Book contents
- Imaging Acute Neurologic Disease
- Imaging Acute Neurologic Disease
- Copyright page
- Contents
- Contributors
- Preface
- Chapter 1 Disorders of consciousness
- Chapter 2 Delirium and confusion
- Chapter 3 Intellectual dysfunction
- Chapter 4 Headache
- Chapter 5 Back pain
- Chapter 6 Acute vision loss
- Chapter 7 Dizziness, nystagmus, and disequilibrium
- Chapter 8 Seizures
- Chapter 9 Acute and subacute ataxia
- Chapter 10 Syncope
- Chapter 11 Fever
- Chapter 12 Acute, focal neurological symptoms
- Chapter 13 Acute, multifocal neurological symptoms
- Chapter 14 Acute brain trauma
- Chapter 15 Spinal cord trauma
- Chapter 16 Bladder, bowel, and sexual dysfunction
- Chapter 17 Parkinsonism
- Chapter 18 Hyperkinesia, dystonia, and tics
- Chapter 19 Non-Parkinson’s disease tremor
- Chapter 20 Neuromuscular weakness
- Chapter 21 Paresthesias and dysesthesias
- Chapter 22 Weakness and fatigue
- Chapter 23 Hearing loss and tinnitus
- Appendix: Risks associated with imaging procedures in acute neurologic disease
- Index
Chapter 9 - Acute and subacute ataxia
Published online by Cambridge University Press: 05 October 2014
- Imaging Acute Neurologic Disease
- Imaging Acute Neurologic Disease
- Copyright page
- Contents
- Contributors
- Preface
- Chapter 1 Disorders of consciousness
- Chapter 2 Delirium and confusion
- Chapter 3 Intellectual dysfunction
- Chapter 4 Headache
- Chapter 5 Back pain
- Chapter 6 Acute vision loss
- Chapter 7 Dizziness, nystagmus, and disequilibrium
- Chapter 8 Seizures
- Chapter 9 Acute and subacute ataxia
- Chapter 10 Syncope
- Chapter 11 Fever
- Chapter 12 Acute, focal neurological symptoms
- Chapter 13 Acute, multifocal neurological symptoms
- Chapter 14 Acute brain trauma
- Chapter 15 Spinal cord trauma
- Chapter 16 Bladder, bowel, and sexual dysfunction
- Chapter 17 Parkinsonism
- Chapter 18 Hyperkinesia, dystonia, and tics
- Chapter 19 Non-Parkinson’s disease tremor
- Chapter 20 Neuromuscular weakness
- Chapter 21 Paresthesias and dysesthesias
- Chapter 22 Weakness and fatigue
- Chapter 23 Hearing loss and tinnitus
- Appendix: Risks associated with imaging procedures in acute neurologic disease
- Index
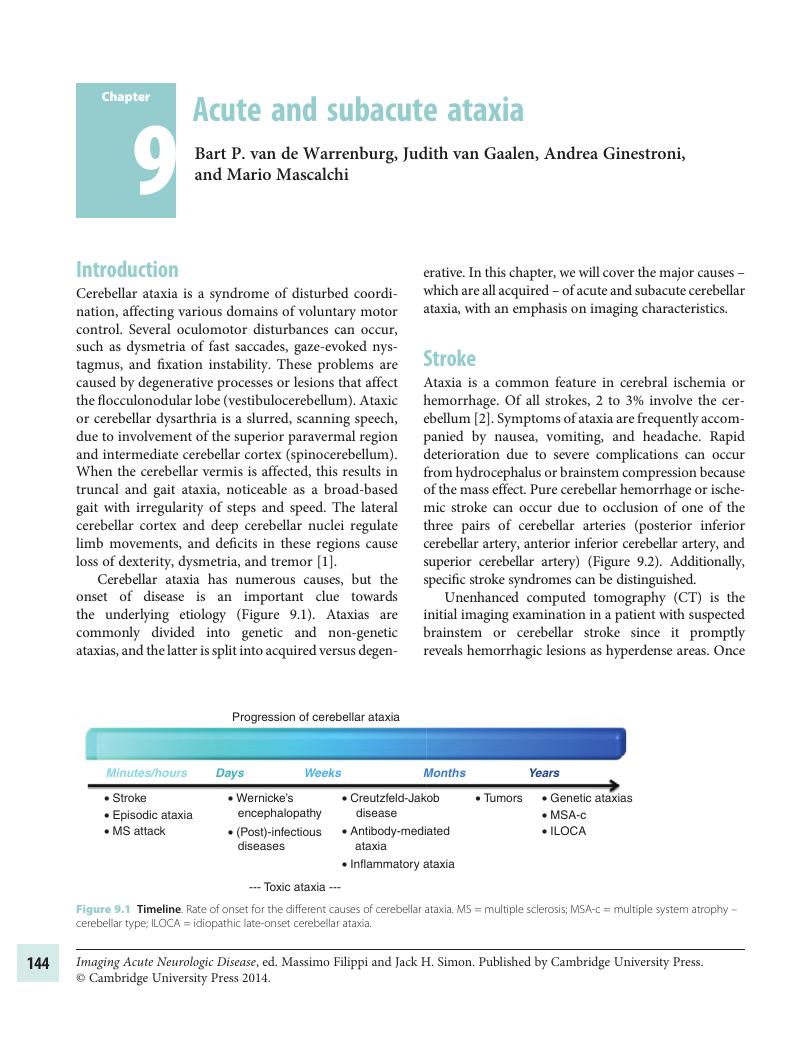
Summary
- Type
- Chapter
- Information
- Imaging Acute Neurologic DiseaseA Symptom-Based Approach, pp. 144 - 165Publisher: Cambridge University PressPrint publication year: 2014