69 results
Patterns, predictors, and patient-reported reasons for antidepressant discontinuation in the WHO World Mental Health Surveys
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 1 / January 2024
- Published online by Cambridge University Press:
- 14 September 2023, pp. 67-78
-
- Article
- Export citation
Changes on depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 32 / 2023
- Published online by Cambridge University Press:
- 01 September 2023, e55
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Empower: Design of a digital intervention for workplace stress and mental health. A European study
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S160-S161
-
- Article
-
- You have access
- Open access
- Export citation
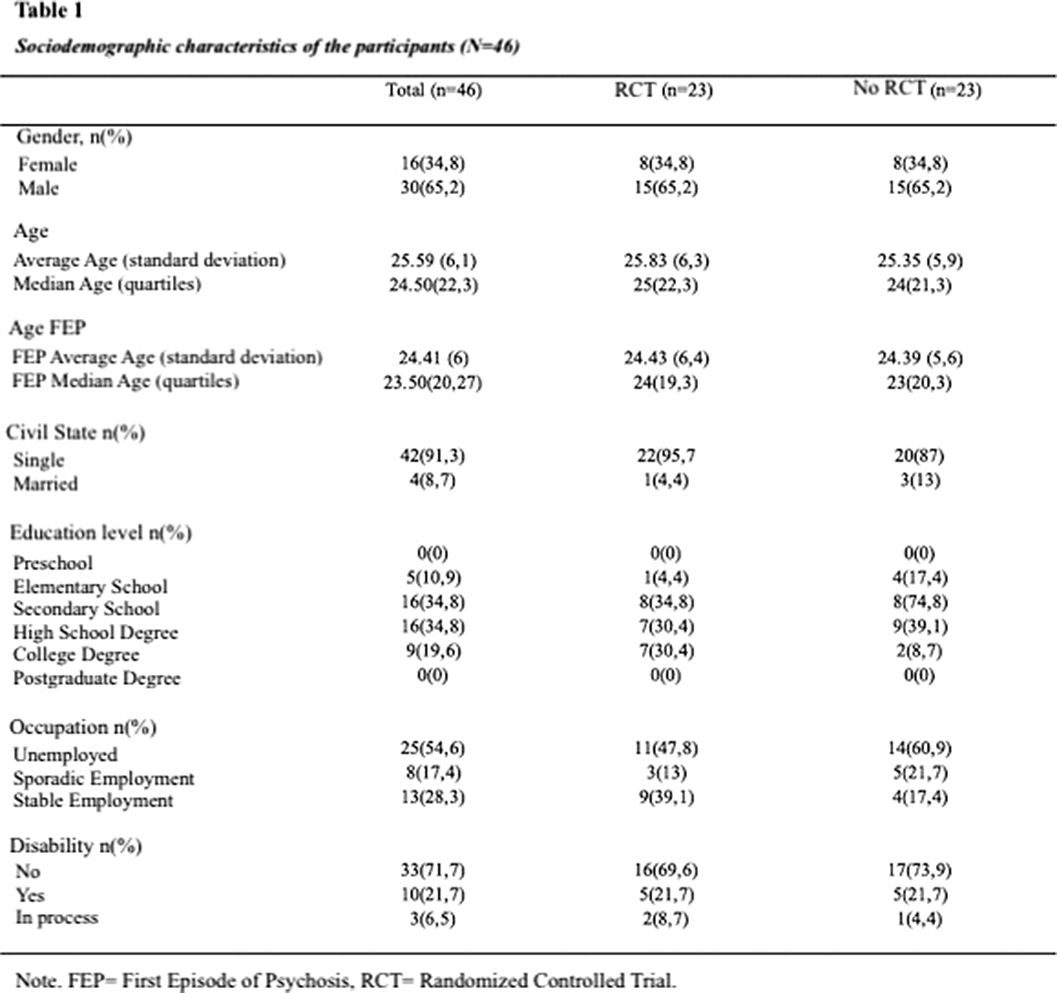
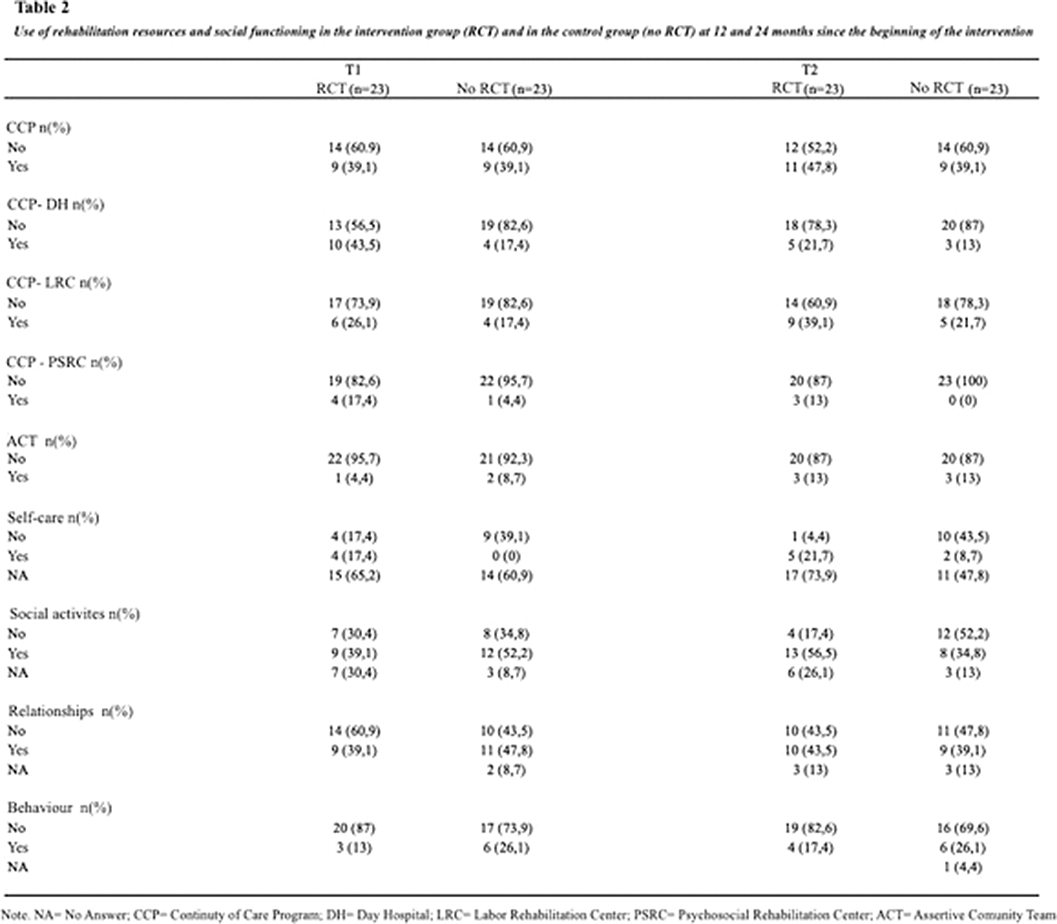
“Social functioning and use of rehabilitation resources in a group of people who experienced a first episode of psychosis and participated in a psychotherapeutic group program versus a control group”
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S185
-
- Article
-
- You have access
- Open access
- Export citation
The usability of daytime and night-time heart rate dynamics as digital biomarkers of depression severity
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 8 / June 2023
- Published online by Cambridge University Press:
- 15 May 2023, pp. 3249-3260
-
- Article
-
- You have access
- HTML
- Export citation
Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population - RETRACTION
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 32 / 2023
- Published online by Cambridge University Press:
- 13 March 2023, e15
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The association between persistent cognitive difficulties and depression and functional outcomes in people with major depressive disorder
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 13 / October 2023
- Published online by Cambridge University Press:
- 13 December 2022, pp. 6334-6344
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Remote Assessment of Disease and Relapse in Major Depressive Disorder (RADAR-MDD): Recruitment, retention, and data availability in a longitudinal remote measurement study
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S112
-
- Article
-
- You have access
- Open access
- Export citation
Clinical validation of EDIT-B test for the diagnosis of bipolar disorder
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S413
-
- Article
-
- You have access
- Open access
- Export citation
Mental impact of Covid-19 among Spanish healthcare workers. A large longitudinal survey
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 31 / 2022
- Published online by Cambridge University Press:
- 29 April 2022, e28
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Previous disorders and depression outcomes in individuals with 12-month major depressive disorder in the World Mental Health surveys
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 30 / 2021
- Published online by Cambridge University Press:
- 11 November 2021, e70
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Antidepressant use in low- middle- and high-income countries: a World Mental Health Surveys report
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 4 / March 2023
- Published online by Cambridge University Press:
- 23 September 2021, pp. 1583-1591
-
- Article
- Export citation
Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 30 / 2021
- Published online by Cambridge University Press:
- 02 June 2021, e49
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The role of ageing in the wish to be dead: disentangling age, period and cohort effects in suicide ideation in European population
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 30 / 2021
- Published online by Cambridge University Press:
- 18 February 2021, e17
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Thirty-day suicidal thoughts and behaviours in the Spanish adult general population during the first wave of the Spain COVID-19 pandemic
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 30 / 2021
- Published online by Cambridge University Press:
- 17 February 2021, e19
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Comorbidity within mental disorders: a comprehensive analysis based on 145 990 survey respondents from 27 countries
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 29 / 2020
- Published online by Cambridge University Press:
- 12 August 2020, e153
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Patterns of care and dropout rates from outpatient mental healthcare in low-, middle- and high-income countries from the World Health Organization's World Mental Health Survey Initiative
-
- Journal:
- Psychological Medicine / Volume 51 / Issue 12 / September 2021
- Published online by Cambridge University Press:
- 28 April 2020, pp. 2104-2116
-
- Article
- Export citation
PW01-181 - Economic Consequences Of Medication Nonadherence In The Treatment Of Schizophrenia: 36-Month Results From The Soho (Schizophrenia Outpatient Health Outcomes) Study
-
- Journal:
- European Psychiatry / Volume 25 / Issue S1 / 2010
- Published online by Cambridge University Press:
- 17 April 2020, 25-E1588
-
- Article
-
- You have access
- Export citation
Translation of Randomised Controlled Trial Findings into Clinical Practice: Comparison of Olanzapine and Valproate in the Emblem Study
-
- Journal:
- European Psychiatry / Volume 24 / Issue S1 / January 2009
- Published online by Cambridge University Press:
- 16 April 2020, 24-E314
-
- Article
-
- You have access
- Export citation
The role of personality disorders on drug dependence treatment outcomes following inpatient detoxification
-
- Journal:
- European Psychiatry / Volume 19 / Issue 4 / June 2004
- Published online by Cambridge University Press:
- 16 April 2020, pp. 187-192
-
- Article
- Export citation