Book contents
- Biopsychosocial Factors in Obstetrics and Gynaecology
- Biopsychosocial Factors in Obstetrics and Gynaecology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Section 1 Generic Issues
- Chapter 1 Promoting and Implementing the Biopsychosocial Perspective in Obstetrics and Gynaecology
- Chapter 2 Psychosocial Context of Illness and Well-Being in Women’s Health
- Chapter 3 Epigenetics
- Chapter 4 Communicating Effectively
- Chapter 5 Biopsychosocial Aspects of Eating Disorders in Obstetrics and Gynaecology
- Chapter 6 The Brain, Heart and Human Behaviour
- Chapter 7 Complementary Medicine for Women’s Healthcare
- Chapter 8 Domestic Violence and Abuse
- Chapter 9 Female Genital Cutting
- Section 2 Gynaecology
- Section 3 Sexual and Reproductive Health
- Section 4 Obstetrics and Maternal Health
- Appendix: RCOG Checklist of Hints and Tips to Support Clinical Practice in the Management of Gender-Based Violence
- Index
- References
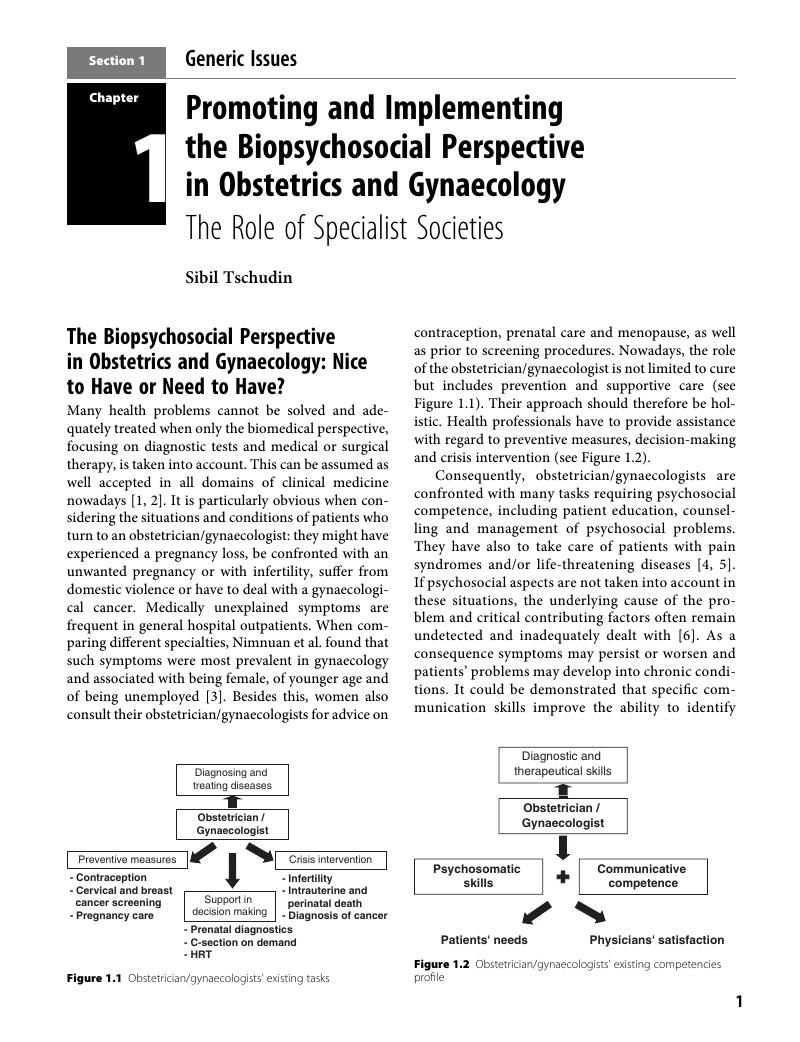
Chapter 1 - Promoting and Implementing the Biopsychosocial Perspective in Obstetrics and Gynaecology
The Role of Specialist Societies
from Section 1 - Generic Issues
Published online by Cambridge University Press: 30 August 2017
- Biopsychosocial Factors in Obstetrics and Gynaecology
- Biopsychosocial Factors in Obstetrics and Gynaecology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Section 1 Generic Issues
- Chapter 1 Promoting and Implementing the Biopsychosocial Perspective in Obstetrics and Gynaecology
- Chapter 2 Psychosocial Context of Illness and Well-Being in Women’s Health
- Chapter 3 Epigenetics
- Chapter 4 Communicating Effectively
- Chapter 5 Biopsychosocial Aspects of Eating Disorders in Obstetrics and Gynaecology
- Chapter 6 The Brain, Heart and Human Behaviour
- Chapter 7 Complementary Medicine for Women’s Healthcare
- Chapter 8 Domestic Violence and Abuse
- Chapter 9 Female Genital Cutting
- Section 2 Gynaecology
- Section 3 Sexual and Reproductive Health
- Section 4 Obstetrics and Maternal Health
- Appendix: RCOG Checklist of Hints and Tips to Support Clinical Practice in the Management of Gender-Based Violence
- Index
- References
Summary
- Type
- Chapter
- Information
- Publisher: Cambridge University PressPrint publication year: 2017
References
- 1
- Cited by