Book contents
- Ovarian Stimulation
- Ovarian Stimulation
- Copyright page
- Dedication
- Contents
- Contributors
- About the Editors
- Foreword
- Preface to the first edition
- Preface to the second edition
- Section 1 Mild Forms of Ovarian Stimulation
- Section 2 Ovarian Hyperstimulation for IVF
- Section 3 Difficulties and Complications of Ovarian Stimulation and Implantation
- Section 4 Non-conventional Forms Used during Ovarian Stimulation
- Section 5 Alternatives to Ovarian Hyperstimulation and Delayed Transfer
- Section 6 Procedures before, during, and after Ovarian Stimulation
- Index
- References
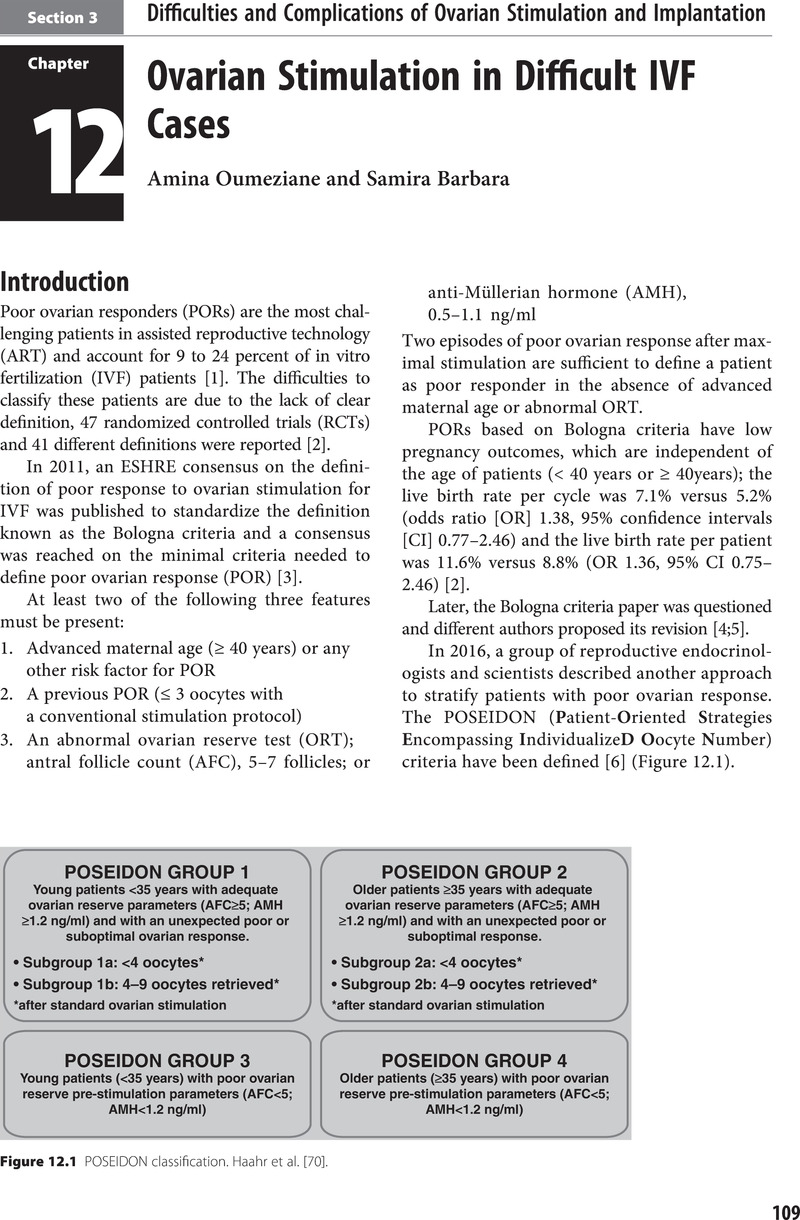
Section 3 - Difficulties and Complications of Ovarian Stimulation and Implantation
Published online by Cambridge University Press: 14 April 2022
- Ovarian Stimulation
- Ovarian Stimulation
- Copyright page
- Dedication
- Contents
- Contributors
- About the Editors
- Foreword
- Preface to the first edition
- Preface to the second edition
- Section 1 Mild Forms of Ovarian Stimulation
- Section 2 Ovarian Hyperstimulation for IVF
- Section 3 Difficulties and Complications of Ovarian Stimulation and Implantation
- Section 4 Non-conventional Forms Used during Ovarian Stimulation
- Section 5 Alternatives to Ovarian Hyperstimulation and Delayed Transfer
- Section 6 Procedures before, during, and after Ovarian Stimulation
- Index
- References
Summary
- Type
- Chapter
- Information
- Ovarian Stimulation , pp. 109 - 188Publisher: Cambridge University PressPrint publication year: 2022