Dyslipidaemia is a well-known risk factors for CVD, CHD, type 2 diabetes and stroke(Reference White, Swerdlow and Preiss1–Reference Glasser, Mosher and Howard4). The prevalence of dyslipidaemia is increasing worldwide. According to the WHO, the prevalence of dyslipidaemia in adults is 36·7% in Western Pacific, 53·7% in Europe and 53·8 % in the USA(5). In Korea, the national survey data showed that 38·4% of adults over 20 years old had a prevalence of dyslipidaemia(6).
Dietary patterns are associated with blood lipids. The studies on the association between plant-based diets such as vegetarian diets or vegan and blood lipid profiles showed mixed results(Reference Wang, Zheng and Yang7–Reference Zhang, Wang and Chen9). Vegetarian diets exclude animal foods and recommend plant foods. However, not all plant foods are healthy. For example, refined grains, sugar and sweets, and sugar-sweetened beverages are not beneficial for health outcomes(Reference Huang, Huang and Tian10–Reference Stanhope12). Plant-based diet indices take into account the intake of plant and animal foods with consideration of the quality of plant foods. Recent studies using plant-based diet indices have shown that the plant-based diet can play an important role in reducing the risk of metabolic diseases such as CVD, type 2 diabetes and obesity(Reference Satija, Malik and Rimm13–Reference Satija, Bhupathiraju and Rimm15). Although the associations between different types of plant-based diets and various diseases have been investigated in Western populations(Reference Satija, Bhupathiraju and Spiegelman14–Reference Zamani, Daneshzad and Siassi16), the studies on association of plant-based diets with diseases are still lacking in Asian population. Asian populations may have different dietary patterns and metabolic responses compared with Western population(Reference Park, Murphy and Wilkens17,Reference Micha, Khatibzadeh and Shi18) . In particular, habitual diet of Koreans is mainly composed of various plant foods such as grains and vegetables(Reference Kim, Ha and Choi19). Thus, more comprehensive examinations of plant-based diets are needed to understand if plant-based diets are related to the dyslipidaemia in Asian populations who habitually consume relatively high amount of plant foods, and if the healthfulness or quality of plant foods is associated with the dyslipidaemia. In this context, the purpose of this study was to investigate the association between the healthiness of plant-based diets and dyslipidaemia using data from the nationally representative sample of South Korean adults.
Methods
Study population
This study was based on the fifth (2012), sixth (2013–2015) and seventh cycles (2016) of the Korea National Health and Nutrition Examination Survey. The Korea National Health and Nutrition Examination Survey, conducted by the Korea Centers for Disease Control and Prevention, is an annual cross-sectional survey which assesses diet and health of the Korean population(20–22). The Korea National Health and Nutrition Examination Survey is a clustered, multistage and stratified, sampling design. Written informed consent was obtained from all participants. Among 30 709 individuals ≥19 years (6293 in 2012, 6113 in 2013, 5976 in 2014, 5945 in 2015 and 6382 in 2016), we excluded the following individuals: 13 158 who did not answer FFQ; 555 extraordinary energy intake (<2092 kJ/d or >16736 kJ/d in men or >14644 kJ/d in women); 482 CVD or cancer; 2347 with missing data on dyslipidaemia components or covariates. A total of 14 167 Korean adults (5417 men and 8750 women) were included for the analyses. The study was approved by the Institutional Review Board of Korea Centers for Disease Control and Prevention.
Plant-based diet score
Participants completed a validated 109-item semi-quantitative FFQ to assess participants’ usual dietary intakes over the previous year(Reference Kim, Song and Lee23). Participants were asked to report the frequency with a standard portion size to calculate the average food consumption per day. Nutrient intakes were calculated by multiplying the amount of food consumed and nutrient composition of each food item using a Korean food composition table(24).
For assessing the quality of plant-based diets, we created the plant-based diet index (PDI), healthful plant-based diet index (hPDI) and unhealthful plant-based diet index (uPDI). The detailed procedure was modified from the original plant-based diet indices used in the prior studies(Reference Satija, Bhupathiraju and Spiegelman14,Reference Satija, Bhupathiraju and Rimm15) . Briefly, each food item was categorised into eighteen food groups based on nutrient and culinary similarities within the larger categories of healthy plant foods, less healthy plant foods and animal foods. Plant foods were distinguished between healthy and less healthy plant foods based on the associations between food items and health outcomes (CVD and type 2 diabetes or their intermediate conditions) reported in the literature(Reference Satija, Bhupathiraju and Spiegelman14,Reference Satija, Bhupathiraju and Rimm15) . Finally, food groups were classified as healthy plant foods (i.e. whole grains, fruit, vegetables, nuts, legumes, tea and coffee), less healthy plant foods (i.e. fruit juices, refined grains, potatoes, sugar-sweetened beverages, sweets and desserts, salty foods) and animal foods (i.e. animal fat, dairy, egg, fish or seafood, meat, miscellaneous animal foods) (online Supplementary Table S1). We considered salty foods (i.e. kimchi and other pickled vegetables) as less healthy plant foods due to high Na content(Reference Kim, Kim and Shin25). We did not include vegetable oil food group, which was included in the original plant-based diet indices (Reference Satija, Bhupathiraju and Spiegelman14,Reference Satija, Bhupathiraju and Rimm15) because the FFQ did not assess the consumption of oils. For complex dishes, some dishes were deconstructed into individual foods, for example, the consumption of sugar or cream added in the coffee was asked separately from the coffee, whereas other dishes (e.g. pizza, hamburger/sandwich, dumplings) were individually identified in the questionnaire.
Next, we calculated energy-adjusted consumption of each of the eighteen food groups using the nutrient density and divided their consumption into quintiles(Reference Hu, Stampfer and Rimm26). In all plant-based diet indices, animal foods were reversely scored. For the PDI, all plant food groups (regardless of healthfulness) were positively scored. For instance, participants in the highest quintile of vegetable consumption received a score of 5, whereas those in the lowest quintile received a score of 1 (positively scored). Conversely, participants in the highest quintile of meat consumption received a score of 1, whereas those in the lowest quintile received a score of 5 (reverse scored). For the hPDI, only healthy plant foods received positive scores, whereas less healthy plant foods received reverse scores. For the uPDI, only less healthy plant foods received positive scores, and healthy plant foods received reverse scores. Therefore, the higher score of hPDI represents high consumption of healthy plant foods and lower animal foods, and the higher score of uPDI represents higher consumption of less healthy plant foods and lower animal foods.
Measurements
Trained researchers measured waist circumference, height and weight during a health examination. Waist circumference was measured to the nearest 0·1 cm at the narrowest point between the lowest rib and the uppermost lateral border of the right iliac crest. BMI was calculated as weight (kg) divided by height squared (m2). Blood samples were collected after an overnight fast, and all biochemical analyses were conducted within 2 h of blood sampling. TAG, total cholesterol (TC), HDL-cholesterol and LDL-cholesterol were measured by enzymatically (Hitachi) in a central, certified laboratory(Reference Kwon, Lee and Kang27). If TAG is less than 400 mg/dl, LDL-cholesterol was calculated using the Friedewald formula(Reference Roberts28).
Definition of dyslipidaemia
The diagnostic criteria for dyslipidaemia include the presence of one or more of following(Reference Rhee, Kim and Kim29): (1) hypertriacylglycerolaemia as serum TAG concentration ≥200 mg/dl; (2) hypercholesterolaemia as TC ≥ 240 mg/dl; (3) low HDL-cholesterol as serum HDL-cholesterol concentration <40 mg/dl in men and HDL-cholesterol concentration <50 mg/dl in women; (4) high LDL-cholesterol as LDL-cholesterol concentration ≥160 mg/dl; (5) use of anti-hyperlipidaemic agent; (6) high non-HDL-cholesterol was diagnosed as non-HDL-cholesterol concentration ≥160 mg/dl.
Covariates
Participants completed a self-administered questionnaire which asked about socio-demographic characteristics (age, sex, education, income) and health behaviours (smoking status, alcohol consumption, physical activity). We categorised education as three groups: ≤6 years (elementary school level), 7–12 years (middle or high school level) and >12 years (college level). Income was categorised into three groups: low (the first quartile), medium (the second and the third quartile) and high (the fourth quartile). Smoking status was categorised as non-smokers, former smokers or current smokers. Alcohol intake during the past year was classified as never drinkers, moderate drinkers (<2 times/week) and heavy drinkers (≥2 times/week). Participants were considered to be physically active if they reported hard exercise for ≥20 min at a time ≥5 d per week, moderate exercise for ≥30 min at a time ≥5 d per week or walking for ≥30 min at a time ≥5 d per week. Hard exercise includes activities such as running, hiking, (mountain) climbing, basketball, swimming or badminton, and moderate exercise includes activities such as power walking, jogging, weight training, golf, dance sports or pilates.
Statistical analysis
All data were analysed using SAS 9.4 (SAS institute), taking into account the number of sample units to produce nationally representative estimates. P values < 0·05 were considered statistically significant. We presented socio-demographic characteristics, health behaviours and nutrient intakes (macronutrients as percentage of total energy and micronutrients as per 1000 kcal) as percentages for categorical variables or as mean values with their standard errors for continuous variables, stratified by sex. We tested differences across the quintiles of plant-based diet scores using the χ 2 test, or the PROC SURVEYREG procedure, as appropriate. To evaluate the associations between three plant-based diet scores and dyslipidaemia, we used multivariable logistic regressions to calculate the OR and 95 % CI. Model 1 adjusted for age and sex. Model 2 adjusted for age, sex, education, income, smoking status, alcohol intake, physical activity, BMI, the presence of diabetes, total energy intake and use of anti-hyperlipidaemic agent. Potential confounders in the multivariable model were selected from the previously published scientific literatures (Reference Kim, Lee and Rebholz30) with the statistical approach comparing adjusted and unadjusted effect estimates(Reference Hernán, Hernández-Díaz and Werler31). Then, we repeated the analyses with the components of dyslipidaemia (hypertriacylglycerolaemia, hypercholesterolaemia, low HDL-cholesterol, high LDL-cholesterol or high non-HDL-cholesterol). Lastly, we modelled individual food groups of uPDI simultaneously instead of uPDI score to investigate if a specific component was driving the associations with dyslipidaemia. As a sensitivity analysis, we reclassified the participants into two separate categories according to the meat consumption (those who consumed any amount of meat v. those who consumed meat at all) and then we observed the association in each group. Similar analysis was done in two separate groups classified according to the fish consumption.
Results
Characteristics of Korean adults
A total of 14 167 Korean adults (5417 men and 8750 women) were included for the analysis. The mean age was 40·8 years and 61·8% of participants were women. Participants educated college or more was 43% and half of the participants were never smokers. Heavy drinkers were 22·5 % and 21·6 % of participants were physically active. Individuals in the highest quintiles of PDI and hPDI were more likely to be older, have low education and never drinkers, and less likely to have current smokers compared with those in the lowest quintiles. Reversely, individuals in the highest quintiles of uPDI were more likely to be younger, have medium education, low income, current smokers, ≥2 times/week alcohol drinkers and less physically active compared with those in the lowest quintiles. In addition, individuals in the highest quintiles of PDI were more likely to have higher TC and LDL-cholesterol but have lower HDL-cholesterol. Individuals in the highest quintiles of hPDI were more likely to have higher TC and LDL-cholesterol. Individuals in the highest quintiles of uPDI were more likely to have slightly higher TAG but have lower TC, LDL-cholesterol and HDL-cholesterol. When we examined nutritional characteristics of diets, individuals in the highest quintiles of PDI consumed higher intakes of carbohydrates as a percentage of energy, dietary fibre, K, Ca, vitamin A, vitamin C, and lower intakes of fat as a percentage of energy and saturated fat compared with those in the lowest quintiles. Overall, hPDI was the same as PDI in the highest quintiles, but Ca was lowered in quintile 5. In uPDI, dietary fibre, K, Ca, vitamin A and vitamin C are the opposite of those in the highest quintile of PDI (online Supplementary Table S2).
Association between plant-based diet index score and dyslipidaemia
In this sample, 47% of the overall population had dyslipidaemia (44% of men and 48% of women). Individuals in the highest quintile of uPDI had 22 % higher odds and the associations remained significant when we further adjusted for socio-demographic characteristics, health parameters and lifestyle behaviours (OR: 1·22, 95 % CI 1·05, 1·41, P trend < 0·0001). Overall, hPDI showed a trend towards lower odds of dyslipidaemia, but none of the quintile results was significant. PDI score was not associated with odds of having dyslipidaemia (Table 2).
Table 1. Baseline characteristics of Korean adults* (Mean values and standard deviations; numbers and percentages)

TC, total cholesterol.
* We report means and standard errors for continuous variables and numbers and percentages for categorical variables.
Table 2. Dyslipidaemia according to quintiles of plant-based diet index scores among Korean adults* (Odds ratios and 95 % confidence intervals)

* Model 1 adjusted for age (continuous) and sex (men/women), model 2 additionally adjusted for physical activity (yes/no), smoking status (never/former/current), education level (≤6, 7–12, >12 years), income level (low/medium/high), alcohol intake (never, <2times/week, ≥ 2times/week), total energy intake (continuous), BMI (continuous), presence of diabetes (yes/no) and use of anti-hyperlipidaemic agent (yes/no).
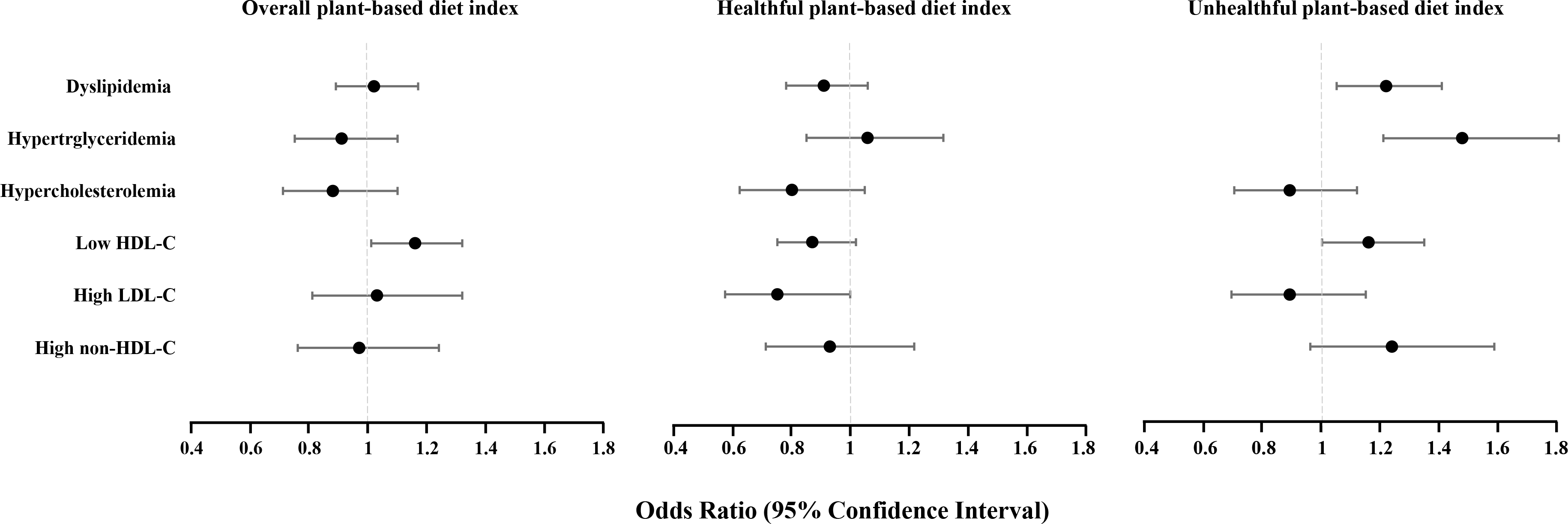
Association between plant-based diet index score and individual lipid disorders
Individuals in the highest quintile of PDI had 16 % higher odds of low HDL-cholesterol compared with those in the lowest quintile (OR: 1·16, 95 % CI 1·01, 1·32). Individuals in the highest quintile of hPDI had 25 % lower odds of high LDL-cholesterol compared with those in the lowest quintile (OR: 0·75, 95 % CI 0·57, 1·00). Individuals in the highest quintile of uPDI had 48 % higher odds of hypertriacylglycerolaemia and 16 % higher odds of low HDL-cholesterol compared with those in the lowest quintile (OR: 1·48, 95 % CI 1·21, 1·81) and (OR: 1·16, 95 % CI 1·00, 1·35) (Table 3).
Table 3. Dyslipidaemia according to quintiles of plant-based diet index scores among Korean adults* (Odds ratios and 95 % confidence intervals)

* Model was adjusted for age (continuous), sex (men/women), physical activity (yes/no), smoking status (never/former/current), education level (≤6, 7–12, >12 years), income level (low/medium/high), alcohol intake (never, < 2 times/week, ≥ 2 times/week), total energy intake (continuous), BMI (continuous), presence of diabetes (yes/no) and use of anti-hyperlipidaemic agent (yes/no).
When we modelled all food groups in the uPDI simultaneously, higher intake of sugar-sweetened beverage was associated with a 20 % higher risk of dyslipidaemia (95 % CI 1·02, 1·40) (online Supplementary Table S3).
Sensitivity analysis
We analysed the association between uPDI and dyslipidaemia according to the meat or fish consumption. We found that the associations did not change for uPDI with dyslipidaemia among individuals who consumed any amount of meat when we additionally adjusted for fish consumption as a covariate (OR quintile 5 v. quintile 1:1·21, 95 % CI 1·04, 1·42; 0·73 servings/d v. 0·69 servings/d), whereas the positive association for uPDI with dyslipidaemia disappeared among individuals who did not consume meat at all (n 272). The associations did not change for uPDI with dyslipidaemia among individuals who consumed any amount of fish when we additionally adjusted for meat consumption as a covariate (OR quintile 5 v. quintile 1:1·24, 95 % CI 1·06, 1·44) whereas this trend disappeared among individuals who did not consume fish at all (n 319).
Discussion
In this nationally representative sample of Korean adults, greater adherence to unhealthful plant-based diets captured by uPDI (i.e. fruit juices, refined grains, potatoes, sweetened beverages, sweets and desserts, salty foods) was associated with 22 % higher odds of dyslipidaemia and 48 % higher odds of hypertriacylglycerolaemia and 16% higher odds of low HDL-cholesterol. Overall, plant-based diets were associated with 16 % higher odds of low HDL-cholesterol and healthful plant-based diets were associated with 25% lower odds of high LDL-cholesterol. These results suggest that the quality of plant foods may play an important role in the prevention and management of dyslipidaemia.
The results from the present study confirm the findings of our previous studies on uPDI and elevated risk of the metabolic syndrome and hypertriacylglycerolaemia in a cross-sectional study(Reference Kim, Lee and Rebholz30) and a prospective study. (Reference Kim, Lee and Rebholz32) These studies extend that increasing the consumption of healthy plant food and decreasing the consumption of less healthy plant foods and animal foods can help prevent dyslipidaemia, a key component of the metabolic syndrome.
Several mechanisms have been suggested on the association between unhealthful plant-based diets and lipid disorders. Various food components and nutrients may affect lipid profiles. Added sugar from sweets and desserts or sugar-sweetened beverages could affect lipid metabolism such as higher TAG and cholesterol(Reference Stanhope12). Our data also showed that sugar-sweetened beverage was associated with a 20 % higher risk of dyslipidaemia. Low soya protein from legumes decreases HDL-cholesterol and increases LDL-cholesterol oxidation(Reference Jenkins, Kendall and Jackson33). High carbohydrate intake from refined grains such as white rice and noodles might contribute to TAG concentration(Reference Kang and Kim34). Dietary fibre increases cholesterol removal through binding bile acids and cholesterol(Reference Brown, Rosner and Willett35) and thus reduction of cholesterol removal would occur by low intake of dietary fibre. Low intakes of antioxidants and polyphenols would contribute to the deteriorated lipid profiles by increasing the oxidation of LDL-cholesterol(Reference Quinones, Miguel and Aleixandre36). In the present study, individuals in the highest quintile of uPDI had a higher amount of carbohydrate and lower amounts of dietary fibre and antioxidants such as vitamin A and vitamin C compared with those in the lowest quintiles of the indices.
A traditional Korean diet is mainly composed of various plant foods such as grains and vegetables unlike the diets from Western population. Increasing the amount of plant foods might not affect dyslipidaemia in Korean population who habitually followed diets rich in plant foods. Therefore, decreasing less healthy plant foods with increasing healthy plant foods may be helpful for the prevention and management of dyslipidaemia in this population. Dietary guideline for prevention of dyslipidaemia should be focused on reducing less healthy plant foods such as refined grains, fruit juices and sweets in a population who followed diets rich in plant foods for a long period.
In a sensitivity analysis, unlike the significant association between uPDI and dyslipidaemia among individuals who consumed any amount of meat or fish, the association was attenuated among those who did not consume meat or fish at all. These results suggest that the association of uPDI with dyslipidaemia may be driven in part by differences in animal food consumption such as meat or fish. Therefore, animal food consumption as well as the quality of plant foods plays an important role in the management of lipid disorders.
This study evaluated the associations between different types of plant-based diets and dyslipidaemia using recently developed plant-based diet indices. Our results expand the understanding of how diets rich in plant foods for a longer period may be associated with dyslipidaemia by influencing different types of lipids.
The strengths of our study include the use of a nationally representative sample of Korean adults, which guarantees the generalisability of the findings. Our data also contribute to the literature with a unique focus on an Asian population who have different dietary patterns than Western populations. The study includes a large sample size and used validated FFQ and adjusted for potential confounding factors. However, several limitations need to be taken into account. First, the study is designed cross-sectionally and thus the causality cannot be inferred. Second, self-reported dietary intakes are subject to measurement error. However, the FFQ was validated and showed reasonable reproducibility and validity. Third, the study did not consider the effect of different fat type from diet. We did not ask vegetable oil intake in the FFQ, although vegetable oil is a main source of dietary fat among Koreans. Different source of vegetable oils provides different fatty acids (PUFA v. SFA) and thus these could modify the associations between plant-based diets and blood lipids markers. For the calculation of plant-based diet indices, we did not take into account the dietary fat type from animal foods. Various meat sources (e.g. red meat, poultry, or fish) may have beneficial or harmful effect on blood lipids depending on the dietary fat type. For example, long-chain n-3 fatty acid from fish decreases TAG and increases HDL-cholesterol, but SFA from red meat increases LDL-cholesterol. (Reference Tou, Gucciardi and Young37,Reference Hassannejad, Moosavian and Mohammadifard38) Not considering different fat type could blur the association between plant-based diets and blood lipids. Lastly, although we adjusted for important confounders, there still be residual confounding factors.
Conclusions
In a large representative sample of Korean men and women who habitually consume diets rich in plant foods, we found that different types of plant-based diets influenced differentially on individual lipid disorders. Our study suggests that the quality of plant foods as well as animal food intake may be important for dyslipidaemia prevention. Prospective studies are needed to confirm the relationship between plant-based diet and dyslipidaemia in diverse populations with different dietary habits.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521003482
Acknowledgements
We would like to thank the study participants and staff. This research was supported by the National Research Foundation of Korea (NRF), grant funded by the Korea government (MSIT) (NRF2021R1A2C1003211 to JK), South Korea. The funders had no role in study design, data collection and analysis, decision topublish, or preparation of the manuscript.
The authors’ contributions are as follows: N.R. contributed to data analysis and writing the first draft. J. K. was the principal investigator and designed the study and interpretation of the findings and wrote the manuscript. All authors read and approved the final manuscript.
The authors have no financial or personal conflicts of interest to declare.