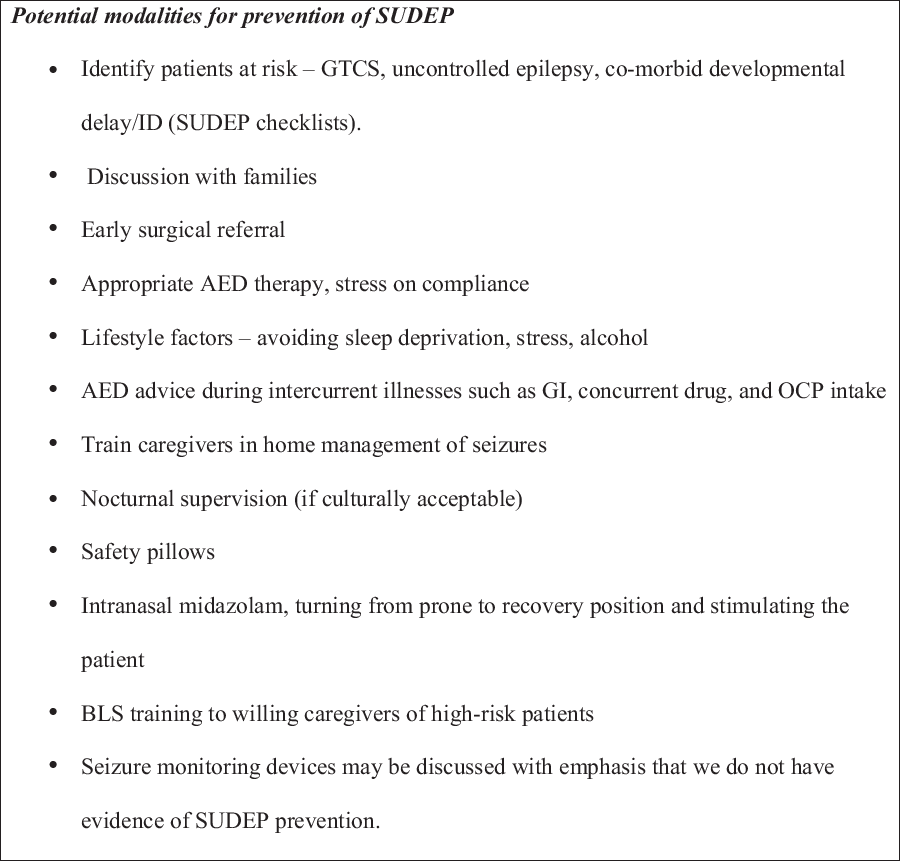
Figure 1: Potential Modalities for Prevention of SUDEP.
Advent of seizure detection devices, safety pillows, drugs reducing adenosine and endogenous opioid-induced brainstem depression, and cardiac and phrenic pacing have paved the way for future prevention modalities, but more studies are needed to establish their effectiveness.
Conflict of Interests
None.





