Book contents
- Management of Complex Treatment-Resistant Psychotic Disorders
- Management of Complex Treatment-Resistant Psychotic Disorders
- Copyright page
- Contents
- Contributors
- Acknowledgements
- Abbreviations
- List of Icons
- Introduction
- Part I Treatment Strategies
- Part II Medication Reference Tables
- First-Generation (Typical) Antipsychotics
- Second-Generation (Atypical) Antipsychotics
- Dopamine Partial Agonist Antipsychotics
- Medications for Motor/Neurologic Adverse Effects
- Mood Stabilizers
- Selective Serotonin Reuptake Inhibitor Antidepressants
- SSRI/5HT1A Partial Agonist Antidepressants
- Serotonin/Norepinephrine Reuptake Inhibitor Antidepressants
- Mixed Mechanism Antidepressants
- Tricyclic Antidepressants
- Monoamine Oxidase Inhibitor Antidepressants
- Anxiolytics
- Sedatives
- Circadian Regulators
- Stimulants
- Histaminic Stimulants
- Cognitive Agents
- α2-Adrenergic Agonists
- Appendices
- Index
- References
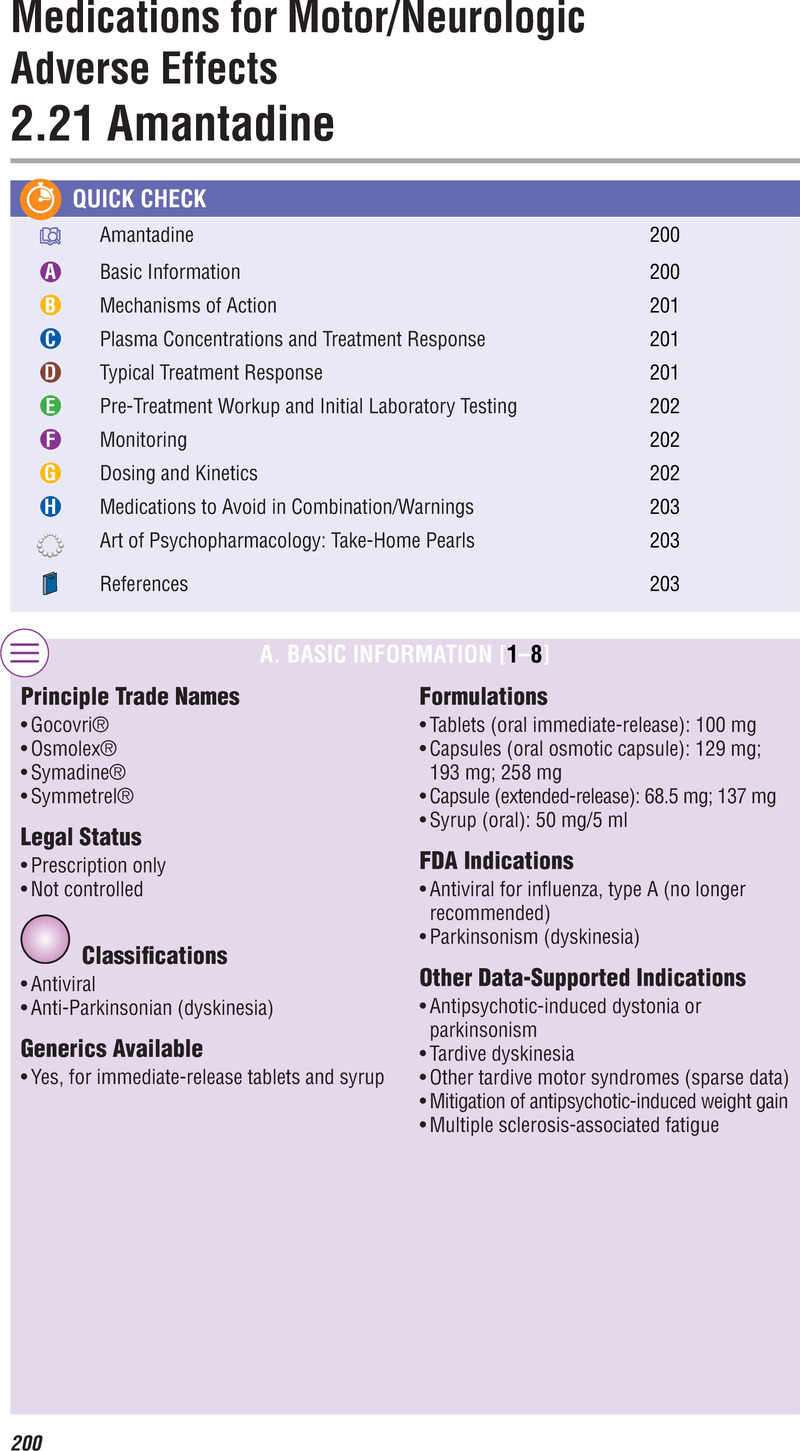
Medications for Motor/Neurologic Adverse Effects
from Part II - Medication Reference Tables
Published online by Cambridge University Press: 19 October 2021
- Management of Complex Treatment-Resistant Psychotic Disorders
- Management of Complex Treatment-Resistant Psychotic Disorders
- Copyright page
- Contents
- Contributors
- Acknowledgements
- Abbreviations
- List of Icons
- Introduction
- Part I Treatment Strategies
- Part II Medication Reference Tables
- First-Generation (Typical) Antipsychotics
- Second-Generation (Atypical) Antipsychotics
- Dopamine Partial Agonist Antipsychotics
- Medications for Motor/Neurologic Adverse Effects
- Mood Stabilizers
- Selective Serotonin Reuptake Inhibitor Antidepressants
- SSRI/5HT1A Partial Agonist Antidepressants
- Serotonin/Norepinephrine Reuptake Inhibitor Antidepressants
- Mixed Mechanism Antidepressants
- Tricyclic Antidepressants
- Monoamine Oxidase Inhibitor Antidepressants
- Anxiolytics
- Sedatives
- Circadian Regulators
- Stimulants
- Histaminic Stimulants
- Cognitive Agents
- α2-Adrenergic Agonists
- Appendices
- Index
- References
Summary
- Type
- Chapter
- Information
- Management of Complex Treatment-resistant Psychotic Disorders , pp. 200 - 216Publisher: Cambridge University PressPrint publication year: 2021