It took 85 % of the time life has existed on earth for animals to emerge onto dry land, and that occurred only when they could take with them the 0·9 % salty water that mimicked the primordial sea they relinquished(1–Reference Rossier, Baker and Studer3). Hence, for terrestrial animals, Na, the part constituent of common salt, is an indispensable, irreplaceable, life-supporting cation. In many animals, the means for acquiring and retaining it have evolved, respectively, Na appetite and kidneys. Indeed, Na demarcates the two forms of life by its motility, essential for animals but absent in plants.
For humans, salt may have initiated trade and urbanisation surrounding salt mines (European). Salt also serves religion and ceremony, and into the 20th century, its use for conserving food prevented starvation in both cold and hot climates(Reference Kurlansky4–Reference Multhauf6).
Today, worldwide, salt is consumed daily, repeatedly, totalling an amount that is in excess of that required to preserve life, which many hold to increase society’s disease burden, vascular and cancerous, significantly and cause three million deaths annually(7). Obesity is estimated to cause four million deaths(8), but a million of those may be due to salt intake(Reference Ma, He and MacGregor9–Reference Zhou, Stamler and Chan11), so that while the two may be similarly deadly, the causes of obesity are researched incomparably more(12,Reference Shaldon and Vienken13) . The reason for this is not clear, but it may be that obesity is prominently visible, whereas salt is allied to a silent killer, hypertension(Reference Shaldon and Vienken13).
The sole methods proposed to regulate salt intake are based on meagre evidence and their efficacy is dubious. It stands to reason that, if we knew the causes of salt intake, we could regulate it better(Reference Burgermaster, Rudel and Seres14). The purpose of this brief review is to highlight the need for research into the determinants of salt intake by summarising the little we know.
Critique of causes of salt intake and intervention
The determinants of our excessive salt appetite have been scarcely researched and, consequently, are scarcely understood(Reference Burgermaster, Rudel and Seres14–Reference Newson, Elmadfa and Biro18). Research has been primarily into the consequences of salt intake, primarily comprising large-scale studies, which have engendered the consensus that salt is toxic, along with a nuanced contention that it is less so(7,Reference Ma, He and MacGregor9–Reference Zhou, Stamler and Chan11,Reference Newson, Elmadfa and Biro18–Reference Trinquart, Johns and Galea27) .
The extant hypotheses about the causes of excess salt intake are that mere exposure to salt early in life, together with Na infiltrated without our knowledge into our bodies via heavily salted processed food, determines our lifelong intake(Reference He and MacGregor20,Reference Hyseni, Elliot-Green and Lloyd-Williams23,Reference Mozaffarian, Fahimi and Singh26,Reference Mancia, Oparil and Whelton28,Reference Henney, Taylor and Boon29) . Yet, shoppers and diners may choose comparatively heavily salted food because salt enhances the flavours, rather than for its taste per se (Reference Henney, Taylor and Boon29,Reference Liem and Russell30) , and salt intake is similar or greater where food is less industrialised(7,Reference McCarron24) . Similarly, the evidence for early exposure as a determinant of later salt intake is poor, and many animal experiments have failed to confirm it(Reference Beauchamp15,Reference Leshem16,Reference Macchione, Caeiro and Godino31,Reference Mecawi, Macchione and Nuñez32) . The opposite is better evidenced: early Na restriction increases lifelong intake(Reference Macchione, Caeiro and Godino31–Reference Goldstein and Leshem39). Moreover, growing children and adolescents ingest and prefer more salt than they were ever previously exposed to(Reference Leshem16,Reference Goldstein and Leshem39,Reference Quader, Gillespie and Sliwa40) (Fig. 1). Hence, both extant hypotheses are meagre and unproven suppositions for a phenomenon as potent, pervasive and persistent as similar ingestion of salt across people with widely differing diets(7,Reference McCarron24,Reference Powles, Fahimi and Micha41) .

Fig. 1. Salt preference in teens (r 0·64, P < 0·02). From Leshem(Reference Leshem16).
Nevertheless, these hypotheses engender the prime methods advocated to regulate salt intake, advisory, admonitory and supervisory(Reference Hyseni, Elliot-Green and Lloyd-Williams23). They are adopted widely, but selected instances have attained extraordinarily diverse results as measured over years (from an increase of 0·5 to a decrease of 4·8 g/d salt per individual(Reference Hyseni, Elliot-Green and Lloyd-Williams23)). However, long-term intervention studies and metanalyses included no comparison groups, provided no data on prior trends and rarely reported concomitant dietary and BMI changes which may determine Na intake. Moreover, they were confounded by sex, regional, and socio-economic differences, epochs of increases during intervention, different samples before and after intervention and changes in energy intake and diet(Reference Hyseni, Elliot-Green and Lloyd-Williams23,Reference Powles, Fahimi and Micha41–Reference O’Flaherty, Buchan and Capewell46) . Therefore, it is moot whether reduction is intervention-related any more than the parallel decrease in total energy intake, to which Na intake is inextricably linked(45,Reference O’Flaherty, Buchan and Capewell46) . Further, failures and contradictory data for the same countries in line with global increases or stability have also been reported(Reference Burgermaster, Rudel and Seres14,Reference Newson, Elmadfa and Biro18–Reference Mancia, Oparil and Whelton28,42,Reference Bernstein and Willett47–51) .
Excess salt intake has been related to many severe diseases, and yet it is uncertain how its use can be limited because too little salt may also contribute to ill health. People and communities differ so much that epidemiological studies, the mainstay of the Na–disease correlation, may swamp diversity, which may range from strong positive relationships to none or inverse relationships, even within the same study(Reference Graudal, Hubeck-Graudal and Jürgens19,Reference Messerli, Hofstetter and Bangalore25–Reference Trinquart, Johns and Galea27,Reference Powles, Fahimi and Micha41,42,52–Reference Kong, Baqar and Jerums54) . A J-shaped curve has been proposed to account best for the data(Reference Graudal, Hubeck-Graudal and Jürgens19).
Wide acceptance of the infiltration and early exposure doctrines may divert us from efforts to understand the causes of high salt intake.
Salt appetite and need
Salt appetite in animals, that is, its determinants and mechanisms, has been well studied. Studies have revealed that bodily Na deficit rapidly transforms the perception of the taste of even concentrated salt from repulsive to desirable. The transformation is mediated by extensive brain circuits, neurohormones and hormones(Reference Morris, Na and Johnson2,Reference Na, Morris and Johnson55–Reference Robinson and Berridge57) . Consistent with the benefit suggestion, salt consumption to alleviate a deficit frequently engenders a lifelong enhancement of salt appetite. It has been proposed that this is adaptive, prioritising salt by increasing its hedonic attraction, and hence salience, and storing Na sources in memory, all as increased protection to prevent hyponatraemic challenge, which has now become a proven hazard. The hazards have been suggested to be ecological (Na-scarce environments), constitutional or pathological (tendencies for, and individual causes of, dehydration and hyponatraemia)(Reference Leshem, Kavushansky and Devys58–Reference Montain, Sawka and Wenger68).
While these physiological systems exist in humans too, the behaviour differs markedly. The remedial hedonic transformation is vestigial at best in humans and poorly evidenced. In fact, no reliable study of salt-deficient humans wanting salt spontaneously exists, and the studies that have been conducted failed to demonstrate it convincingly(Reference Beauchamp, Bertino and Burke69–Reference Wilkins and Richter74), but see Leshem et al. (Reference Leshem, Abutbul and Eilon75) and Wald & Leshem(Reference Wald and Leshem76). Indeed, in contradiction to studies in animals, even neonates(Reference Leshem59,Reference Wolf and Pfaffman77) , studies in humans have found that they do not crave, seek or ingest salt when in need and can die from its lack in the body with salt at hand(Reference Moritz and Ayus78).
In contrast to animals, whose salt consumption can be remedial, which is absent in humans, humans take pleasure from consuming salt with almost every food and meal. Daily it pleases all the inhabitants of the planet. Salt is invariably taken with food, which it enhances in many ways, increasing saltiness, suppressing bitterness, promoting taste where it is understated and imbuing it where absent, modifying texture and preserving, frequently when its own taste is covert(Reference Beauchamp15–Reference Mattes17,Reference Hayes, Sullivan and Duffy56,Reference Breslin and Beauchamp79,Reference Lucas, Riddell and Liem80) . Although this is consistent with the infiltration hypothesis as a cause of high salt intake, before acceding to it, recall the issue: why has our sense of taste evolved to respond in this way? It seems to be no coincidence because while the infinite variety of tastes and flavours is served by four taste receptors on the tongue, reinforced by olfaction, there is one more, unique among taste receptors in that it is dedicated solely to one ion – Na, the salt taste receptor (to which olfaction cannot contribute). There may even be one or two more, less specific, backup receptors(Reference Kure, Joseph and Feldman81,Reference Smith, Treesukosol and Paedae82) . No other nutrient, taste molecule or ion is awarded such specificity in humans or animals. These receptors, in addition to the taste of salt, also mediate some of its effects on other tastes via peripheral (oral) or brain-mediated neural activity(Reference Kure, Joseph and Feldman81,Reference Sandhu, Fernando and Irvine83) . Indeed, Na deficiency can impair other taste sensations(Reference McCance71).
Thus, human salt appetite does not appear to be remedial as it is in animals, but it may be beneficial in other ways that enhance its taste to promote its intake.
Acquisition of salt appetite
As already mentioned, it is generally believed that early exposure to salt in food determines lifelong intake, but the evidence is poor, and therefore, I shall detail what we do know.
The precocious rat pup brain has the salt appetite already at birth. By 12 d of age, the pup will lick salt if it requires it and, by weaning, it develops the ability to pinpoint Na among cations, possibly paralleling the process in the human fetus(Reference Leshem59).
Many preterm (about 10 % of babies) and some full-term babies are at risk of hyponatraemia and receive Na supplementation to ensure proper growth and neurological and cognitive development(Reference Macchione, Caeiro and Godino31,Reference Al-Dahhan, Jannoun and Haycock84–Reference Chan, Chua and Teo87) . The severity of the obligatory neonatal dehydration and Na loss predicts the Na content of the diet we will compose in childhood and possibly beyond(Reference Leshem36–Reference Stein, Cowart and Epstein38,Reference Leshem, Maroun and Weintraub88) (Fig. 2).

Fig. 2. Correlations of neonatal serum and dietary sodium in children by (a) ethnicity and (b) sex. Black symbols and continuous lines, Arabs and boys, respectively; white symbols and dashes, Jews and girls, respectively. Correlations: Arabs, r 0·333 (NS, but without outlier, r 0·470*); Jews, r 0·520*; boys, r 0·549*; girls, r 0·400*. * P > 0·05. Data from forty-one children aged 10·5 (sem 0·2) years. From Shirazki et al.(Reference Shirazki, Weintraub and Reich37), with permission.
Only some babies have a liking for salt(Reference Crystal and Bernstein34), in part dependent on birth weight, blood pressure(Reference Shirazki, Weintraub and Reich37,Reference Liem89–Reference Stein, Cowart and Beauchamp91) and the severity of their mother’s morning sickness(Reference Crystal and Bernstein33–Reference Leshem36). The severity of the mother’s morning sickness also has a long-term effect, increasing salt appetite in her offspring in their infancy, adolescence and adulthood(Reference Crystal and Bernstein33–Reference Leshem36). Then, in infancy, childhood vomiting and diarrhoea contribute further to the perinatal influences increasing later salt appetite(Reference Kochli, Tenenbaum-Rakover and Leshem35–Reference Shirazki, Weintraub and Reich37,Reference Leshem, Maroun and Weintraub88) (Fig. 3). It is assumed that vomiting, whether maternal during pregnancy or in the child, and diarrhoea cause Na loss, thereby engaging the protective enhancement mentioned above.

Fig. 3. Relation of history of mineralofluid loss (maternal vomiting during pregnancy, infantile vomiting and diarrhoea) and avidity (sum of all test measures) for the taste of salt or sugar (the mean values with their standard errors for salt are higher than for sweet because they include scores for salting of food and dietary NaCl). 0 = no history of mineralofluid loss, 3 = highest incidence of mineralofluid loss. ** P > 0·01, different from 0. * P < 0·01, different from 3. The data are from fifty (8, 15, 18, 9 by mineralofluid loss score) girls and boys aged 14 (sem 2) years, and their mothers. From Leshem(Reference Leshem36) with permission. ![]() , NaCl;
, NaCl; ![]() , sugar.
, sugar.
As it develops, the human child increasingly has a predilection for salt, marginally related to early dietary experience(Reference Mecawi, Macchione and Nuñez32,Reference Sullivan and Birch92,Reference Stein, Cowart and Beauchamp93) , but significantly related to neonatal hyponatraemia and to growth(Reference Leshem16,Reference Macchione, Caeiro and Godino31,Reference Mecawi, Macchione and Nuñez32,Reference Leshem36–Reference Quader, Gillespie and Sliwa40,Reference Leshem, Maroun and Weintraub88,Reference Liem89) . It is important to note that this increase in later salt appetite occurs with no experience of salt taste, a phenomenon established in rats(Reference Morris, Na and Johnson2,Reference Leshem, Kavushansky and Devys58,Reference Sakai, Fine and Epstein65,Reference Sakai, Frankman and Fine66,Reference Leshem, Langberg and Epstein94) ; in babies, the neonatal Na supplementation is administered intravenously which may not condition a salt preference(Reference Tordoff and Coldwell95). In fact, it may be that the consequent increase in dietary Na of such children (aged 10–15 years) is unaccompanied by a preference for the taste of salt per se (Reference Shirazki, Weintraub and Reich37) (but see Liem(Reference Liem89)), a known dissociation(Reference Lucas, Riddell and Liem80,Reference Liem89,Reference Drewnowski, Henderson and Driscoll96) . Finally, in the adolescent growth spurt, Na intake outstrips the intake of energy content, other macronutrients and electrolytes, together suggesting a unique developmental or maturational requirement(Reference Goldstein and Leshem39,Reference Quader, Gillespie and Sliwa40,Reference Al-Dahhan, Jannoun and Haycock84–Reference Bischoff, Tomlinson and Belik86,Reference Ayisi, Mbiti and Musoke97,Reference Bobowski and Mennella98) .
These observations, particularly that children’s salt intake is greater than adults’ salt intake, and boys’ salt intake greater than girls’ salt intake(Reference Goldstein and Leshem39), contradict the pervasive notion that ‘mere exposure’ to dietary salt, specifically early exposure, determines the subsequent attraction for salt and its intake. ‘Mere exposure’ is difficult to confirm in humans, but many studies in which rats were exposed to high dietary salt from gestation to adolescence have generally failed to reveal a systematic, Na-specific, relationship to long-term salt preference(Reference Leshem16,Reference Liem89) .
Thus, in humans, its enhancement by early Na loss, restriction or deficiency is the most substantiated determinant of long-term salt appetite. The extent of the salt intake that is thus determined remains to be investigated, but morning sickness may affect 33 % of pregnancies(Reference Crystal and Bernstein33,Reference Chortatos, Haugen and Iversen99) and in a small study, increased salt intake in 50 % of adolescents was due to putative perinatal Na losses, a phenomenon consistent with other early metabolic programming(Reference Macchione, Caeiro and Godino31,Reference Mecawi, Macchione and Nuñez32,Reference Leshem36,Reference Alwasel, Barker and Ashton85) (Figs. 2 and 3). Together, these could suggest a significant contribution to high salt intake in the population.
Adult salt intake
However, in adults, Na loss, restriction or deficiency no longer enhances salt appetite(Reference Leshem100).
Adult salt intake is lower and settles into different patterns for men and women. Men take more salt per kg of body weight than women by about 20 %, possibly because men sweat more and have a greater lean mass(Reference Leshem16,Reference Wald and Leshem76) . Men’s higher intake also possibly protects them from depression because low dietary Na can contribute to depression, and women suffer more from depression(Reference Goldstein and Leshem39,Reference Shimizu, Kadota and Koyamatsu101) (Fig. 4). In rats, low Na also indicates depression, and antidepressant treatment may reduce salt intake(Reference De Gobbi, Omoto and Siqueira102,Reference Leshem103) . The relationship of salt intake and mood is examined briefly below.
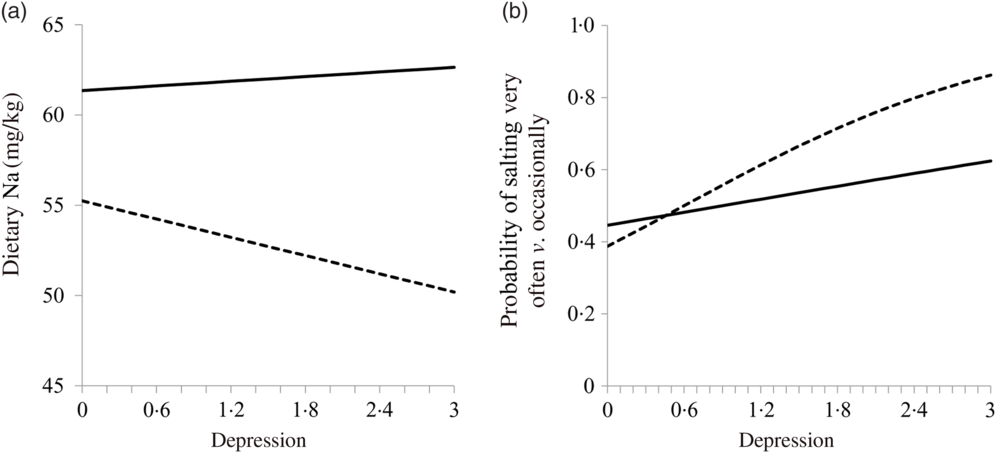
Fig. 4. Relationship of weight-adjusted dietary sodium (a) and adding salt (b) to depression. Men, line; women, dashes. Both variables are adjusted for dietary energy. The relationships are significant for women. From Goldstein & Leshem(Reference Goldstein and Leshem39).
Salt and the elderly
Unlike other pleasures, sensations and tastes, such as thirst and hydration that wane with age, the taste for salt probably does not. Older people continue to relish their salt, and it may therefore be useful in maintaining their nourishment in age-related anorexia and hyponatraemia(Reference Goldstein and Leshem39,Reference Hendi and Leshem104–Reference Zallen, Hooks and O’Brien106) . Older people are frequently hypertensive and hence routinely recommended to restrict Na intake, although some researchers have suggested the opposite advice might be given(Reference Mahtani, Heneghan and Onakpoya22,Reference Mente, O’Donnell and Rangarajan53) . Cognitive impairment related to salt intake in the elderly has been studied, but the results are currently indeterminate(Reference Renneboog, Musch and Vandemergel105–Reference Nowak, Fried and Jovanovich109).
Sodium deficiency
Dietary Na deficiency is rare, occurring in extreme cases of eating or drinking disorders(Reference Bhattarai, Kafle and Panda110). Hyponatraemia, especially frequent among the institutionalised, hospitalised and the elderly, is associated with multiple pathologies, including of mood, and with mortality, and it is due to multiple fluid and electrolyte disorders(Reference Hao, Li and Zhang111,Reference Mohan, Gu and Parikh112) . Hyponatraemia is also frequent in physical exertion, due to Na loss in sweat or overhydration that leaches Na, particularly among less trained athletes. Nevertheless, athletes can be in mortal danger of hyponatraemic crisis because its diagnosis requires astute health workers(Reference Moritz and Ayus78,Reference Hao, Li and Zhang111,Reference Mohan, Gu and Parikh112) . These counsellors are necessary because unlike animals, humans seek salt to please their palate, but not to save their life(Reference Moritz and Ayus78). Hence, many sports authorities recommend Na supplementation for safety, as well as to maintain athletic performance and accelerate recovery after it(Reference Moritz and Ayus78,Reference Del Coso, González-Millán and Salinero113–Reference Hew-Butler, Loi and Pani115) . Such effects could condition a salt preference and contribute to its intake(Reference Wald and Leshem76).
Substantive findings suggest that low dietary Na contributes to CVD, whether in general or only in vulnerable individuals, as in the case of high Na intake, is not however known(Reference Graudal, Hubeck-Graudal and Jürgens19,Reference Mahtani, Heneghan and Onakpoya22,Reference Messerli, Hofstetter and Bangalore25,Reference Trinquart, Johns and Galea27,Reference Mente, O’Donnell and Rangarajan53,Reference Kong, Baqar and Jerums54) . If Na intake alleviates the discomfort caused by these diseases, its taste may become preferred, and thus, its intake may be increased.
Are there benefits supporting excess salt intake?
Na intake is essential to all bodily functions and to all organs, tissues, and cells, their membranes and contents, but current physiological knowledge indicates that a pinch a day suffices (about 1·3 g salt or 500 mg Na+), our intake far exceeds this amount. Evolutionary rationale suggests that prominent characteristics, such as perceiving the taste of salt as delectable, are readily explainable as adaptations, but it is not known how our excess salt intake may be beneficial(Reference Beauchamp15–Reference Mattes17,Reference Goldstein and Leshem39) . Might there be benefits yet to be discovered driving this excessive intake(Reference Goldstein and Leshem39,Reference Benton, Cousins and Young116) ?
Benefits would tend to promote the inheritance of an increased salt appetite, whereas ailments such as hypertension, stroke and cancer would not tend to restrain it because evolutionary rationale biases for the inheritance of properties that are effective prior to reproductive age (the benefits), rather than after it (the ailments). Further, some of the maladaptive effects of Na may be adaptive in other circumstances(Reference Fessler62,Reference Benton, Cousins and Young116–Reference Leshem, Saadi and Alem118) . Nevertheless, currently there is little evidence that salt appetite is inherited(Reference Keskitalo, Tuorila and Spector119–Reference Wise, Hansen and Reed121).
Another suggested determinant is addiction. This implies that all 7·6 billion of humans are addicted to salt, despite the obvious fact that pure crystalline salt is not craved, ingested, injected or inhaled, even by people in putative withdrawal on a low-Na diet. This also dissociates animal studies that proposed that brain Na appetite substrates also serve other addictions(Reference Morris, Na and Johnson2,Reference Liedtke, McKinley and Walker122) . Moreover, an addiction that is a norm might be a contradiction in terms, and dealing with it is rather daunting, considering our failure with other addictions, all of them together comparatively imperceptible(Reference Cocores and Gold123,Reference Tekol124) .
Conditioning salt preference through exertion, mood, health and disease
Many physiological changes, modifying salt appetite or modified by it, may have little to do with maintaining Na homoeostasis. On the other hand, they may condition subsequent Na intake, if when Na is lost, salt intake alleviates some discomfort. This may underlie the increased acceptability of isotonic drinks in athletes and exercisers and in patients with Na-wasting diseases who discover salt to be prophylactic, and for the relief of hyponatraemia(Reference Kochli, Tenenbaum-Rakover and Leshem35,Reference Montain, Sawka and Wenger68,Reference Wald and Leshem76,Reference Yeomans, Blundell and Leshem125) .
In animal studies, salt was found to mitigate stress and facilitate social behaviour, which are useful effects, while low Na and its related hormones were found to indicate depression(Reference Morris, Na and Johnson2,Reference Na, Morris and Johnson55,Reference De Gobbi, Omoto and Siqueira102,Reference Leshem103,Reference Krause, de Kloet and Flak126) . The human data are less consistent. Hostile male medical students seem to prefer salt(Reference Miller, Friese and Dolgoy127), and low dietary Na contributes to depression in Japanese men and marginally in American women, who may self-medicate with salt to improve their mood(Reference Goldstein and Leshem39,Reference Shimizu, Kadota and Koyamatsu101) . Other research has failed to relate the two or indicated cultural and dietary dependence, and yet other studies suggested salt may increase anxiety and even panic(Reference Miller, Friese and Dolgoy127–Reference Foo and Mason132).
Before or after exertion, many athletes drink Na-containing fluids and some swallow salt pills, and salt can aid recovery after exertion and condition a preference(Reference Wald and Leshem76,Reference Del Coso, González-Millán and Salinero113–Reference Hew-Butler, Loi and Pani115) . However, it is not known whether this generalises to the athlete’s dietary intake.
Desert dwellers relish salt, possibly to support hydration. They trade in salt and preserve their food in it, and it sustains their crucially important livestock and features prominently in their folklore(Reference Leshem, Saadi and Alem118).
In some salt-wasting diseases, such as congenital adrenal hyperplasia, children frequently prefer salt to medication. It may ameliorate their affliction acutely and so may become favoured, whereas medication requires persistence and compliance, and even though its therapy is more comprehensive, long delayed effects condition poorly(Reference Tordoff and Coldwell95).
Salt may mitigate pain(Reference Foo and Mason132): dietary Na has an inconclusive direct relation to headache, is inversely related to migraine(Reference Pogoda, Gross and Arakaki133) and may alleviate certain forms of fibromyalgia(Reference De Lorenzo, Hargreaves and Kakkar134,Reference Graham135) . There is even a hypothesis that our high salt intake crucially protects us in the case of the many desiccating diseases(Reference Fessler62).
A long-standing issue of whether Na can be stored in the body has been resolved with the discovery of hypertonic Na in subcutaneous skin and muscle(Reference Titze136). More importantly, immunity may be compromised by high salt intake, although some immune protection may be reduced with reduced salt(Reference Jantsch, Schatz and Friedrich137,Reference Rucker, Rudemiller and Crowley138) .
Such beneficial effects might condition a preference for the taste of salt, contributing to its intake(Reference Kochli, Tenenbaum-Rakover and Leshem35,Reference Wald and Leshem76,Reference Cocores and Gold123) . Similar ideas have been considered for food intake, where palatability is central to the reinforcement hypothesis contributing to food intake and obesity(Reference Morris, Na and Johnson2,Reference Yeomans, Blundell and Leshem125,Reference Epstein and Leddy139) . Salt, of course, contributes greatly to palatability.
It is also possible that short-term negative effects condition reduced salt intake(Reference Wald and Leshem76), but their potential for regulation of salt intake has not been explored.
Humans dislike salt and do not eat it
A very significant and frequently overlooked observation is that animals eat salt(Reference Leshem, Langberg and Epstein94,Reference Bowell, Warren and Redmond140) , whereas humans do not(Reference Leshem16). Surprisingly, the delectability of salt for humans is unrelated to its taste. Very few people eat pure salt (an observation that militates against the addiction hypothesis).
Pure salt is inedible not merely because of it being concentrated (and activating aversive signalling taste receptors(Reference Smith, Treesukosol and Paedae82,Reference Sandhu, Fernando and Irvine83) ), given that it is also aversive at low concentrations in water. This may be more than an issue of hedonism; it may be a physiological response because salt in solution is emetic(Reference Casavant and Fitch141). Indeed, there are no salty drinks. Paradoxically, the same concentration (about 1 %) in an adulterated aqueous solution, such as tomato soup or beef broth, is relished(Reference Leshem16,Reference Hayes, Sullivan and Duffy56) .
In contrast, animals lick rock salt, do not like salt in food (wherein its intake cannot be regulated(Reference Beauchamp and Bertino142,Reference Stricker, Verbalis and Stricker143) ), prefer it in solution (wherein its intake can be regulated to the required 0·9 %(Reference Stricker, Verbalis and Stricker143)) and relish it most in the 0·9 % physiological concentration (like a saline drip). Hyponatraemic humans, however, require health workers to both diagnose their condition and administer Na(Reference Montain, Sawka and Wenger68,Reference Moritz and Ayus78,Reference Hao, Li and Zhang111–Reference Evans, James and Shirreffs114) . Further, Na-deficient animals recognise Na in any mineral form(Reference Schulkin67), whereas humans do not, taking only the single form, table salt (NaCl), suggesting that Na, the life-essential ion, is not the target cation taste as it is for animals(Reference Leshem16).
The comparison with the animal research is instructive because the animal behaviour, as outlined above, defines the behavioural requirements for the maintenance of Na homoeostasis, each of which humans abrogate, suggesting strongly that the humans’ love of salt in food does not stem from physiological Na requirement.
The causes must therefore be behavioural, with the caveat that there may well be specific requirements during early development and growth.
Limitations
Confirmation, but particularly further research, of the determinants of salt intake is clearly required. Specifically, the significance of conditioning to excess Na intake is indeterminate. Research of this underrepresented science is limited at present, but resources for its encouragement should be found. The alternative notion that the excess salting of food has no palpable cause is not tenable.
Conclusions
Throughout life, our love of salt peaks and dips. Salt flavours our food and promotes its consumption and thus possibly obesity; it sustains and protects us in physical exertion, may occasionally be remedial, contributes to our growth and ailments and generates controversy(Reference Trinquart, Johns and Galea27).
Nonetheless, salt itself is inedible.
The attribution of this complexity to early dietary exposure and processed food is unsubstantiated, as well as inadequate.
The fundamental question persists of why we love the taste of salt.
An understanding of the predilection for salt taste should improve evidence-based intervention for effective reduction of the health risks associated with both Na surfeit and deficiency. For example, individual control of salt intake could benefit from counselling focused on children born to mothers who had high rates of nausea and vomiting during pregnancy, were hyponatraemic as neonates, or suffered Na losses in infancy, people with mood issues, and dissociating salt for exertion and diet for athletes. None of this is currently applied, and probably little known among those working to regulate Na intake. Note that salt need not be the direct cause of its associated effects, but can serve as the sensory marker for them as a ‘conditioned stimulus’ in conditioning theory.
However, most critical and promising are the determinants of salt intake, the discovery of which is surely awaiting novel and creative approaches in this crucial domain of human behaviour, nutrition and illness.
As astonishing science prepares to launch our first spaceship to Mars, it has yet to unravel the reasons for our daily 80 000-tonne sprinkle of salt(Reference Powles, Fahimi and Micha41). Despite not knowing why we need so much salt, the ship will be supplied with it(Reference Lerchl, Rakova and Dahlmann144).
Acknowledgements
This study was supported by the Israel Science Foundation (902/00-2 and 7481478) and the Israel Ministry of Health (1043-3-00000).
The author declares that there are no conflicts of interest.










