The rapid rise in overweight and obesity rates over recent decades is increasingly recognised as a complex and costly public health problem of global magnitude( Reference Dehghan, Akhtar-Danesh and Merchant 1 – 3 ). The prevalence of childhood and adult obesity in Malta is among the highest worldwide( Reference Finucane, Stevens and Cowan 4 – 6 ). Obesity is a precursor of non-communicable diseases including IHD, cerebrovascular disease and several types of cancer that collectively account for the majority of deaths in Malta( Reference Gatt 7 ). In 2010 over 40 % of a national cohort of 10-year-old children were classified as either overweight or obese according to criteria of the International Obesity Task Force (now known as the World Obesity FederationFootnote †), a substantial increase from the 26 % prevalence measured three years previously( Reference Grech and Farrugia Sant’Angelo 8 , Reference Grech and Farrugia Sant’Angelo 9 ). Other studies using different methods have reported similar findings in younger as well as older Maltese children( Reference Currie, Zanotti and Morgan 10 – 12 ). The economic implications for the national health and social care systems are significant, with estimated annual direct costs attributable to the consequences of overweight and obesity in the population aged 15 years and over of about €20 million in 2008. This included medical expenses such as in-patient stays, day-patient stays and consultations with general practitioners and specialists, but excluded costs related to medication, surgery, ancillary services and loss of income. Assuming no change in the proportion of overweight and obese individuals in the population, the projected cost for 2020 would increase by about €6 million. However, the authors cautioned that increasing overweight and obesity rates in recent years suggest these calculations are likely to grossly underestimate the true cost( Reference Calleja and Gauci 13 ).
In light of this situation, the Maltese government has launched a number of strategy and policy documents outlining targets and measures intended to increase physical activity and improve nutrition across the population( 14 – 18 ). These include a national obesity strategy that outlines a range of possible economic and fiscal measures, targeted multidisciplinary programmes and changes to the environment( 14 ); ongoing education reforms aiming to modify the school nutrition environment and positively affect time allocated to physical activity during or after school hours( 16 , 19 , 20 ); and policies to improve the local physical environment taking into account environmental, economic, social, cultural and infrastructural considerations( 18 ). However, while political commitments to address obesity in Malta seem to heed the call for a shift in emphasis from treatment of already obese children to prevention and policy-level changes, actions promoting major changes to the physical, economic and social environment have not been implemented, with the majority of current measures predominantly focusing on improving consumer knowledge.
The ‘obesogenic’ environment is defined as ‘the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations’. Tackling this obesogenicity requires system-wide environmental interventions that complement educational and behavioural measures in order to create supportive environments( Reference Swinburn, Egger and Raza 21 ). Population-level environmental interventions are cost-effective measures to achieve lasting reductions in obesity because they become incorporated into structures, systems, policies and sociocultural norms( Reference Swinburn, Egger and Raza 21 – Reference Sassi, Cecchini and Lauer 23 ). However, it is likely that strategies to combat obesity will be more effective if they are appropriate to the national context( Reference Knai and McKee 24 , Reference Swinburn, Sacks and Hall 25 ). A recently published framework for monitoring and benchmarking of food environments recommends that an initial country-level contextual analysis be carried out( Reference Swinburn, Sacks and Vandevijvere 26 ) to outline country characteristics and factors influencing food composition or nutrient profiles( Reference Neal, Sacks and Swinburn 27 ), food prices( Reference Lee, Mhurchu and Sacks 28 ), as well as the status of existing government and private-sector policies and actions related to food environments, obesity and non-communicable disease( Reference Sacks, Swinburn and Kraak 29 ). The present paper maps out potential drivers of obesity in Malta and outlines areas where further research would be beneficial.
Methods
We conducted a contextual analysis to explore factors contributing to the establishment of an obesogenic environment in Malta, informed by a review of the literature around obesity, physical activity and nutrition in Malta published between 1990 and 2013. Two electronic databases (MEDLINE and EMBASE) were searched using the following key search terms: ‘Malta’, ‘obesity’, ‘nutrition’, ‘food’ and ‘physical activity’; 109 articles were identified. After reviewing abstracts, eighty-seven papers were rejected and twenty-two full-text articles were retrieved. Additional publications were identified following recommendations by Maltese public health experts; a review of relevant Maltese websites; and thorough hand searching of back issues of the Malta Medical Journal since 1990.
Results are organised and presented using the ANalysis Grid for Elements Linked to Obesity (ANGELO) framework( Reference Swinburn, Egger and Raza 21 ). This diagnostic tool, which has been used to conceptualise the obesogenic environment and prioritise action points for obesity prevention in communities( Reference Simmons, Mavoa and Bell 30 ), outlines two levels of environment: (i) the micro-environment within which individuals typically interact on a daily basis (such as the home, school, workplace, neighbourhood); and (ii) the broader macro-environments which tend to be outside direct individual control. These include large, geographically diffuse sectors such as the education and health systems, government and private sectors, and the food industry. Each environmental level in turn comprises four possible dimensions that potentially affect population-level nutrition and physical activity: (i) the physical dimension describes factors such as urban design, transportation and the home or neighbourhood built environment; (ii) the economic dimension encompasses factors such as income, education and socio-economic status at the micro level; (iii) the policy dimension describes national or regional policies and regulations at the macro level; and (iv) socio-cultural factors refer to the broader context within which individuals live, such as societal norms about nutrition and family behaviour. These four dimensions interact to influence people’s diet and physical activity choices, and are explored in a narrative fashion to illustrate why Malta could be described as an ‘obesogenic’ island in the Mediterranean.
Results
Factors affecting nutrition and physical activity are presented separately below for the macro- and micro-environments.
The macro-environment
Factors affecting nutrition
Historical context and the nutrition transition in Malta
Malta’s small size, colonial heritage, its longstanding cultural and commercial links with and proximity to mainland Europe, and its longstanding dependence on imported foodstuffs have fundamentally conditioned the food system and dietary norms of the Maltese( Reference Gastoni and Atkins 31 ). Tourism, media and the effect of globalisation in the decades since the 1960s have also had an impact on the consumption of convenience and luxury foods( Reference Mizzi 32 ). Thus, despite its central Mediterranean location, the diet prevalent in Malta cannot be said to be truly ‘Mediterranean’( Reference Helsing 33 – Reference Bellizzi 35 ), instead exhibiting ‘…diet and health patterns more typical of Northern Europe than of the Mediterranean’( Reference Serra-Majem, Ferro-Luzzi and Bellizzi 36 ).
Colonial impact
An 1839 British colonial government report described the diet of the Maltese as consisting mainly of bread, seasonal vegetables and occasional fish, with minimal animal produce( 37 ). This is very similar to the traditional Mediterranean diet that has been shown to significantly reduce incidence of CVD( Reference Estruch, Ros and Salas-Salvado 38 ) and which is typically high in olive oil, nut, vegetable, pulses, cereal and fruit intakes with moderate amounts of fish but low meat or dairy product intake( Reference Kushi, Lenart and Willett 39 – Reference Esposito, Ciotola and Giugliano 44 ). Since then, the Maltese economy has progressed from one harnessed to the needs of the British colonial administration to a diversified open-market economy that is mainly export-driven, with an emphasis on manufacturing, financial services and tourism. Following a process of trade liberalisation initiated in 1989( Reference Mizzi 32 ) which facilitated the fast-food industry’s penetration into the local market, Malta joined the EU in 2004 and is classified as a high-income country by the World Bank.
The nutrition transition
Table 1 shows that between 1961 and 2010, overall energy availability (in kcal) increased by approximately 21 %, supporting claims that daily energy intake in Malta increased significantly during the latter half of the 20th century even as consumption of fatty foods exceeded that consumed in Northern European countries( Reference Schmidhuber 45 ). It is likely that the historical influences outlined above, systematic changes to global food production and distribution systems, improving economic conditions and a dependence on foreign imports have consolidated the shift away from the traditional Mediterranean diet( Reference Tourlouki, Matalas and Bountziouka 46 , Reference Piscopo 47 ) and led to the adoption of a more ‘Westernised’ diet high in refined carbohydrates, meat, SFA and salt( Reference Bellizzi 34 , Reference Bellizzi 35 , Reference Tessier and Gerber 48 ). Thus, a century-and-a-half later, a 1986 WHO report portrayed the Maltese diet as an unhealthy one rich in fats and sugar and low in fibre, designating the Maltese as a high-risk group for non-communicable disease( 49 ). An increase in the variety of available foods, all-year-round availability of food items that were previously only available during the local growing season and increased accessibility of energy-dense food products( 16 ) in a cultural environment where food occupies a central role have had predictable results. Results from a food consumption study conducted in 2010 indicated that overall vegetable and fruit intake is low, while pasta, bread and meat intakes are substantial( 50 ). Similarly, previous research on Maltese children’s diet showed that intake of carbohydrate-based foods such as pasta, pizza and fast-food-style meals is pervasive, as is consumption of breakfast cereals and soft drinks. On the other hand, very few Maltese children consume sufficient fruit and vegetables( Reference Piscopo 51 ). The Health Behaviour in School-aged Children (HBSC) studies showed that, between 2002 and 2010, self-reported daily fruit and vegetable consumption has generally decreased while daily soft drink consumption has increased among 11-, 13- and 15-year-olds. However, only reductions in fruit consumption among 11-year-old girls and 15-year-old boys were significant at the 95 % confidence level (17 % reduction, z=2·57, P=0·01; and 12 % reduction, z=2·06, P=0·04, respectively)( 12 , Reference Currie, Roberts and Morgan 52 , 53 ).
Table 1 Major sources of dietary energy (kcal)Footnote *, 1961–2010, Malta (from FAOSTAT(55))
To convert kcal to kJ, multiply kcal by 4·184
* Five-year moving average.
Household expenditure data might suggest a similar trend for the general population. Figure 1 indicates that domestic (i.e. excluding tourist) expenditure on food relative to total domestic expenditure has decreased by about 25 % since 1995, while Fig. 2 illustrates domestic expenditure on different food categories as a proportion of total expenditure on food and beverages. Expenditure on meat has since risen slowly but steadily since 1995, in contrast to a gradual decline in expenditure on bread and cereals. Spending on confectionery and sugary products has increased consistently in recent years, even as expenditure on vegetables has decreased.
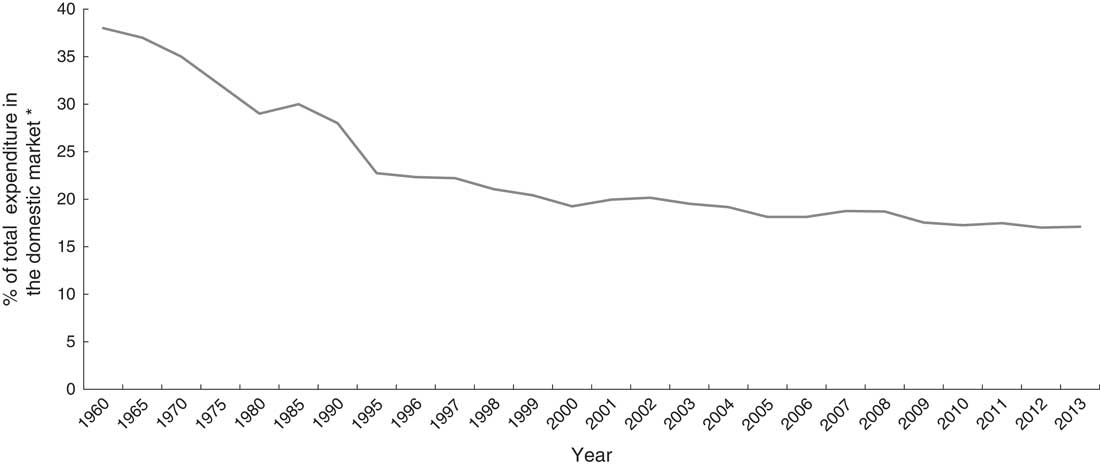
Fig. 1 Expenditure on foods and non-alcoholic beverages as a percentage of total household expenditure*, 1960–2013, Malta (from household expenditure data, Malta (1960–2013) supplied by National Statistics Office, Valletta, personal communication, 2014). *Excludes expenditure by tourists
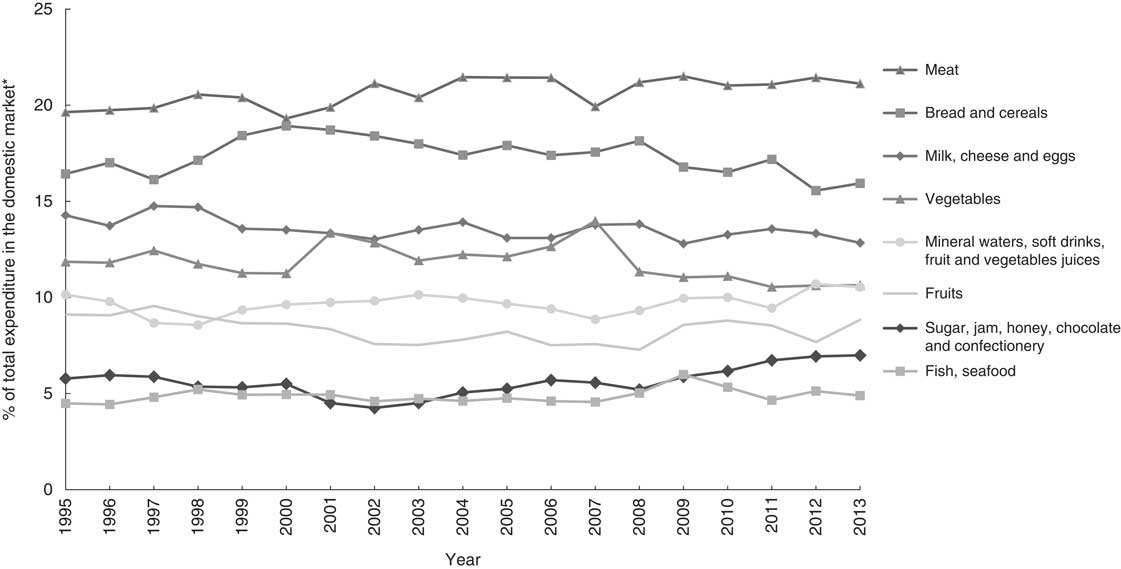
Fig. 2 Expenditure on selected food items as a percentage of total household expenditure on foods and non-alcoholic beverages*, 1995–2013, Malta (from household expenditure data, Malta (1960–2013) supplied by National Statistics Office, Valletta, personal communication, 2014). *Excludes expenditure by tourists
Although food balance sheetFootnote * data should be interpreted with caution considering the proportionately large number of tourists visiting Malta compared with the permanent resident population, data in Fig. 3 show a steady increase in the availability of meat and sugar/confectionery. Vegetable, fruit and fish availability have risen slightly, whereas availability of dairy products has remained mostly stable. At the same time, there has been a decline in availability of cereals. Supplies of both protein and fat have increased steadily by 38·8 % and 26·8 %, respectively, since the 1960s (Fig. 4(a) and (b)), with a proportionally greater share derived from animal products.
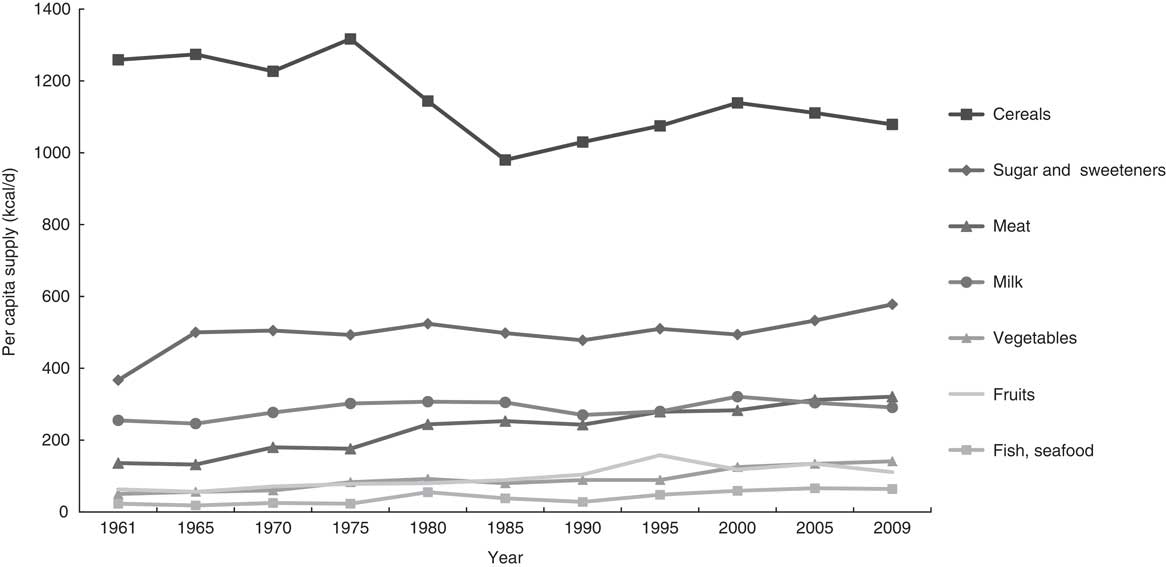
Fig. 3 Per capita supply of selected food categories (kcal/d), 1961–2009, Malta (from FAOSTAT(55)); to convert kcal to kJ, multiply kcal by 4·184
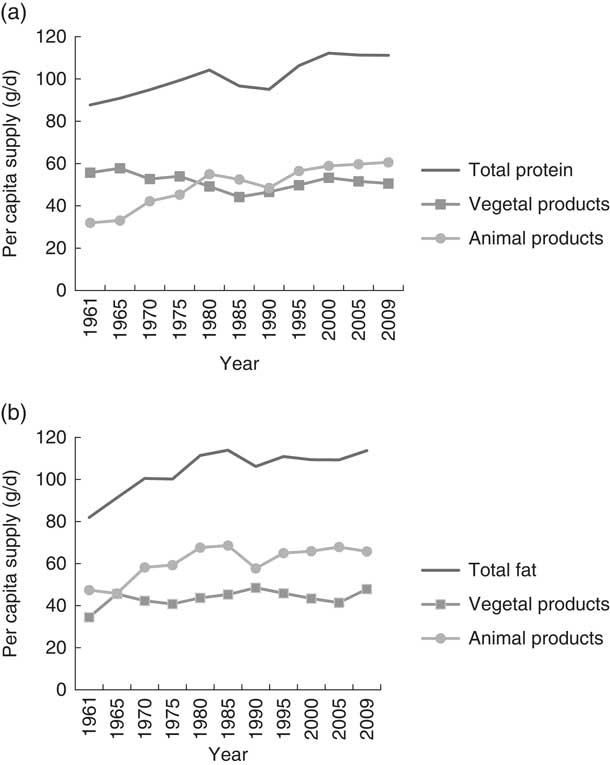
Fig. 4 Per capita supply of (a) protein (g/d) and (b) fat (g/d), 1961–2009, Malta (from FAOSTAT(55))
Other socio-cultural aspects
Malta underwent a sudden shift from food shortage – particularly during the Second World War when meat and foods rich in fats and sugar were practically unobtainable – to one of affluence, while at the same time the cultural identity shifted from Mediterranean to Anglo-Saxon( Reference Tessier and Gerber 48 ). Large numbers of Maltese workers who emigrated during the 1950s and 1960s returned decades later with Western food preferences established during their stay in host countries such as Australia, Canada, the USA and the UK( Reference Formosa, Savona-Ventura and Mandy 54 ). In addition, for many years during and after the Second World War, Malta was greatly dependent on foreign monetary and commodity aid, including imported foods. This may have negatively impacted the type and quality of food available at the time and encouraged the establishment of unhealthy dietary practices. The Maltese consume large amounts of cheddar cheese, sugar, corned beef and condensed milk – unusual in the Mediterranean region( Reference Mizzi 32 ). Although not a producer of sugar, Malta’s per capita supply of sugar is the highest in the EU (Fig. 5) and among the highest in the world( 55 ), indicating that sugar could be a major source of energy in the Maltese diet( Reference Bellizzi 35 ).
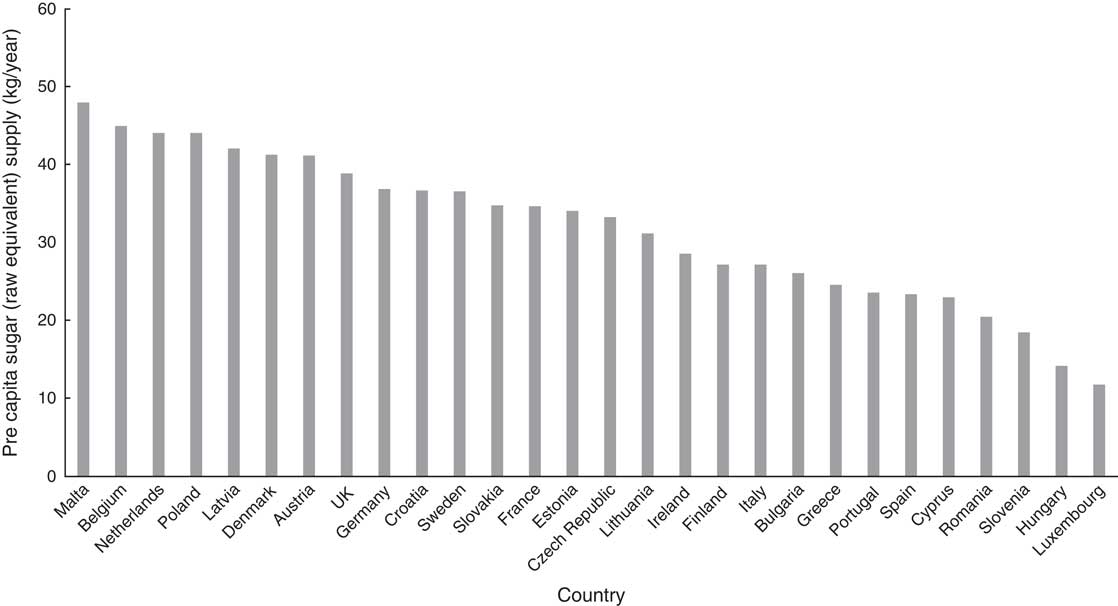
Fig. 5 Per capita supply of sugar (raw equivalent) to EU-28 countries, 2011 (from FAOSTAT(55))
Thus, in spite of increasing awareness of what constitutes a healthy diet, such a ‘socially learned’ attitude towards food might have been perpetuated from one generation to the next( Reference Fieldhouse 56 ) and remains the norm today. Additionally, the Maltese embrace a number of obesogenic cultural norms, such as a marked preference for large portion sizes( 50 ), a tendency to eat out with family( Reference Piscopo 51 , Reference Costa 57 ) and frequent engagement in religious, public or family-oriented feasts and celebrations that are traditionally characterised by an abundance of food. Village ‘festas’ are distinctive cultural traditions that have been commercialised by the food industry, with a plethora of Maltese and foreign fast foods such as hot dogs, burgers, ice cream, kebabs, chips, nougat, fried pastry and other foods rich in saturated fats and sugars( Reference Formosa, Savona-Ventura and Mandy 54 ).
Food advertising aimed at children
Television (TV) viewing reduces energy expenditure through displacement of physical activity, is associated with increased energy intake from snacking and entails exposure to food advertising( Reference Lissner, Lanfer and Gwozdz 58 ). Local research suggests that a majority of primary-school children regularly exert pressure on parents to purchase foods advertised on TV( Reference Costa 57 ). The introduction of cable TV to the islands in 1991 increased the selection of local and foreign (Italian, British and American) programming and advertising to children( Reference Piscopo 51 ). Studies have suggested that food marketing targeting children is pervasive in Malta, particularly through point-collection schemes, sponsorship of school events and children’s TV programmes, distribution of free materials in schools, offering ‘free’ gifts with fast-food meals and TV food advertising( Reference Fenech 59 ). A content analysis of food advertising on Maltese TV stations during children’s viewing hours revealed systematic promotion of fast foods, breakfast cereals, fruit squash mixers and confectionery items( Reference Fenech 60 ).
Factors affecting physical activity
Topopography and climate
Malta is one of the most densely populated countries in the world( 61 ) and this has been reflected in significantly changing land use over time. Currently, there is a relatively high proportion of urban/industrial land cover (29·7 % of the total land area in 2008, up from 21·5 % in 2000). This represents a rate of development about three times the EU average( Reference Gatt 7 ); 51 % of the Maltese islands is devoted to agricultural use and the remaining 18 % is covered by natural vegetation( 62 ). It may be argued that excessive land development has reduced the availability of outdoor spaces where children can be active. Certainly, population participation in sports remains alarmingly low( 17 ) with about 72 % of the adult population characterised as being physically inactive in a recent international study( Reference Hallal, Andersen and Bull 63 ). Additionally, Malta’s typical Mediterranean climate is characterised by hot, dry summers and mild, rainy winters( 61 ). Temperatures in summer can exceed 35°C, with high levels of humidity often making the outdoors uncomfortable. High temperatures are associated with reduced physical activity( Reference Bosdriesz, Witvliet and Visscher 64 ), hence climate may also contribute to the low levels of physical activity observed.
Transport preferences
In spite of a fiscal regime imposing relatively high taxation on car registration and purchase of polluting cars together with high fuel costs, Malta has one of the highest per capita car ownership levels in the EU: 607 cars per 1000 inhabitants in 2009( 65 ). Moreover, 19·6 % of households own three cars or more( 66 ). In spite of Malta’s small size and lack of significant inter-city distances that in other countries account for a large proportion of kilometres travelled per passenger, data indicate that three-quarters (74·6 %) of all journeys are undertaken using private passenger cars( 66 ). This has been attributed to a ‘car culture’ which ‘embraces and aspires to car ownership’; cars offer greater freedom than public transport with the added bonus of being a status symbol. High car usage and the lack of efficient public transport options have fostered the perception that there is no choice in transport, a mindset which is exacerbated by social status, peer pressure and culture( 67 ). Malta’s high motor vehicle density has exerted pressure on national transport infrastructure leading to significant capacity problems and traffic bottlenecks outside peak hours that further incapacitate the public transport system. The Public Transport Reform launched in 2011 was intended to kick-start a shift towards public transport use. However the reform did not achieve the desired effect, culminating in the transport system’s re-nationalisation in December 2013( Reference Sansone 68 ). Concurrently, levels of both walking and cycling in Malta are low( 69 ). This has been attributed to a range of factors including Malta’s hilly topography and subtropical climate, poor road conditions coupled with a lack of cycling infrastructure, road congestion, air and noise pollution, and high levels of perceived road danger( 66 , 67 ).
Taxation and subsidies
Governmental efforts to exert control on supply and availability of unhealthy food products have been rendered mostly ineffective by trade agreements, common markets and transnational marketing of food products and food chains( 16 ). However, the feasibility of fiscal incentives to encourage healthy nutrition, increase the availability of healthy food outlets and restrict outlets selling fast foods is currently being explored by the Maltese government( 14 ). Malta is also a signatory to the European Charter on Counteracting Obesity( 70 ), which emphasised the importance of subsidies, reformulation and marketing restrictions.
The micro-environment
Factors affecting nutrition
Children tend to have limited autonomy in their food intake and physical activity levels, with the majority of their choices determined by their parents and immediate family, and to a lesser extent their peers( Reference Scaglioni, Arrizza and Vecchi 71 ). A study on Maltese 8–10-year-olds showed that children most liked eating pasta, pizza, chips, fruit and burgers, while their least liked foods were vegetables, meat, fish, soup and fruit( Reference Costa 57 ). They are also heavy consumers of soft drinks( Reference Piscopo 51 ).
Community food environment
Although self-sufficient in the production of most fresh vegetables, milk and eggs, Malta is partially dependent on imports of meat and potatoes and completely dependent on imports of grain, flour and sugar. About 71 % of the island’s food requirements are imported( 55 , 65 ) and this may have shaped Maltese eating habits in a process of food acculturation( Reference Fieldhouse 56 ). Limited research on factors influencing the broader food environment in Malta exists( Reference Gastoni and Atkins 31 , Reference Mizzi 32 ). There have been informal calls for action to limit proliferation of fast-food establishments or street hawkers outside schools, often frequented by children and parents immediately after school hours( 72 ). Small grocery stores offering fresh fruit and vegetable produce in some villages have gradually disappeared, as customers were attracted by competitive prices and wider choices offered by larger outlets. However, roving vendors selling fruit and vegetables are popular in many villages, possibly enhancing access to fresh foods for certain households( 16 ). A more recent phenomenon is the presence of mobile vendors selling doughnuts, ice cream and sweets – often directly targeting children by parking in the vicinity of schools – announcing their presence with loud jingles or catchy phrases, which have proved to be extremely popular( 72 ). Mobile vendors have been shown to impact children’s snacking opportunities( 53 ). In many villages, such food outlets provide a convenient alternative to cooking fresh meals. Figure 6 shows a rapid increase in the overall number of trading licences issued to confectionery stores, ‘pastizzeria’ outlets (stores selling cheap pastry products high in fat and sugar content and baked on-site, such as cheesecakes or sausage rolls) and – more recently – to mobile vendors selling doughnuts.
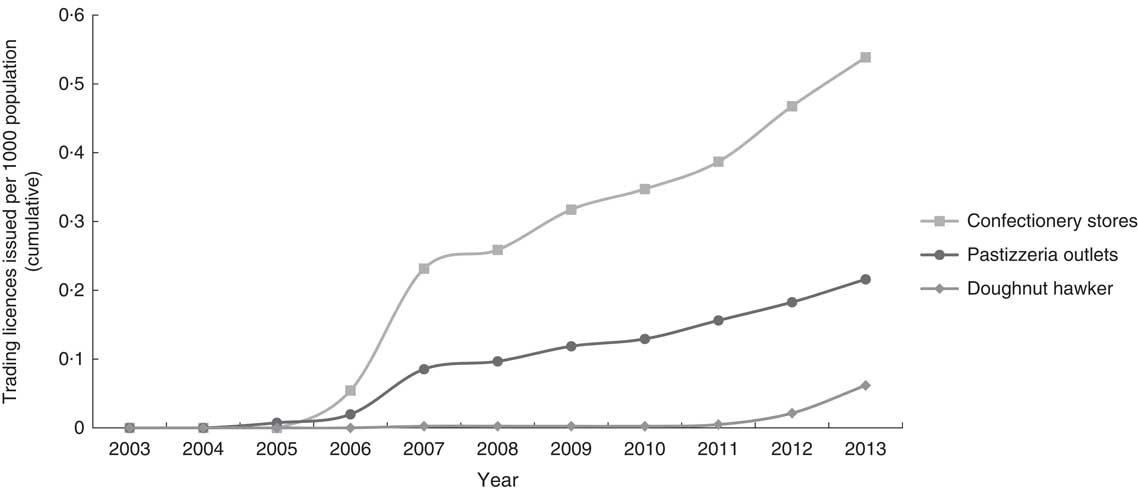
Fig. 6 New trading licences* per 1000 population issued between 2003 and 2013 for selected food outlets/mobile vendors, Malta (cumulative; from applications for food trading licenses (2003–2013) supplied by Environmental Health Directorate, Msida, Malta, personal communication, 2014). *New trading licences allowing food to be sold on-site, issued by the Environmental Health Directorate between 01/01/2003 and 31/12/2013 (showing vendors operational as of 31/01/2014)
The introduction and proliferation of major fast-food chain outlets in Malta since 1995 has been followed by heavy marketing in the Maltese mass media( Reference Costa 57 , Reference Marmara 60 ). It is not unusual for children to be taken to such outlets as a treat for good behaviour( Reference Piscopo 51 ).
Educational settings
The 2007 Healthy Eating and Lifestyle Plan (HELP) document outlines steps to be taken in schools to promote healthy lifestyles for Maltese students, providing voluntary guidelines to a health-promoting school environment and curriculum. It recommends regulation of foods sold in state school canteens and/or vending machines, as well as school policies to control content of students’ packed lunches (school meals are not provided to schoolchildren in Malta)( 20 ). It is currently being revised prior to its introduction as standard policy in state schools. However, HELP cannot exert control over the retail environment outside schools, where children often purchase snacks( Reference Costa 57 ). Other efforts to improve schoolchildren’s nutrition within the school setting include the provision of free milk daily to state primary-school students; the introduction of a ‘Breakfast Club’ offering a free healthy breakfast to children of working parents who attend state schools; and a EU co-funded ‘School Fruit and Vegetable Scheme’ where a portion of pre-packed fresh fruit or vegetable is given weekly to all primary-school children in Malta( 73 ). The 1999 Maltese National Minimum Curriculum stipulated lessons on nutrition and specifies a number of hours of Physical Education weekly, yet these are often sacrificed in favour of other academic subjects deemed to be of greater priority( 74 ). Currently, Physical Education policies are not consistently enforced across schools and these activities are timetabled for a range from 60 min/week in certain church schools to more than 120 min/week in independent schools( 75 ). Starting in September 2014, a compulsory subject (Physical Health Education) comprising elements of Physical Education and Home Economics was introduced to all primary- and secondary-school students, based on the rationale that compulsory certification might improve participation rates and decrease physical inactivity in schools( 19 ).
Social and educational status
Parental social and educational statuses are strongly associated with obesity( Reference Classen and Hokayem 76 – Reference Singh, Siahpush and Kogan 79 ). The 2005/2006 WHO HBSC survey( 12 ) demonstrated an inverse association between family affluence and self-reported overweight and obesity among European children. An inverse relationship between educational level and obesity in Malta was shown in the 2008 Health Interview Survey and other studies( Reference Borrelli, Giuffre and Buono 5 , 80 ). Economic considerations may impact familial food choices particularly during times of financial hardship: one consequence of economic insecurity as a result of the recent financial crisis is the relatively high proportion of Maltese having part-time as well as full-time jobs( 81 ). This may leave less time for parents to cook healthy food or accompany children outdoors, potentially leading to unhealthy food choices and lack of exercise opportunities( Reference Will, Zeeb and Baune 82 ).
Home food environment
Eating behaviours and physical activity of Maltese adolescents are particularly variable and tend to be influenced by both individual and environmental factors( Reference Grundy 83 , Reference Selassie and Sinha 84 ), as well as familial patterns of overweight( Reference Birch and Davison 85 ). Parental overweight status is itself a strong predictive risk factor for childhood obesity particularly in deprived families, whereas parental leanness seems to confer protection against development of childhood overweight regardless of family socio-economic status( Reference Parsons, Power and Logan 2 , Reference Semmler, Ashcroft and van Jaarsveld 86 ). This has significant implications for Maltese children given the large proportion of overweight and obese adults in the population. Little is known about consumption in the home; however, it has been suggested that snacks are eaten in addition to, rather than displacing, set meals in Malta, resulting in a high frequency and level of food consumption( Reference Piscopo 51 ).
Factors affecting physical activity
We found little information on policies or interventions that might influence physical activity levels of Maltese children in the community and at home; the majority of studies and policies identified in the literature review focused on the food environment.
Physical activity in the community and at home
Gross Domestic Product and public sector expenditure on health have been positively associated with increased leisure-time physical activity( Reference Van Tuyckom 87 ). Government investment in recreational and sport facilities in Malta has gained momentum with a number of sports facilities inaugurated over the past two decades. Local sporting events are often subsidised by the government and access to fitness facilities in state-run leisure centres is heavily subsidised in a bid to encourage attendance( 17 ). Additionally, outdoor fitness centres are being created to provide space for physical activity (C Gauci, personal communication, 5 June 2014). Although studies on the extent of sedentariness in Maltese children are lacking, the highly prevalent use of TV and gaming technology as ‘babysitting’ devices has been identified as a target for action in the Healthy Weight for Life Strategy( 14 ).
Discussion
The health and economic costs of excess weight in Malta continue to rise, leading to a situation where the morbidity and mortality burden of obesity-related disease such as diabetes and CVD are higher than the European average( Reference Gatt 7 , 16 , Reference Formosa, Savona-Ventura and Mandy 54 ). This may have been driven by a strongly obesogenic environment, with multiple drivers across different settings, sectors and the life course of unhealthy eating and low levels of physical activity. However, data characterising the links between these various environmental components and childhood obesity are currently lacking or difficult to access. There is a clear need for an integrated whole-system approach that considers both health and non-health sectors (including trade, agriculture, transport and urban planning) in order to create synergies that support sustainability of actions and policies( Reference Gortmaker, Swinburn and Levy 88 ). The role of public health action should be to restore a level playing field in which physical, socio-cultural, economic and policy drivers are shifted to create healthy defaults, making healthier choices the easiest choices( Reference Radnitz, Loeb and DiMatteo 89 ). For example, the burgeoning agro-tourism sector in the Maltese islands might be encouraged to capitalise on its ‘healthy lifestyle’ message by offering cycling tours, which in turn would benefit from construction of cycle lanes between areas of interest. Encouraging active travel through provision of appropriate infrastructure would also benefit local mobility, thus creating a self-sustaining system that promotes an active lifestyle for all. Such multi-component, community-based initiatives have been reasonably successful in preventing obesity in children( Reference Tessier and Gerber 48 , Reference Decelis, Fox and Jago 90 , Reference Bemelmans, Wijnhoven and Verschuuren 91 ) and provide best-practice evidence for interventions that can be applied to Malta. Crucially, they are aimed both at changing children’s behaviour directly and at altering their environment. We have applied the ANGELO framework to structure discussion of obesogenic factors in the Maltese environment emerging from our review.
Economic factors
Figures 1 to 4 indicate that food availability in Malta is increasing slowly but steadily even as proportional domestic expenditure on food decreases; however, this may simply reflect improving income levels in the general population( Reference Knai and McKee 24 ). As yet, no nationally representative food consumption data are available for Malta, making it difficult to derive conclusions about proportional expenditure or nutritional habits at population level. A qualitative food consumption survey conducted in 2010 does not provide information on actual quantities of food consumed. Food balance sheet data are based on food import, export and production data, and hence should be interpreted with caution in view of potential seasonal increases in food supply in response to tourist demand. Establishing a national survey mechanism to collect trend data on food consumption (including children) and food pricing would enhance our knowledge of food habits and the influence of prices on food consumption, enabling the development of evidence-based nutrition policy recommendations targeting specific sections of the population. Other economic considerations operate at the micro level. For example, Maltese schoolchildren are often given money to purchase their own snacks on school days( Reference Costa 57 ), leading to potentially unhealthy snack purchases dependent on cost, availability and taste. Family lifestyle and socio-economic status are also likely to influence accessibility, variety and quality of food eaten by children, as well as their access to sports and recreational facilities (e.g. through parental willingness to pay for sports equipment or club membership fees).
Physical factors
While schools remain a key setting for provision of structured physical activity to Maltese children, actual time spent being physically active during a physical education lesson is limited to a small fraction of the total time allocated( 74 ). Regular auditing of actual time spent being physically active should be carried out in all schools on a regular basis and ideally more sessions allocated for physical activity( Reference Waters, de Silva-Sanigorski and Hall 92 ). The introduction of a new compulsory subject combining healthy eating, physical activity and body image in secondary-school curricula may help foster healthy dietary habits and enhance overall levels of physical activity, and is a recommended component of best-practice interventions( Reference Waters, de Silva-Sanigorski and Hall 92 ). This will complement an existing scheme that aims to shape children’s food preferences and promote sustainable consumption of fruit and vegetables through once-weekly distribution of free fruit and vegetables portions in primary schools( 73 ).
At a population level, it remains to be seen whether the desired shift away from car usage towards public transport can be achieved. Furthermore, we did not find evidence of policies aiming to encourage alternative forms of urban mobility (such as through the provision of bicycle lanes) or to increase levels of physical activity in the community or at home. Further studies exploring the feasibility and effectiveness of interventions in these areas would be useful.
Socio-cultural factors
Eating habits and food preferences are established at a young age and maintained into adolescence( Reference Birch and Fisher 93 , Reference Wang, Bentley and Zhai 94 ). Food norms are passed on across generations through a process of socialisation, moulding children’s preferences( Reference Fieldhouse 56 ). In turn, preferences may influence intake either directly through children’s requests to adult food providers or indirectly through adults’ fulfilment of perceived children’s preferences. Best-practice recommendations to create an environment and culture that support children eating nutritious foods and being active from an early age include the provision of support to school staff for the implementation of health-promotion strategies and activities and the engagement of parents to offer complementary action within the home (e.g. discourage screen-based activities)( Reference Tessier and Gerber 95 ).
Systematic advertising of sugar-sweetened beverages may help explain Maltese children’s preference for soft drinks over water( Reference Piscopo 51 ) and the high rate of soft drink consumption in Malta (second only to Mexico( 96 )); however, there is a lack of evidence to support such conjectures. An analysis of online media advertising targeted at children has not yet been carried out in Malta. Additionally, a comprehensive content analysis of TV and other audiovisual media advertising that expands upon the single dissertation study tackling the topic( Reference Marmara 60 ) would help formulate targeted policy responses to inappropriate advertising to children. Both multifaceted school-based programmes with active physical education components as described above, and initiatives to reduce TV advertising of high-fat and/or high-sugar foods and drinks to children, have been found to be highly cost-effective interventions( Reference Haby, Vos and Carter 97 ). At the same time, fast-food outlets continue to proliferate, advertise and innovate in response to consumer demand( 98 ), further compounding the change in nutrition habits. Although ‘pastizzerias’ and confectionery stores have been around for decades, could their recent apparent proliferation be due to changing consumer preferences, followed by a market response to demand? For example, children with working mothers may be more likely to watch more TV and eat prepared food than children with mothers who do not work outside the home or to stop at a junk-food outlet on their way to private tuition lessons after school( Reference Piscopo 51 ). It is difficult to clarify the links between the evolving food environment, nutritional and physical activity habits and their impact on obesity rates when baseline quantitative data are lacking. Although the evidence base on associations between neighbourhood environment and weight status is mixed( Reference Tourlouki, Matalas and Bountziouka 46 , Reference Bennie, Chau and van der Ploeg 99 ), local research on the potential impact of neighbourhood built and food environments on lifestyle might open up alternative avenues for policy makers in Malta to explore. Furthermore, Malta is visited by more than a million tourists annually( 61 ) adding yet another layer to this complex issue. It may be the case that tourism has facilitated the assimilation of non-native foods, either by mere exposure to discourse around non-Maltese cuisines or by actual provision of such cuisine in local catering establishments( Reference Piscopo 51 ). Working with industry to encourage reformulation of food – and limit portion sizes – served at catering establishments may be an integral component of an overall strategy seeking to reduce food intake at population level.
Policy factors
The policy environment at both macro and micro levels influences behaviour. Thus informal household rules regulating time spent watching TV, playing video games or other sedentary activities, and rules around food such as eating meals together as a family or limiting snacks, may critically shape children’s attitudes towards food and physical activity levels through their lives( Reference Harrison, Bost and McBride 100 ). More broadly, state-imposed regulations around food labelling and advertising aimed at children may directly or indirectly impact children’s risk of overweight and obesity( Reference Cecchini, Sassi and Lauer 22 ). Currently no national standards on labelling of food items to facilitate healthy food choice exist, although the National Obesity Strategy suggests a need for such standards and EU legislation entered into application in December 2014( 101 ). Additionally, there has been little in the way of policy response to reduce the impact of advertising on children( 14 ).
Conclusion
Many aspects of the physical, social, economic and cultural environments in Malta favour a positive energy balance, characterised by limited infrastructure for active living combined with an energy-dense food supply. Alleviating the future health and economic burden of obesity-related disease will require a deeper understanding of the ways in which Malta’s geopolitical background, cultural identity, physical environment and other drivers of obesity have changed over time. The collection of trend data related to food consumption, physical activity and changes to the built environment will enable the strength of interactions between these drivers to be quantified and appropriate countermeasures to be developed.
Acknowledgements
Acknowledgements: The authors would like to thank Ms Ketevan Glonti and Dr Julian Mamo for their advice during the writing of this article. Financial support: This work was supported by the Malta Government Scholarship Scheme. The Malta Government Scholarship Scheme had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: D.C. contributed to formulating the research question, designing the study, conducting the literature search, analysing the data and writing the article. C.K. and H.R. contributed to formulating the research question and reviewing the article. Ethics of human subject participation: Not applicable.












