Book contents
- Trauma Anesthesia
- Trauma Anesthesia
- Copyright page
- Contents
- Contributors
- Foreword to the second edition
- Foreword to the second edition
- Foreword to the first edition
- Foreword to the first edition
- Preface
- Acknowledgments
- Section 1 Initial management of the trauma patient
- Chapter 1 Mechanisms and demographics
- Chapter 2 Trauma in the prehospital environment and the emergency department
- Chapter 3 Trauma airway management
- Chapter 4 Shock management
- Chapter 5 Establishing vascular access in the trauma patient
- Chapter 6 Massive blood transfusion in trauma care
- Chapter 7 Blood loss: does it change my intravenous anesthetic?
- Chapter 8 Fluid and blood therapy in trauma
- Section 2 Techniques for monitoring, imaging, and pain relief
- Section 3 Anesthetic considerations
- Section 4 Special populations
- Section 5 Organization of trauma management
- Index
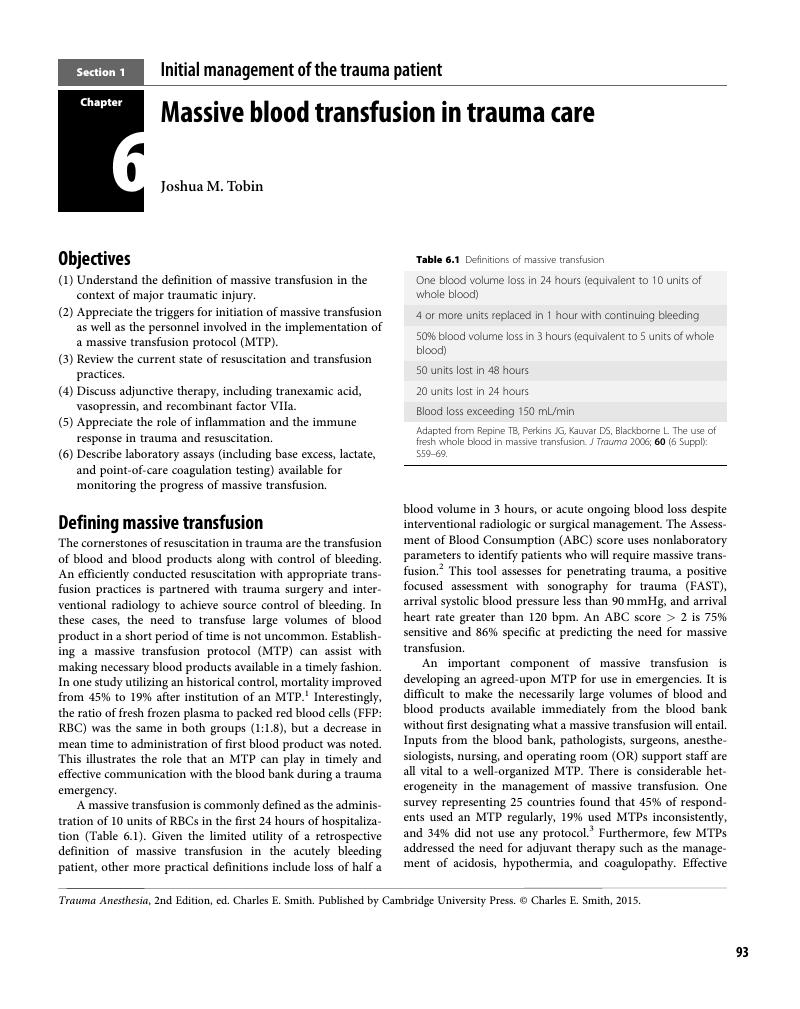
Chapter 6 - Massive blood transfusion in trauma care
from Section 1 - Initial management of the trauma patient
Published online by Cambridge University Press: 05 April 2015
- Trauma Anesthesia
- Trauma Anesthesia
- Copyright page
- Contents
- Contributors
- Foreword to the second edition
- Foreword to the second edition
- Foreword to the first edition
- Foreword to the first edition
- Preface
- Acknowledgments
- Section 1 Initial management of the trauma patient
- Chapter 1 Mechanisms and demographics
- Chapter 2 Trauma in the prehospital environment and the emergency department
- Chapter 3 Trauma airway management
- Chapter 4 Shock management
- Chapter 5 Establishing vascular access in the trauma patient
- Chapter 6 Massive blood transfusion in trauma care
- Chapter 7 Blood loss: does it change my intravenous anesthetic?
- Chapter 8 Fluid and blood therapy in trauma
- Section 2 Techniques for monitoring, imaging, and pain relief
- Section 3 Anesthetic considerations
- Section 4 Special populations
- Section 5 Organization of trauma management
- Index
Summary
- Type
- Chapter
- Information
- Trauma Anesthesia , pp. 93 - 104Publisher: Cambridge University PressPrint publication year: 2015