At present, BMI is widely used as an indicator to evaluate the nutritional status of children and adolescents in the world(Reference Abarca-Gómez, Abdeen and Hamid1,Reference Dong, Zou and Yang2) . Being overweight or obese during childhood or adolescence is associated with short-term and long-term risk of adverse health outcomes such as hypertension, dyslipidaemia(Reference Friedemann, Heneghan and Mahtani3), target organ damage(Reference Cote, Harris and Panagiotopoulos4) and CVD(Reference Llewellyn, Simmonds and Owen5). Recently, the prevalence of overweight and obesity among children and adolescents has been increasing around the world, including in China(Reference Abarca-Gómez, Abdeen and Hamid1,Reference Wang, Xue and Du6–Reference Ng, Fleming and Robinson8) . For instance, between 1997 and 2011 in China, the prevalence of overweight (including obesity) among children and adolescents aged 7–17 years increased from 6·5 to 15·5 % in boys and from 4·6 to 10·4 % in girls(Reference Wang, Xue and Du6), and between 2011 and 2015, the prevalence of overweight (including obesity) remained stable in children aged 7–11 years but continued to increase in adolescents aged 12–18 years(Reference Zhang, Wang and Wang9). Despite these increasing trends at the upper end of the BMI distribution, the prevalence of stunting or thinness remains prevalent in children living in developing countries(Reference de Onis, Onyango and Borghi10). In rural areas or some remote provinces of China, there was a relatively high prevalence of stunting and thinness. For example, in Guizhou province in 2014, the prevalence of stunting among children and adolescents aged 7–18 years was 8·9 % in boys and 9·0 % in girls, and the prevalence of thinness was 5·6 % in boys and 3·9 % in girls(Reference Song, Agardh and Ma7).
The Tibet Autonomous Region of China is located at high altitude in the Qing-Tibetan highland. The hypoxic environments, socio-economic conditions and lifestyle factors in high altitude areas may have significant impacts on children’s growth and development(Reference Niermeyer, Andrade Mollinedo and Huicho11). The majority of Tibetan children and adolescents live at high altitudes which may lead to the unhealthy nutritional status among them(Reference Harris, Crawford and Yangzom12). Several studies have shown a high prevalence of stunting, thinness and underweight among Tibetan children aged < 10 years(Reference Harris, Crawford and Yangzom12–Reference Dang, Yan and Yamamoto14), indicating that child malnutrition is positively related to high altitude(Reference Dang, Yan and Yamamoto14). However, up to date, no study has focused on the nutritional status of Tibetan adolescents aged 12–17 years living at high altitude. We have a hypothesis that Tibetan adolescents living at high altitude areas may be more likely to have thinness.
Using data from one cross-sectional survey conducted between August and September in 2018 in Shigatse City, Tibet municipality, we aimed to assess the prevalence of thinness, overweight and obesity among Tibetan adolescents aged 12–17 years.
Methods
Study population
Data were from a cross-sectional survey conducted from August to September in 2018 in Shigatse City (with an average altitude of more than 4000 m(Reference Liu15)), Tibet municipality. Using a convenient cluster sampling method, we selected three junior high schools in Yadong County, Gamba County and Sangzhutun District of Shigatse City, and three senior high schools in Sangzhutun District of Shigatse City (as senior high schools are usually located in urban regions of Shigatse City). The six high schools were conveniently selected due to their good compliance and cooperation. All students in selected schools were invited to participate in the survey. In this survey, 3250 participants aged 10–24 years with complete physical and lifestyle measurements were initially recruited. The ethnic classification of a participant was determined according to the identity certificate information provided by the school. After the completion of data collection, we excluded those who were not Tibetan, younger than 12 years or older than 17 years and those with missing data on physical or lifestyle measurements, and thus a total of 2642 Tibetan adolescents aged 12–17 years with complete data on sex, age, height, weight and lifestyle variables were finally included. Signed informed consent was obtained from each participant and his/her guardians/parents.
Measurements
Height and weight were measured using the HGM 300 ultrasonic height and weight scale in light clothes without shoes to the nearest 0·1 cm and 0·1 kg, respectively. BMI was calculated as weight in kilograms divided by the square of height in meters. Height and weight were measured twice, respectively, and the average value was used in the analyses.
Nutritional status was defined according to each of three BMI classifications: the China definition(16,17) , the International Obesity Task Force (IOTF) definition(Reference Cole and Lobstein18) and the WHO definition(Reference de Onis, Onyango and Borghi19). Based on the China definition(16,17) , overweight and obesity were defined according to the percentile cut-offs by sex and age in Chinese school-age children and adolescents, and thinness was defined according to percentile thresholds for thinness of school-age children and adolescents. Based on the IOTF definition, thinness, overweight and obesity BMI percentile cut-offs were defined as the linkage of international growth curve data for boys and girls with adult BMI cut-offs of 18·5 kg/m2 (thin), BMI 25 kg/m2 (overweight) and BMI 30 kg/m2 (obese) at the age of 18 years(Reference Cole and Lobstein18). Based on the WHO definition, thinness, overweight and obesity were defined as BMI for age and sex <-2 sd, ≥1 sd and <2 sd, and ≥2 sd above the WHO Growth Reference median value, respectively(Reference de Onis, Onyango and Borghi19). The IOTF definition and WHO definition are two widely used international definitions to assess the nutritional status in children and adolescents. The China definition is widely used in Chinese children and adolescents. In the current study, three different definitions were used to assess the prevalence of thinness, overweight and obesity among Tibetan adolescents aged 12–17 years, which can comprehensively reflect the nutritional status among Tibetan adolescents, and can be convenient for prevalence comparison across different regions and countries.
Socio-demographic and lifestyle factors were collected using a self-reported questionnaire, which was distributed by trained investigators to ensure the collection of reliable data. Socio-demographic factors included sex, age and race. Lifestyle factors included intakes of fruit, vegetable and meat, water drinking, physical activity, screen time and sleep duration.
Statistical analysis
Continuous variables including age, height, weight and BMI were expressed as mean and sd, and sex difference was examined using the t-test. Categorical variables including nutritional status, intakes of fruit, vegetable or meat (<1 v. ≥1 time/d), water drinking (≤1 v. >1 time/d), physical activity (<1 v. ≥1 time/d), screen time (≤2 v. >2 h/d) and sleep duration (<8 v. ≥8 h/d) were expressed as proportions, and sex difference was examined using the χ 2 test. General linear regression models were used to examine the trend of BMI with increase of age, in which BMI was the dependent variable and age was the independent variable. Logistic regression models were used to examine the trends in prevalence of thinness, overweight or obesity with increase of age, in which thinness, overweight and obesity, respectively, were the dependent variables, and age was the independent variable, and the cluster effect (i.e., class) was considered in the model. Multivariate logistic regression models were used to examine the association between lifestyle factors and nutritional status. All statistical analyses were performed using SAS software (version 9.4). A two-sided P < 0·05 was considered statistically significant.
Results
A total of 2642 Tibetan adolescents (44·4 % boys) were included in our study. The mean age of the surveyed participants was 15·3 (sd 1·7) years. Boys were taller than girls (158·3 v. 153·8 cm; P < 0·001). However, girls had greater mean values of BMI than boys (19·9 v. 18·6 kg/m2; P < 0·001) (Table 1). Girls were more likely to consume vegetable one or more times per d, to sleep < 8 h/d and to spend screen time more than 2 h/d. Boys were more likely to consume meat one or more times per d and to perform physical activity one or more times per d. However, there was no significant difference in weight, fruit intake and water drinking between both sexes (online supplementary material, Supplemental Table S1).
Table 1 Characteristics of the study population*

* Continuous variables are presented as mean and sd, and sex difference was examined using the t-test.
As shown in Table 2, BMI showed an upward trend with increase of age among both sexes (both P for trend <0·001). Based on the China, IOTF and WHO definitions, the prevalence of overweight/obesity among Tibetan adolescents was 5·4 %/1·4 %, 4·4 %/0·7 % and 5·7 %/0·9 %, respectively, while the prevalence of thinness was 9·4, 14·7 and 2·8 %, respectively (Fig. 1). Table 3 presents the prevalence of thinness, overweight and obesity among Tibetan adolescents according to sex and three BMI classifications. The prevalence of thinness and overweight was significantly different between sexes according to each of three BMI classifications (P < 0·001). There was no significant difference in the prevalence of obesity between both sexes according to each of three BMI classifications.
Table 2 BMI (kg/m2) of Tibetan adolescents aged 12–17 years by age and gender*

* Data are presented as mean and sd.
† P for trend (age) was tested using linear regression analysis.
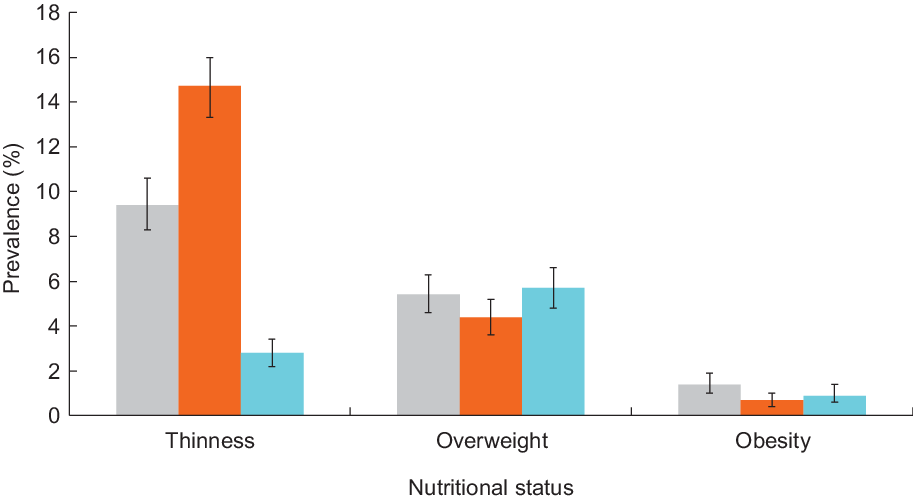
Fig. 1 Prevalence (%) of thinness, overweight and obesity among Tibetan adolescents by different BMI classifications. ![]() , China definition;
, China definition; ![]() , IOTF definition;
, IOTF definition; ![]() , WHO definition
, WHO definition
Table 3 Prevalence of thinness, overweight and obesity among Tibetan adolescents by gender and different BMI classifications
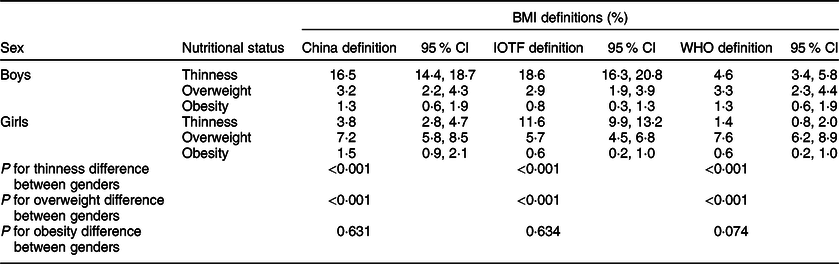
IOTF, International Obesity Task Force.
As shown in online supplementary material, Supplemental Table S2, there was no significant trend in thinness with increase of age according to the China and IOTF definitions, but the prevalence of thinness tended to increase with increase of age in boys according to the IOTF definition (P for trend <0·05). In contrast, the prevalence of thinness tended to decrease with increase of age in girls according to the IOTF definition and in total sample according to the WHO definition (P for trend <0·05). There were no significant trends in overweight or obesity according to the China, IOTF and WHO definitions.
Online supplementary material, Supplemental Table S3 presents potential lifestyle factors associated with thinness, overweight and obesity among Tibetan adolescents. Short sleep duration was associated with reduced risk of thinness. Tibetan adolescents who consumed fruits less than one time per d had an increased risk of overweight. Tibetan adolescents who spent screen time more than 2 h/d had an increased risk of overweight.
Discussion
Our findings showed a relatively low prevalence of overweight and obesity and a high prevalence of thinness among Tibetan adolescents living at high altitude. The prevalence of thinness differed substantially depending on the classification used to assign nutritional status, while only minor differences were found for the prevalence of overweight and obesity. The difference in prevalence of thinness might be due to that the IOTF definition is based on data collected from six countries(Reference Cole and Lobstein18), the WHO definition is based on data collected from the USA alone(Reference de Onis, Onyango and Borghi19) and the China definition is based on data collected from China. There are differences in living environments and lifestyle behaviours between the participants used for the development of three definitions, and thus they result in different BMI percentile cut-offs for three different definitions. But the current use of three definitions will make our results comparable with participants from China and outside China.
The prevalence of overweight and obesity in our study is lower than that reported for Chinese children and adolescents between 2011 and 2015, based on the IOTF and WHO definitions(Reference Zhang, Wang and Wang9), and is also lower than what has been reported in developed countries based on the IOTF definition(Reference Ng, Fleming and Robinson8). One cross-sectional study in China indicated that the prevalence of excess body weight (including overweight and obesity) in Tibetan adolescents aged 7–18 years was 12·0 % (using the China definition)(Reference Dong, Zou and Yang2), which is higher than our findings (the prevalence was 6·9 % using the same definition). However, findings from one previous study were consistent with ours with the prevalence of overweight and obesity in children aged 9–10 years in Lhasa was 3·5 and 0·5 % in girls and 4·8 and 1·5 % in boys, based on the WHO definition(Reference Bianba, Yangzong and Gonggalanzi13).
One study showed that the prevalence of moderate and severe thinness in children and adolescents aged 5–19 years worldwide in 2016 was 8·4 % in girls and 12·4 % in boys based on the WHO definition(Reference Abarca-Gómez, Abdeen and Hamid1), and a large national successive cross-sectional survey in China showed that the prevalence of stunting decreased from 16·4 % in 1985 to 2·3 % in 2014, and the prevalence of thinness decreased from 8·4 % in 1985 to 4·0 % in 2014 based on the WHO definition(Reference Song, Agardh and Ma7). Compared with the above results, the prevalence of thinness in our study is lower than that in children and adolescents worldwide but higher than the average level in China. A study in 2018 reported that the prevalence of thinness in Tibetan adolescents aged 7–18 years was 14·9 % in boys and 9·2 % in girls based on the China definition(Reference Dong, Zou and Yang2), which is similar to our findings for boys but higher than girls in our study. Another recent review of 398 Tibetan children aged 9–10 years showed that the prevalence of underweight was 36·7 % in girls and 31·1 % in boys based on the WHO definition, which is much higher than what we found(Reference Bianba, Yangzong and Gonggalanzi13). The discrepancy in these findings might be due to differences in age range, sample size and sampling methods. To our knowledge, no study has assessed the nutritional status based on different BMI definitions in Tibetan adolescents aged 12–17 years. Although the proportions differ between studies mentioned above, these data consistently show that there is still a high prevalence of thinness in Tibetan children and adolescents. One reason is the adverse influence of poor socio-economic conditions in Tibet(Reference Harris, Crawford and Yangzom12,Reference Pawson, Huicho and Muro20) , while others have emphasised that a high altitude might lead to delayed growth in children(Reference Dang, Yan and Yamamoto14,Reference Greksa21) . In addition, the economic environment of localities at high altitude is often poor, which can lead to a high prevalence of thinness in children and adolescents(Reference Niermeyer, Andrade Mollinedo and Huicho11).
Irrespective of the different BMI classifications applied in our study, the prevalence of thinness was higher in boys than girls, while the prevalence of overweight was higher in girls than boys. Findings from previous studies are similar to ours(Reference Dong, Zou and Yang2,Reference Gaskin and Walker22) , while some others have shown an opposite trend(Reference Bianba, Yangzong and Gonggalanzi13). The following reasons might explain the sex difference in nutritional status. Compared with girls, boys usually engage in more physical activities (e.g., playing basketball and footballs)(Reference Li, Li and Wang23). The gender difference in nutritional status might also be explained by an earlier onset of sexual maturation among girls, as fat accumulation is more likely to occur in girls after 12 years of age(Reference Dong, Zou and Yang2), and body fat percentage is indeed positively correlated with BMI(Reference Wang, Wang and Liu24).
Although we found no significant age trend in the prevalence of thinness according to the China and IOTF definitions, the prevalence of thinness tended to decrease with increase of age according to the WHO definition. There were no obvious trends with increase of age for the prevalence of overweight and obesity according to the China, IOTF and WHO definitions. A study reported that the prevalence of thinness among Chinese children with ethnic minority aged 7–9 years is highest, according to the China definition, followed by adolescents with ethnic minority aged 16–18 and 13–15 years(Reference Dong, Zou and Yang2). Another study in fifty-eight low- and middle-income countries showed that the prevalence of overweight and obesity among young adolescents aged 12–13 years is higher than those aged 14–15 years according to the IOTF and WHO definitions, but the prevalence of thinness among those aged 12–13 years is lower than those aged 14–15 years(Reference Yang, Bovet and Ma25). The inconsistency of these findings might be explained by differences in race, sample sizes and sampling methods.
We found that several lifestyle factors were associated with thinness, overweight and obesity among Tibetan adolescents. Tibetan adolescents who spent screen time more than 2 h/d had an increased risk of overweight, which is similar to the findings from previous studies(Reference Braithwaite, Stewart and Hancox26,Reference Marshall, Biddle and Gorely27) . In addition, short sleep duration was associated with reduced risk of thinness in our study, and the same result was found in one adult study(Reference Ryu, Kim and Han28). We also found that Tibetan adolescents who consumed fruits less than once per day had an increased risk of overweight. Similar to our finding, a systematic review showed that there was a significantly inverse association between intakes of fruits and vegetables and abdominal obesity among adolescents(Reference Collese, Nascimento-Ferreira and de Moraes29).
The main strength of the current study includes the use of three BMI classifications (China, IOTF and WHO definitions) to estimate the prevalence of thinness, overweight and obesity in Tibetan adolescents, which allows a direct comparison of our findings with those from others. However, the current study has some limitations. Firstly, thinness can only indicate an unhealthy nutritional status(Reference Li, Hu and Zhao30). Further studies with more detailed information of malnutrition status are needed. Secondly, BMI is a crude indicator of nutritional status, and other indicators such as body fat percentage and biochemical indicators should be considered in future studies. Thirdly, the current study used a convenient cluster sampling method, and the representativeness of the data might have been affected. Fourthly, several variables including sleep time, screen time, intakes of fruit, vegetable and meat, water drinking and exercise were self-reported, which might have affected the observed association.
In conclusion, we found the prevalence of overweight and obesity is low among Tibetan adolescents aged 12–17 years, but the prevalence of thinness is generally high, especially among boys. Our findings reinforce evidence suggesting that timely monitoring and improvement of the nutritional status of thinness among Tibetan adolescents are necessary, although the co-occurrence of overweight and obesity also should be paid some attention.
Acknowledgements
Acknowledgements: The authors thank all students and their parents who participated in this survey. Financial support: This work was supported by Cheeloo Medical School, Shandong University. Conflict of interest: The authors declare that they have no competing interests. Authorship: B.X. designed and supervised the study. Y.Z. analysed the data and drafted the manuscript. B.X., C.G.M., M.Z. and J.S. made contributions to interpretation of data and critically revised the manuscript. All authors read and approved the submission of the final manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Committee of Shandong University. Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021000215






