Introduction
Through qualitative research and witness statements, childhood sexual abuse (CSA) survivors have provided powerful accounts of the pervasive personal impact of CSA (Australian Royal Commission into Institutional Responses to Child Sexual Abuse, 2017; Isely et al., Reference Isely, Isely, Freiburger and McMackin2008). Extensive quantitative research complements these individual accounts by documenting population-level associations between CSA and a range of problems in adulthood, including higher rates of mental, physical, and psychosocial difficulties (for multi-outcome reviews, see Hailes et al., Reference Hailes, Yu, Danese and Fazel2019; Irish et al., Reference Irish, Kobayashi and Delahanty2010; Lippard & Nemeroff, Reference Lippard and Nemeroff2020). However, methodological limitations and a narrow focus on mental health outcomes in much of the existing literature mean that we do not yet have good quality population-based evidence about the links between CSA and adverse outcomes across multiple life domains, how strong those links are, and whether they persist across adulthood.
Three common limitations in the literature constrain our understanding of the long-term outcomes associated with CSA. First, most studies have focused on a small number of specific outcomes in one or two domains of functioning (mostly mental health), and at one point in time. Yet, we know from CSA survivors that the impacts can be diverse and interconnected, and that they manifest across multiple domains of function at different life stages (Australian Royal Commission into Institutional Responses to Child Sexual Abuse, 2017). Second, most primary studies have relied on clinical or selected rather than general population samples (e.g., Dunlop et al., Reference Dunlop, Hill, Johnson, Klein, Gelenberg, Rothbaum and Kocsis2015; Lewis et al., Reference Lewis, McElroy, Harlaar and Runyan2016), used cross-sectional retrospective designs (e.g., Sachs-Ericsson et al., Reference Sachs-Ericsson, Blazer, Plant and Arnow2005), or applied inadequate controls for possible confounders such as other major childhood stressors that often coincide with CSA (e.g., Papalia et al., Reference Papalia, Luebbers, Ogloff, Cutajar and Mullen2017), all of which can introduce bias, produce inflated effect sizes, and reduce generalizability of the findings. Third, the use across the literature of inconsistent definitions of CSA and different methods of measuring outcomes makes it difficult to synthesize the available evidence and to understand the extent of the relationship between CSA and risk for adverse outcomes across multiple life domains in adulthood (discussed in Cicchetti & Toth, Reference Cicchetti and Toth2004; Danese & Widom, Reference Danese and Widom2020; Hailes et al., Reference Hailes, Yu, Danese and Fazel2019).
A definitive causal link between CSA and outcomes in adulthood cannot be ethically determined because it would require random assignment to CSA, but good quality longitudinal studies that adjust for potential confounding factors can help researchers get closer to understanding the relationship. By following cohorts of individuals with substantiated child maltreatment into adolescence and adulthood and comparing them to a matched control group, the seminal studies by Widom and colleagues (e.g., Osborn & Widom, Reference Osborn and Widom2020; Widom et al., Reference Widom, Czaja, Bentley and Johnson2012; Widom, Reference Widom1989; Wilson & Widom, Reference Wilson and Widom2009) and the LONGSCAN series of studies (e.g., Lewis et al., Reference Lewis, McElroy, Harlaar and Runyan2016; Runyan et al., Reference Runyan, Curtis, Hunter, Black, Kotch, Bangdiwala and Landsverk1998) have provided valuable information about the long-term mental, physical, sexual, and antisocial consequences associated with CSA. However, findings from such selected-sample studies may not generalize to the wider population: children with court- or child protective service-substantiated instances of CSA are likely to represent a small proportion of those who experience it, and to differ in systematic ways from those who experienced CSA but did not report it or go through a legal process.
Good quality evidence relating to the long-term outcomes associated with CSA in the general population comes from prospective longitudinal studies in which a population-based (rather than selected) cohort of individuals is followed over their life course, and adjustments made for prospectively measured covariates. Most such studies have examined CSA-related outcomes in young adulthood (age 18–30), and have come from a small number of parent studies. Data from the Christchurch Health and Development Study, Queensland Mater-University Pregnancy Study, and Dunedin Multidisciplinary Health and Development Study ("Dunedin Study") show associations between CSA and higher risk for specific indicators of physical (Mamun, Lawlor, et al., Reference Mamun, Lawlor, O'Callaghan, Bor, Williams and Najman2007), mental (Fergusson et al., Reference Fergusson, Beautrais and Horwood2003, Reference Fergusson, Boden and Horwood2008; Goodwin et al., Reference Goodwin, Fergusson and Horwood2005; Hayatbakhsh et al., Reference Hayatbakhsh, Najman, Jamrozik, Mamun, O'Callaghan and Williams2009; Hyland et al., Reference Hyland, Murphy, Shevlin, Vallières, McElroy, Elklit and Cloitre2017; Kisely et al., Reference Kisely, Strathearn and Najman2020; Mamun, Alati, et al., Reference Mamun, Alati, O'Callaghan, Hayatbakhsh, O'Callaghan, Najman and Bor2007), sexual (van Roode et al., Reference van Roode, Dickson, Herbison and Paul2009), interpersonal (Friesen et al., Reference Friesen, Woodward, Horwood and Fergusson2010; Murphy et al., Reference Murphy, Elklit and Shevlin2020), and economic (Najman et al., Reference Najman, Scott, Farrington, Clavarino, Williams, McGee and Kisely2022) problems in young adulthood. However, CSA was not always significantly associated with higher risk for specific outcomes (e.g., educational outcomes in Boden et al., Reference Boden, Horwood and Fergusson2007), especially in the Queensland Mater-University Pregnancy Study, which showed an overall pattern of weak and inconsistent associations between CSA and adverse outcomes in young adulthood (Strathearn et al., Reference Strathearn, Giannotti, Mills, Kisely, Najman and Abajobir2020).
Fewer population-based prospective studies have examined associations between CSA and outcomes in mid to late adulthood. In midlife (ages 31–44), data from the Christchurch Health and Development Study and (US) National Longitudinal Study of Adolescent to Adult Health show associations between CSA and higher risk for physical (Duncan et al., Reference Duncan, Mulder, Wilkinson and Horwood2019), mental (Bell et al., Reference Bell, Foulds, Horwood, Mulder and Boden2019), sexual (Cleland et al., Reference Cleland, McLeod, Dhakal, Fenton, Welch, Horwood and Boden2022), and economic problems (Assini-Meytin et al., Reference Assini-Meytin, Thorne, Sanikommu, Green and Letourneau2022). In middle age, data from the 1958 (British) National Child Development Study (Power & Elliott, Reference Power and Elliott2005) show associations between CSA and higher risk for premature mortality between ages 45 and 58 (Rogers et al., Reference Rogers, Power and Pinto Pereira2021), as well as specific indicators of poorer physical health (physical functioning and self-rated health, Archer et al., Reference Archer, Pinto Pereira and Power2017; high glycated hemoglobin, Li et al., Reference Li, Pinto Pereira and Power2019; health risk behaviors and faster age-related gains in body mass index, Power et al., Reference Power, Pinto Pereira and Li2015), mental health (composite psychopathology measure, Clark et al., Reference Clark, Caldwell, Power and Stansfeld2010; suicidal ideation, Stansfeld et al., Reference Stansfeld, Clark, Smuk, Power, Davidson and Rodgers2017), and economic (lack of assets, benefit use, financial insecurity, and low socioeconomic status, Pinto Pereira et al., Reference Pinto Pereira, Li and Power2017) outcomes. However, CSA was not significantly associated with every outcome assessed in every study, indicating that the results can depend on the specific measures and control variables used.
These studies provide important evidence that CSA is likely to be associated with a range of adverse outcomes in multiple life domains, and at multiple different points in adulthood. However, the separate findings from each study are difficult to consolidate as they predominantly focus on specific mental health diagnoses, consider a small number of outcomes in one life domain at one time-point, and use different definitions of CSA. While some studies have considered outcomes in several domains across wider timeframes in adulthood (Easton et al., Reference Easton, Kong, Gregas, Shen and Shafer2019; Fergusson et al., Reference Fergusson, McLeod and Horwood2013) or summarized findings across several different articles based on the same cohort (Power et al., Reference Power, Li and Pinto Pereira2020; Strathearn et al., Reference Strathearn, Giannotti, Mills, Kisely, Najman and Abajobir2020), to date none have taken a wider view and systematically assessed associations between CSA and the persistence across adulthood of problems in multiple domains of functioning.
By following a large, population-based cohort of individuals since birth, and repeatedly assessing a range of outcomes in six key domains (physical, mental, sexual, interpersonal, economic, and antisocial) across a 20-year period from young adulthood to midlife, this study aims to provide some of the most comprehensive evidence to date about the long-term outcomes associated with CSA. Using the rich biopsychosocial data set from the Dunedin Study (Poulton et al., Reference Poulton, Moffitt and Silva2015) we sought to provide population-based evidence that quantifies the extent and persistence across adulthood of adverse outcomes associated with CSA, after taking into account other major coinciding stressors such as socioeconomic disadvantage and other adverse childhood experiences. We also sought to assess cumulative risk for adverse outcomes across multiple domains, and address questions about how CSA definition impacts the findings. In doing so, we aim to advance the state of the evidence and provide survivors, practitioners, and policy makers with good quality information on which to act to prevent or ameliorate the long-term outcomes associated with CSA.
Method
Study design and population
Participants were members of the Dunedin Study, a longitudinal investigation of health and behavior in a representative birth cohort. Participants (n = 1037; 91% of eligible births; 52% male) were all individuals born between April 1972 and March 1973 in Dunedin, New Zealand, who were eligible based on residence in the province and who participated in the first assessment at age 3 years (Poulton et al., Reference Poulton, Moffitt and Silva2015). The cohort represented the full range of socioeconomic status in the general population of New Zealand’s South Island and as adults matched the New Zealand National Health and Nutrition Survey on key adult health indicators and the New Zealand Census of citizens of the same age on educational attainment (Poulton et al., Reference Poulton, Hancox, Milne, Baxter, Scott and Wilson2006; Richmond-Rakerd et al., Reference Richmond-Rakerd, D’Souza, Andersen, Hogan, Houts, Poulton and Moffitt2020). The cohort is primarily New Zealand European/white (93%), matching South Island demographics. Assessments were carried out at birth and ages 3, 5, 7, 9, 11, 13, 15, 18, 21, 26, 32, 38, and most recently (completed April 2019) 45 years, when 94% (n = 938) of the 997 participants still alive took part. At each assessment, participants came to the research unit for interviews and examinations. The New Zealand Health and Disability Ethics Committee approved the study, and informed written consent was obtained from all participants.
Child sexual abuse measures
CSA was assessed via computer-based questionnaire at age 26 years within a wider set of questions about sexual and reproductive health. Participants indicated whether they had experienced specific types of unwanted sexual contact before age 16, including genital touching (touched by or forced to touch perpetrator), attempted intercourse, or forced intercourse (Table S1 shows question wording). Of the 980 study members who took part in the age 26 assessments, 938 (96%) answered at least one question about CSA type. One person was excluded from analysis as their responses were contradictory, leaving a final sample of 937 participants. Note that it was not routine practice in general population studies in the 1970s and 80s, when study members were minors, to ask about CSA or to systematically seek out objective records relating to CSA exposure. Hence, we focused on retrospective reports of CSA provided by participants at the age 26 assessment.
Our primary analyses compared those who reported experiencing any type of CSA (genital touching, attempted or forced intercourse) with those who did not. Given there is no consensus on the best definition of CSA for research purposes, and because different definitions may produce different results, we also conducted secondary analyses that compared outcomes for three alternative groupings: those who reported (i) forced or attempted intercourse versus all other participants; (ii) forced intercourse versus all other participants; and (iii) forced intercourse versus no CSA.
Outcomes in adulthood
Physical
Health risk behaviors. At ages 26, 32, 38, and 45, study members were asked to report their smoking and alcohol consumption, as previously reported (Rasmussen et al., Reference Rasmussen, Caspi, Ambler, Danese, Elliott, Eugen-Olsen and Moffitt2020). At each phase, participants were assessed as engaging in health risk behaviors if they were a current smoker or exceeded New Zealand Ministry of Health maximum alcohol consumption guidelines (>10 alcoholic drinks per week for women or 15 for men; see https://www.health.govt.nz/your-health/healthy-living/addictions/alcohol-and-drug-abuse/alcohol).
Systemic inflammation. Following previous Dunedin Study work (Danese et al., Reference Danese, Moffitt, Pariante, Ambler, Poulton and Caspi2008), we used three indicators of systemic inflammation that were all measured from blood samples drawn at ages 32, 38, and 45: serum high-sensitivity C-reactive protein, fibrinogen, and white blood cells. At each phase, participants were counted as having high systemic inflammation if they exceeded established normative cutoffs: high-sensitivity C-reactive protein > 3 mg/L (Pearson et al., Reference Pearson, Mensah, Alexander, Anderson and Cannon2003), fibrinogen > 4 g/L (Mackie et al., Reference Mackie, Kitchen, Machin and Lowe2003), or white blood cells >11 × 109cells/L (Dean, Reference Dean2005).
Metabolic syndrome. At ages 26, 32, 38, and 45, participants were counted as having metabolic syndrome if they had at least three of the following risk indicators based on the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), and as previously described (Israel et al., Reference Israel, Moffitt, Belsky, Hancox, Poulton, Roberts and Caspi2014): waist circumference >88 cm for women or 102 cm for men; systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥ 85mmHg; high density lipoprotein ≤40 mg/dL for men or 50mg/dL for women; triglycerides ≥2.26 mmol/L; or glycated hemoglobin ≥5.7%. Data for high density lipoprotein and glycated hemoglobin at age 45 were calibrated against prior data up to age 38 due to changes in assay methods.
Low lung function. At ages 26, 32, 38, and 45, pre-bronchodilator forced expiratory volume in 1 s (FEV1) was measured using a computerized spirometer and Vmax body plethysmograph (Care Fusion, Yorba Linda, CA, USA), as previously described (Hancox et al., Reference Hancox, Thomas, Williams and Sears2020). Normative values for the Dunedin study population were calculated for each assessment phase by creating sex-specific spirometry prediction equations from separate multiple linear regression models including never-tobacco smoking, nonpregnant women, and nonasthmatic women and men, and using height and height squared as predictors (Zhang, Reference Zhang2021). One extreme outlier (height <1m) was excluded. We then calculated each participant’s FEV1 as a percentage of their age and sex-predicted FEV1. At each phase, participants in the lowest tertile of predicted FEV1 were counted as having low lung function.
Poor oral health. We examined oral health in light of evidence that child maltreatment is associated with poorer oral health outcomes (reviewed in Bradbury-Jones et al., Reference Bradbury-Jones, Isham, Morris and Taylor2019). We used two indicators of oral health problems: periodontal disease and caries. Examinations were carried out by calibrated dental examiners at ages 26, 32, 38, and 45, as described previously (Broadbent et al., Reference Broadbent, Thomson and Poulton2008; Thomson et al., Reference Thomson, Broadbent, Poulton and Beck2006). A periodontal examination was conducted by examining three sites (mesiobuccal, buccal, and distolingual) per tooth (excluding third molars) using a PCP-2 periodontal probe. Periodontal attachment loss was computed as the sum of gingival recession and probing depth. Participants were counted as having periodontal disease if they had 1 or more site(s) with ≥5 mm of combined attachment loss.
Teeth were examined for caries and restorations following the World Health Organization Oral Health Surveys methodology. Four surfaces were considered for canine and incisor teeth: buccal, lingual, distal, and mesial; a fifth surface, occlusal, was considered for premolar and molar teeth. Tooth surfaces were classified as having untreated caries if a cavitated carious lesion was present, as filled if a dental restoration was present (including crowns), and missing due to caries if the participant indicated that a given tooth had been removed due to decay or failed dental restorative work. The proportion of caries-affected tooth surfaces was then calculated. Surfaces of teeth that were unerupted, lost due to trauma, extracted for reasons other than caries (impaction, orthodontic treatment, or periodontal disease), or could not be visualized by the examiner were excluded from calculations. Participants were counted as having high caries if more than 25% of their tooth surfaces had been caries-affected (including tooth loss due to caries). At each phase, participants were counted as having poor oral health if they had periodontal disease or high caries.
Mental
Externalizing, internalizing, and thought disorder. At ages 26, 32, 38, and 45, health professionals interviewed study members using the Diagnostic Interview Schedule (Robins et al., Reference Robins, Helzer, Croughan and Ratcliff1981, Reference Robins, Cottler, Bucholz and Compton1995) which assessed a comprehensive set of disorders defined by relevant DSM criteria. As previously described, diagnoses were based on symptom algorithms and impairment ratings, but also incorporated information from standardized informant reports, psychiatrists’ review of interviewers’ detailed case notes, pharmacists’ medication review, and staff ratings of symptoms observed (Caspi et al., Reference Caspi, Houts, Ambler, Danese, Elliott, Hariri and Moffitt2020; Meier et al., Reference Meier, Caspi, Reichenberg, Keefe, Fisher, Harrington and Moffitt2014). Consistent with previous Dunedin Study work (2020), we assessed three categories of mental disorders: externalizing (attention-deficit/hyperactivity disorder, conduct disorder, alcohol dependence, cannabis dependence, other drug dependence, and tobacco dependence), internalizing (depression, generalized anxiety disorder, fears [including social phobia, simple phobia, agoraphobia, and panic disorder], posttraumatic stress disorder, and eating disorders [including bulimia and anorexia]), and thought (obsessive-compulsive disorder, mania, and schizophrenia). At each phase, participants who met DSM diagnostic criteria for an externalizing, internalizing, or thought disorder were counted in the relevant category.
Suicide attempt. At ages 18, 21, 26, 32, 38, and 45, suicide attempts were queried during structured interviews about self-harm and suicide and again as a symptom of depression during structured diagnostic interviews for depression, as previously described (Goldman-Mellor et al., Reference Goldman-Mellor, Caspi, Harrington, Hogan, Nada-Raja, Poulton and Moffitt2014). For this study, we analyzed whether participants had ever attempted suicide in their lifetime (i.e., by age 45).
Sexual
The questions on sexual health and behavior used in this study were adapted from the British National Survey of Sexual Attitudes and Lifestyles questionnaire (Johnson et al., Reference Johnson, Wadsworth, Wellings and Field1994; Mitchell et al., Reference Mitchell, Ploubidis, Datta and Wellings2012).
Sexual difficulties. At ages 38 and 45, participants who had sex in the past 12 months were asked if in the past 12 months they had experienced any of the following for three months or longer: lacked interest in having sex, lacked enjoyment in sex, felt anxious during sex, felt physical pain as a result of sex, felt no arousal or excitement during sex, did not come to a climax or took a long time to reach a climax despite feeling excited/aroused, came to climax more quickly than they would like, had trouble with vaginal dryness (females) or getting and keeping an erection (males). At each age, participants were counted as having sexual difficulties if they reported at least one of these problems.
Risky sex. At ages 26, 32, 38, and 45, participants who had ever had sex were asked how many same and opposite sex partners they had in the past 12 months, and how often they used a condom in the past 12 months. Participants were counted as having engaged in risky sex if they had two or more sexual partners in the past year and reported using a condom sometimes or never. This definition follows previous Dunedin Study work (Ramrakha et al., Reference Ramrakha, Caspi, Dickson, Moffitt and Paul2000), but uses two instead of three or more partners due to the relatively small number of people in the CSA-exposed groups.
Sexually transmitted diseases. At ages 26, 32, 38, and 45, study members who had ever had sex were asked to report whether they had been diagnosed with a sexually transmitted disease since the last assessment point. Their serum samples were also analyzed for the presence of Herpes Simplex Virus 2 using indirect enzyme immunoassay (Eberhart-Phillips et al., Reference Eberhart-Phillips, Dickson, Paul, Herbison, Taylor and Cunningham2001). At each phase, participants were counted as having a sexually transmitted disease if they self-reported being diagnosed with one since the last assessment point or were seropositive for Herpes Simplex Virus 2.
Interpersonal
High-conflict relationship. At ages 26, 32, 38, and 45, study members who were in a relationship completed the 33-item Dunedin Study Abuse scales, as previously described (Bourassa et al., Reference Bourassa, Caspi, Harrington, Houts, Poulton, Ramrakha and Moffitt2020). Study members reported their experience as both victim and perpetrator of 33 abusive behaviors within their intimate partner relationship in the past 12 months. Given the high correlation between victim and perpetrator scores (Bourassa et al., Reference Bourassa, Caspi, Harrington, Houts, Poulton, Ramrakha and Moffitt2020), an overall relationship conflict score was derived for each age by summing the 66 behaviors (possible range 0-66). At each phase, participants were counted as being in a high-conflict relationship if their score was in the highest tertile.
Not in a relationship. At ages 26, 32, 38, and 45, participants were counted as not being in a relationship if they reported that in the past year they had not been involved with someone in a romantic (intimate or close) relationship that lasted at least one month.
Parenting difficulties. For study members who were parents, research workers visited their home when their first child was around age 3 and videotaped the parent interacting with their child. During the home visit, each parent-child dyad was videotaped in three increasingly demanding semi-structured tasks, each lasting 10 min. The video recordings of these three tasks were later coded using a set of 7-point scales developed for the NICHD Study of Early Child Care (NICHD Early Child Care Research Network, 1999): sensitive responsiveness, stimulation of cognitive development, positive regard for the child, detachment, intrusiveness, and negative regard for the child (Belsky et al., Reference Belsky, Jaffee, Sligo, Woodward and Silva2005). Scores for sensitive responsiveness, stimulation of cognitive development, positive child regard, and detachment were averaged across the tasks and the four averaged ratings were used to create a composite "positive parenting" score (McAnally et al., under review July 2022). Participants whose score was in the lowest tertile were counted as having parenting difficulties.
Economic wellbeing
Qualifications. At ages 32, 38, and 45, study members reported their highest educational qualification. In this study, participants were counted as having no formal educational qualifications if they had not acquired any by age 45 (i.e., did not have at least a high school-level qualification or its equivalent).
Socioeconomic status. At ages 32, 38, and 45, study members’ current or most recent (i.e., at the previous assessment phase) occupation was coded using a six-point scale for occupations in New Zealand; those without current or recent occupation data were rated on the basis of their educational achievement according to criteria in the New Zealand Socioeconomic Index 1996 (Davis et al., Reference Davis, Jenkin and Coope2003). At each phase, participants with a score of 1 or 2 were counted as being in a low socioeconomic status group. Occupation data were also collected at age 26 but not used to calculate socioeconomic status for that phase because of the transient nature of that period.
Benefit use. The New Zealand Ministry of Social Development provided information on study members’ benefit use from age 21 to 46. We obtained information about spells and duration of the following New Zealand government benefits: Unemployment Benefit, Unemployment Benefit Hardship, Unemployment Benefit Training, Job Seeker, Emergency Benefit, Emergency Maintenance Allowance, Invalids Benefit, Sickness Benefit, Widows Benefit, Sole Parent Support, Youth/Young Parent Payment, Domestic Purposes Benefit-Woman Alone, Domestic Purposes Benefit-Caring for Sick or Infirm, and Supported Living Payment. Only one benefit can be received at any given time. At each phase, participants were counted as having high benefit use if their number of days on a benefit since the last phase was in the highest tertile.
Financial difficulties. At ages 26, 32, 38, and 45, study members were asked six questions about credit difficulties and seven about money management problems. As previously described, these scores were summed and an overall financial difficulties score computed by standardizing and then averaging the credit difficulties and money management scores (Moffitt et al., Reference Moffitt, Arseneault, Belsky, Dickson, Hancox, Harrington, Houts, Poulton, Roberts, Ross, Sears, Thomson and Caspi2011). At each phase, participants were counted as having financial difficulties if their total score was in the highest tertile.
Antisocial behavior
High delinquency. At ages 26, 32, 38, and 45, participants completed a self-reported delinquency questionnaire in which they reported their engagement in 48 delinquent acts in the past year (Moffitt & Silva, Reference Moffitt and Silva1988). At each phase, we summed the number of antisocial behaviors participants engaged in and created separate tertiles for males and females; those with a score in the highest tertile for their sex were counted as having high delinquency.
Criminal conviction. The New Zealand Police provided information about study members’ criminal convictions, which ranged from minor offenses such as cannabis possession and shoplifting through to assault, rape, and manslaughter. Participants were counted as having a criminal conviction if they had any conviction recorded by age 45.
Covariates
Sex
Sex was recorded as male or female at birth.
Childhood socioeconomic status
Socioeconomic status was measured repeatedly from birth through age 15 years using a scale that placed parents’ occupations into 1 of 6 categories based on educational achievement and income associated with that occupation in the New Zealand Census (Poulton et al., Reference Poulton, Caspi, Milne, Thomson, Taylor, Sears and Moffitt2002). Our analyses used the average across assessments of the highest socioeconomic status of either parent.
Child harm and household dysfunction adverse childhood experiences (ACEs)
Our adverse childhood experience measures correspond to the categories introduced by the CDC Adverse Childhood Experiences Study (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards and Marks1998), which included five types of child harm (physical abuse, emotional abuse, physical neglect, emotional neglect and sexual abuse) and five types of household dysfunction (incarceration of a family member, household substance abuse, household mental illness, loss of a parent, and household partner violence). Prospective child harm and household dysfunction adverse childhood experience counts were generated from archival Dunedin Study records gathered during seven biennial assessments carried out from ages 3 to 15 years, as previously described (Reuben et al., Reference Reuben, Moffitt, Caspi, Belsky, Harrington, Schroeder and Danese2016). As CSA was our primary exposure of interest in this study, it was excluded from the count of child harm adverse childhood experiences. For analysis, we truncated the child harm and household dysfunction ACE counts to three groups: 0, 1, and 2 or more.
Sexual assault in adulthood
Unwanted adult sexual experiences were queried at ages 21, 32, and 38 years; participants also completed a life history calendar (Caspi et al., Reference Caspi, Moffitt, Thornton, Freedman, Amell, Harrington and Silva1996) at each phase to document major life events. Sexual assault in adulthood was indicated if participants: at the age 21 assessment reported being forced the first time they had sex and that their first time was after age 16 (to avoid overlap with our CSA definition); at the age 21, 32, or 38 assessments reported unwanted touching, attempted intercourse, or forced intercourse since the last assessment phase; or reported sexual assault since age 38 in the life history calendar.
Analysis
All analyses were conducted using Stata/IC 16 (HG) and checked via independent replication by a second analyst (JK). First, we calculated the proportion of participants in each CSA group who met criteria for each of the outcomes in the physical, mental, sexual, interpersonal, socioeconomic, and antisocial domains. For the 17 outcomes repeatedly assessed across adulthood (health risk behaviors, high systemic inflammation, metabolic syndrome, low lung function, poor oral health, externalizing disorder, internalizing disorder, thought disorder, sexual difficulties, risky sex, sexually transmitted diseases, high-conflict relationships, lack of intimate relationships, low socioeconomic status, high benefit use, financial difficulties, and high delinquency), we counted participants as having a particular problem if they met criteria for that outcome at multiple assessment points (two or more) between ages 26 and 45 to assess whether adverse outcomes were evident repeatedly across adulthood. To understand cumulative problems across multiple life domains, we calculated the number of domains in which participants had at least one problem across adulthood. To minimize data loss, participants were included in particular analyses if they had the minimum data required to reasonably address the research question: that is, data available for a particular outcome at two or more time points for the analyses with the 17 repeated measures; data available for four or more domains for the multi-domain analyses. Table S2 summarizes the sample size available for analyses with each outcome.
Primary analyses. We used Poisson regression with robust standard errors to assess associations between CSA and specific problems in adulthood, including problems across multiple domains. To understand the influence of potential confounding factors, sex, childhood socioeconomic status, child harm ACEs, household dysfunction ACEs, and sexual assault in adulthood were entered into the regression models in a stepwise fashion: Model 1 included sex; Model 2 added childhood socioeconomic status; Model 3 added child harm ACEs; Model 4 added household dysfunction ACEs; and Model 5 added sexual assault in adulthood.
Secondary analyses. We used the same statistical approach to assess whether the results observed in the primary analyses depended on the definition of CSA, but to reduce complexity and repetition focused on the fully adjusted model including all control variables (Model 5).
Supplementary analyses. We conducted additional sensitivity analyses to test whether the observed results were: i) an artifact of using cutoffs for continuous variables; (ii) consistent when we used quartile rather than tertile cutoffs for variables that did not have established cutoffs (relationship conflict, parenting difficulties, benefit use, financial difficulties, and delinquency; results not shown); and (iii) were evident across assessment phases. We used the same statistical approaches as for our secondary analyses, except used linear regression to assess the associations between CSA and continuous outcomes.
Results
Childhood sexual abuse prevalence and participant characteristics
One in five (19% overall; 30% of females; 9% of males) participants reported at least one type of CSA; one in twenty (6% overall; 10% of females; 2% of males) reported the most severe type: forced intercourse (Table 1). The any CSA (compared to no CSA) group included higher proportions of people who were female, grew up in lower socioeconomic status families, had more child harm and household dysfunction ACEs, and had reported being sexually assaulted in adulthood (Table 2).
Table 1. Self-reported childhood sexual abuse exposure in the Dunedin study birth cohort (N = 937)

Table 2. Participant characteristics by different definitions of childhood sexual abuse exposure

Note. CSA = childhood sexual abuse. † p < 0.06, *p < 0.05, ** p < 0.01, ***p < 0.001. Subgroup sample sizes do not always add to the total due to missing data for some variables. Bolded test statistics indicate statistically significant effects.
Primary analyses: Any versus no CSA
The unadjusted prevalence of every problem except sexual difficulties, risky sex, parenting difficulties, and criminal convictions was numerically higher among those who reported any compared with no CSA (Figure 1; Table S3). Those who reported CSA also had problems across adulthood in more domains (Figure S1). However, these observed relationships may have been affected by confounding with sex, childhood socioeconomic status, child harm ACEs, household dysfunction ACEs, and/or sexual assault in adulthood. We sought to understand the relationships between CSA and problems across adulthood after adjusting for each of these factors in turn.

Figure 1. Unadjusted prevalence of persistent problems among those who reported any versus no childhood sexual abuse. Error bars show 95% confidence intervals.
After adjusting for sex (Model 1, Table 3), CSA was significantly associated with higher risk of the following problems across the assessed domains: physical (health risk behaviors, high systemic inflammation, low lung function, poor oral health); mental (externalizing disorder, internalizing disorder, thought disorder, suicide attempts); sexual (sexually transmitted diseases); interpersonal (high-conflict relationships); economic (no formal qualifications, low socioeconomic status, high benefit use, financial difficulties); antisocial (high delinquency, criminal convictions); and multi-domain (cumulative problems across multiple domains). We did not observe statistically significant associations between CSA and metabolic syndrome, sexual difficulties, risky sex, lack of intimate relationships, and parenting difficulties.
Table 3. Associations between childhood sexual abuse and problems across adulthood

Notes. RR = relative risk. SES = socioeconomic status. ACEs = adverse childhood experiences. Model 1 includes sex; Model 2 sex and childhood socioeconomic status; Model 3 sex, childhood socioeconomic status, and child harm adverse childhood experiences; Model 4 sex, childhood socioeconomic status, child harm adverse childhood experiences, and household dysfunction adverse childhood experiences; Model 5 sex, childhood socioeconomic status, child harm adverse childhood experiences, and household dysfunction adverse childhood experiences and sexual assault in adulthood. All relative risks show the difference between those who reported forced intercourse and all other participants (reference group). Bolded text indicates statistical significance. *p < 0.05, **p < 0.01, ***p < 0.001.
After adding childhood socioeconomic status to the model (Model 2, Table 3), CSA remained significantly associated with the following problems across the assessed domains: physical (health risk behaviors and poor oral health); mental (externalizing disorder, internalizing disorder, thought disorder, and suicide attempts); sexual (sexually transmitted diseases); interpersonal (high-conflict relationships); economic (high benefit use and financial difficulties); antisocial (high delinquency and criminal convictions); and multi-domain (cumulative problems across multiple domains). The associations observed in Model 1 between CSA and high systemic inflammation, low lung function, lack of formal qualifications, and low socioeconomic status in adulthood were no longer statistically significant; associations with metabolic syndrome, sexual difficulties, risky sex, lack of intimate relationships, and parenting difficulties remained nonsignificant.
The addition of child harm ACEs to the model (Model 3, Table 3) did not further change the pattern of results. After including household dysfunction ACEs (Model 4, Table 3), CSA was no longer significantly associated with criminal convictions, but all other patterns remained the same. After adjusting for all control variables in the final model (Model 5, Table 3), CSA was significantly associated with the following problems across the assessed domains (RRs range 1.32-2.64): physical (health risk behaviors, poor oral health); mental (externalizing disorder, internalizing disorder, thought disorder, suicide attempts); sexual (sexually transmitted diseases); interpersonal (high-conflict relationships); economic (high benefit use, financial difficulties); antisocial (high delinquency); and multi-domain. Figure 2 summarizes the results for this final model across all outcomes.

Figure 2. Adjusted group differences in the prevalence of problems across adulthood among those who reported any versus no childhood sexual abuse. Relative risks from the regression models including all control variables (sex, childhood socioeconomic status, child harm and household dysfunction adverse childhood experiences, and sexual assault in adulthood) are shown along with their 95% confidence intervals.
Secondary analyses: Effects with different CSA definitions
To assess whether the observed participant characteristics and pattern of CSA-related problems across adulthood was specific to the CSA definition used in the primary analyses (any versus no CSA), we repeated our analyses with three alternative analytic groupings that differed in relative severity: those who reported (i) forced or attempted intercourse versus all other participants; (ii) forced intercourse versus all other participants; and (iii) forced intercourse versus no CSA. Regarding participant characteristics, a consistent picture emerged, with female sex, lower childhood socioeconomic status, and more household dysfunction ACEs consistently and significantly linked to all four measures of CSA. There were also consistent numerical trends across CSA definitions, indicating more child harm ACEs and greater likelihood of sexual assault in adulthood among those who reported CSA. However, effects for those variables were statistically significant only for the comparisons between: i) any and no CSA; and ii) forced or attempted intercourse and all other participants, possibly reflecting the greater uncertainty around the effect estimates with smaller numbers of participants in the exposed groups (see Table 2).
Table S3 summarizes the unadjusted prevalence of problems by different CSA definitions. Table 4 summarizes the group differences for each CSA definition after taking into account all control variables, and Figure 3 illustrates those differences. The first point to note is that the overall pattern of findings was consistent across the different definitions, albeit with some differences in statistical significance due to severity-related differences in effect size (i.e., smaller effect sizes for comparisons with less severe CSA types) and sample size in the exposed group (i.e., smaller sample size and less certain estimates in the comparisons with more severe CSA types). For all four definitions, participants in the exposed group had significantly higher risk of the following problems across the assessed domains: physical (health risk behaviors [RRs 1.32–1.49], poor oral health [RRs 1.50–1.67]); mental (externalizing disorder [RRs 1.44–1.59], internalizing disorder [RRs 1.40–1.68], and suicide attempts [RRs 2.64–4.22]); interpersonal (high-conflict relationships [RRs 1.43–1.70]); economic (high benefit use [RRs 1.37–1.53], financial difficulties [RRs 1.36–1.60]); antisocial (high delinquency [RRs 1.82–2.32]); and multi-domain (RRs 1.41–1.52). Similarly, for all four definitions of CSA, participants in the exposed groups were not significantly more likely to have: low lung function, sexual difficulties, risky sex, lack of intimate partner relationships, parenting difficulties, lack of formal qualifications, low socioeconomic status, or a criminal conviction. For three of the four CSA definitions, participants in the exposed group were more likely to have high systemic inflammation (RRs 1.44–1.81; significant for all definitions except the any versus no CSA comparison) and thought disorder (RRs 2.31–2.85; significant for all definitions except forced intercourse versus all other participants).
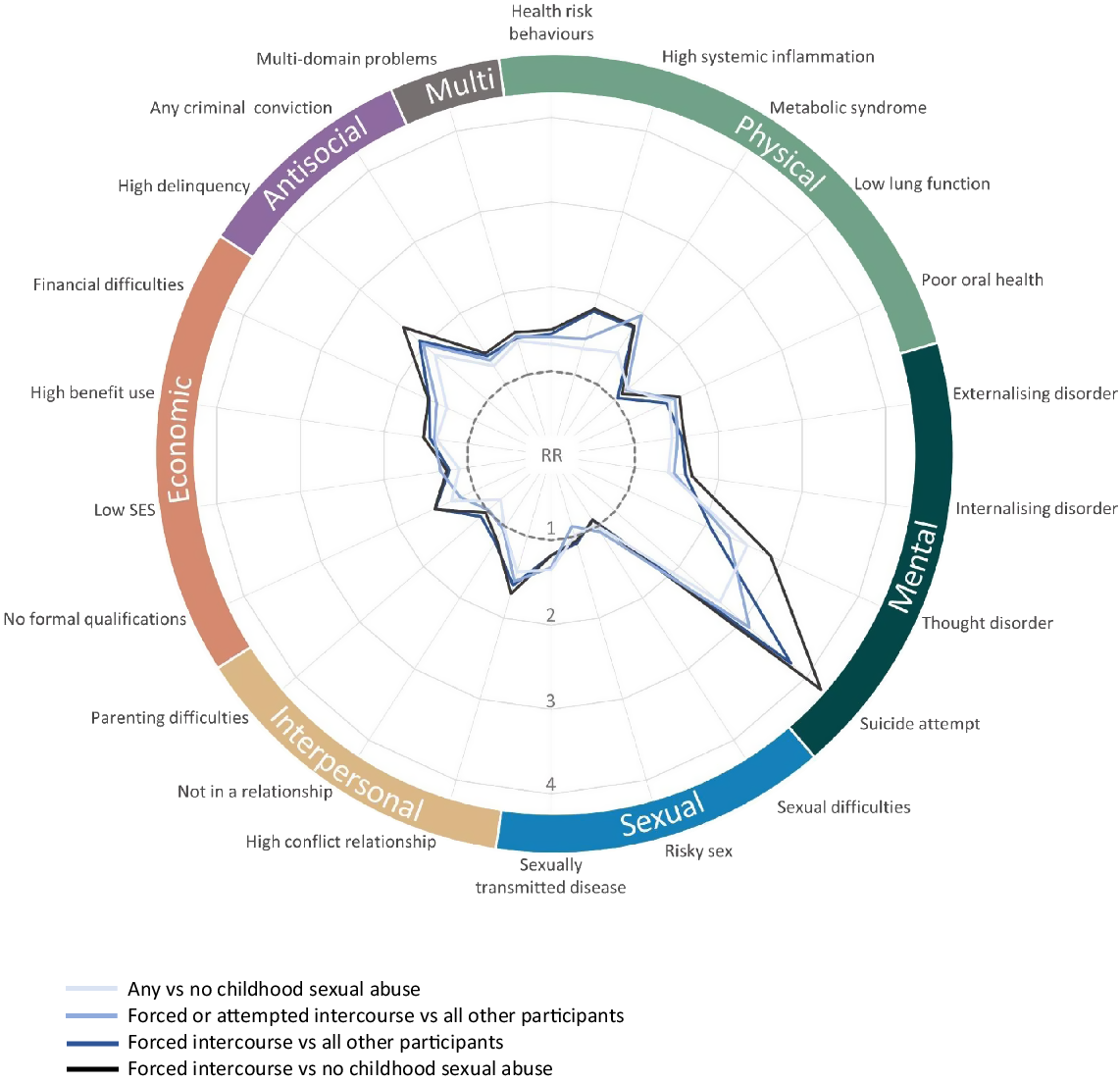
Figure 3. Adjusted group differences in the prevalence of problems across adulthood by different definitions of childhood sexual abuse. Relative risks from the regression models including all control variables (sex, childhood socioeconomic status, child harm and household dysfunction adverse childhood experiences, and sexual assault in adulthood) are shown. A relative risk of 1 (dashed line) indicates no difference by childhood sexual abuse; points further from the center indicate a higher relative risk.
Table 4. Relationships between different definitions of childhood sexual abuse exposure and problems across adulthood
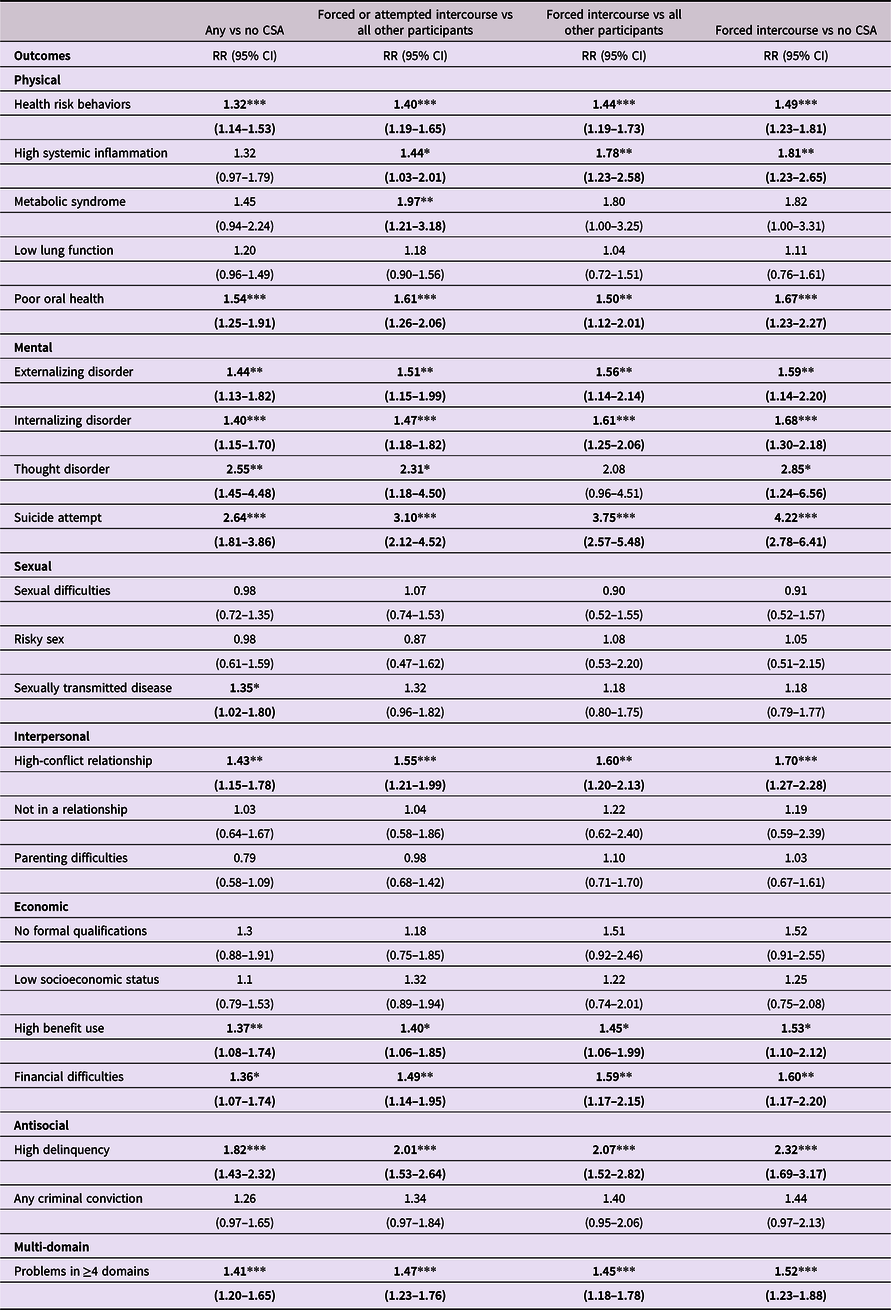
Notes. CSA = childhood sexual abuse. Relative risks (RRs) and 95% confidence intervals indicate group differences between the exposure and comparison groups (always the reference group) after adjusting for all control variables (sex, childhood socioeconomic status, child harm adverse childhood experiences, household dysfunction adverse childhood experiences, and sexual assault in adulthood). Bolded text indicates statistically significance. *p < 0.05, **p < 0.01, ***p < 0.001.
The second point to note is that where differences between definitions of CSA in the observed effect sizes were evident, they tended to reflect differences in the relative severity of CSA between the exposed and comparison groups. For example, the observed relative risks tended to be larger for the analyses that focused on forced intercourse than those that focused on any CSA, and larger for the forced intercourse versus no CSA analyses than the more conservative analyses that compared those who reported forced intercourse to all other participants (i.e., including those who experienced less severe types of CSA such as genital touching or attempted intercourse).
Discussion
In this longitudinal study, CSA was associated with problems across multiple domains of functioning from young adulthood to midlife. After adjusting for prospectively measured confounding factors, participants who reported CSA were more likely than their peers to have problems across adulthood in the following domains: physical (health risk behaviors, high systemic inflammation, and poor oral health), mental (internalizing disorder, externalizing disorder, thought disorder, and suicide attempts), sexual (sexually transmitted diseases), interpersonal (high-conflict relationships), economic (benefit use and financial difficulties), antisocial (high delinquency), and cumulative problems in multiple life domains. The pattern of findings was consistent across different CSA definitions, with small to moderate effect sizes (albeit large for lifetime suicide attempts) that incremented with CSA severity.
Against the overall picture of higher risk for problems in multiple domains across adulthood, participants who reported CSA were not significantly more likely than their peers to have low lung function, lack of formal qualifications, low socioeconomic status, and criminal convictions in adulthood after adjusting for all control variables (sex, childhood socioeconomic status, child harm and household dysfunction ACEs, and sexual assault in adulthood). The stepwise analyses are informative here. After adjusting for sex only, CSA was associated with those four outcomes, but after further adjusting for childhood socioeconomic status, CSA was no longer significantly associated with low lung function, lack of formal qualifications, or low socioeconomic status. After adjusting for household dysfunction ACEs, CSA was no longer significantly associated with criminal convictions. These findings indicate that some CSA-outcome links might be better explained by other coinciding adversities, and underscore the importance of adjusting for prospectively measured covariates in CSA outcomes research. Nonetheless, practitioners will of course note that while separating out the effects of other life stressors that often coincide with CSA is important for research purposes, coinciding stressors cannot in reality be separated from a person’s experience.
We also did not find statistically significant associations between CSA and sexual difficulties, risky sex, lack of intimate relationships, and parenting difficulties, even before other control variables were taken into account. These nonsignificant findings could indicate no meaningful relationships with CSA, or that the measures used in the current study were unable to detect them. Guidance from the previous literature is limited as findings on the relationships between CSA and sexual outcomes, and between CSA and parenting, are mixed and often depend on how the sample was selected (Bigras et al., Reference Bigras, Vaillancourt-Morel, Nolin and Bergeron2020; Greene et al., Reference Greene, Haisley, Wallace and Ford2020). It is possible that associations between CSA and sexual outcomes are more evident earlier or later than our study period from age 26 to 45 years. Consistent with this idea, previous Dunedin Study research showed stronger CSA-related differences in sexual health at age 18 to 21 years than 26 to 32 years (van Roode et al., Reference van Roode, Dickson, Herbison and Paul2009), and in the current study we saw CSA-related differences in sexual difficulties at age 45 years only. Nonetheless, these findings do not preclude the possibility of more nuanced links between CSA and sexual outcomes, or CSA and later parenting, that future longitudinal research could examine.
Strengths and limitations
Four factors strengthen the current findings. First, the high retention rate (94% of living study members participated at age 45) and study design features (e.g., population-based birth cohort, predominantly prospective data, regular follow-ups over the life course, consistent high quality biopsychosocial measures, controls for other stressors) help to rule out some of the alternative explanations for the findings. Second, we repeated our analyses using different definitions of CSA and showed consistent patterns of effects that varied according to severity in expected ways: a pattern that is consistent with other similar studies, including the Christchurch Health and Development Study (Fergusson et al., Reference Fergusson, McLeod and Horwood2013). Third, our supplementary analyses showed that the overall pattern of findings was consistent across linear as well as binary outcome measures, and four separate ages in adulthood. Finally, the multidisciplinary, long-duration approach using consistent measures across adulthood helped mitigate problems associated with differences in definition and design that those seeking to synthesize the literature lament (Hailes et al., Reference Hailes, Yu, Danese and Fazel2019).
It is also important to note the current study’s limitations. First, the relatively small numbers in the exposed groups meant that we could not adequately test whether CSA effects were different for males and females, and that some potentially meaningful effects (see Figure 2) were not statistically significant. Second, the findings are based on a specific cohort born in New Zealand in the early 1970s, and may not generalize to other cultures or birth cohorts. However, our findings are consistent with CSA outcomes research in other populations, and our cohort’s mental and physical health characteristics align with those in nationally representative samples (Caspi et al., Reference Caspi, Houts, Ambler, Danese, Elliott, Hariri and Moffitt2020; Poulton et al., Reference Poulton, Hancox, Milne, Baxter, Scott and Wilson2006). Moreover, the prevalence of CSA in this study was similar to that in comparable New Zealand studies that included people of the same generation as Dunedin Study members. The overall CSA prevalence was 19% in this study, and 14% in another longitudinal study started in Christchurch, New Zealand in 1977 (Fergusson et al., Reference Fergusson, McLeod and Horwood2013). Similarly, CSA prevalence among females in this study was 30%, and 24 to 27% in population-level surveys that included New Zealand women born between 1971 and 1980 (Fanslow et al., Reference Fanslow, Hashemi, Gulliver and McIntosh2021).
Third, although all other measures were collected prospectively, exposure to CSA was recorded retrospectively at age 26 years. Research comparing prospective and retrospective reports of childhood maltreatment in the same sample has shown that the two methods identify largely distinct groups of people: a significant proportion of people with prospectively documented evidence of child maltreatment do not later report it, and a significant proportion of those who retrospectively report child maltreatment do not have corroborating prospective records (Baldwin et al., Reference Baldwin, Reuben, Newbury and Danese2019; Danese & Widom, Reference Danese and Widom2020; Latham et al., Reference Latham, Quilter, Arseneault, Danese, Moffitt, Newbury and Fisher2021; Najman et al., Reference Najman, Kisely, Scott, Strathearn, Clavarino, Williams and Bernstein2020). This evidence has led to questions about the veracity of retrospective reports of childhood maltreatment (Widom, Reference Widom2019), but it is important to note that both prospective and retrospective methods have features that can lead to under- and over-reporting (discussed in Baldwin et al., Reference Baldwin, Reuben, Newbury and Danese2019). In this study of retrospectively reported CSA, we cannot not rule out the possibility that recall or reporting biases influenced the results. However, there are some factors that increase confidence in the data analyzed here. For example, we observed relationships between CSA and objectively measured outcomes as well as self-reported ones, helping to avoid issues with common method variance. We were also able to use information about CSA exposure type to assess how the pattern of results varied by relative severity, and found that it consistently reflected that severity. Moreover, our secondary analyses used a conservative approach that included those who reported a less severe CSA exposure in the unexposed group (e.g., forced intercourse versus all other participants, including those who reported attempted intercourse or genital touching), showing a consistent pattern of effects even when misclassification into abuse groups was likely. Nonetheless, no currently available measure of CSA in a population research setting (whether prospective or retrospective) can provide precise and correct identification of all cases and exclusion of all inaccurate reports. Thus, the results here are best described as providing evidence that CSA retrospectively reported in young adulthood is associated with multiple problems across life domains and across adulthood.
The fourth limitation is that while this omnibus study provides an overview of a range of problems in adulthood, outcomes were largely limited to those that were consistently and repeatedly assessed from age 26 to 45 years. There may be other important outcomes that researchers have considered more recently (e.g., neurological functioning; Blanco et al., Reference Blanco, Nydegger, Camarillo, Trinidad, Schramm and Ames2015), and others still that can only be assessed when study members are older (e.g., heart failure; dementia). Finally, the current findings do not elucidate the likely complex mechanisms by which CSA could lead to problems in multiple domains across adulthood.
Implications
Despite these limitations, replicating the current findings in different longitudinal samples and with different measures of CSA is likely to have important implications for policy and practice. Evidence that CSA is a risk factor for cumulative problems in multiple life domains across adulthood, not just mental health, is likely to be important for informing the work of agencies tasked with developing compensation and support frameworks for CSA survivors (e.g., commissions of inquiry; government agencies; insurance companies). Such evidence would also underscore the value of early interventions that might help to prevent the wide range of possible long-term outcomes and ultimately improve adult wellbeing (Cummings et al., Reference Cummings, Berkowitz and Scribano2012), support the inclusion of multiple domains of functioning into assessment and treatment, and encourage specialists to implement coordinated care across professions to ensure survivors have an appropriate support network.
There is an ongoing question in the literature whether CSA causes adverse outcomes (Hailes et al., Reference Hailes, Yu, Danese and Fazel2019). Causation cannot be inferred from the current findings, but they nevertheless indicate that many associations between CSA and adverse long-term outcomes were not explained by other major childhood risk factors that often coincide with CSA, including socioeconomic adversity and other ACEs (Danese, Reference Danese2020). Our findings are also consistent with the idea that childhood maltreatment is likely to contribute to poor biopsychosocial outcomes via the downstream effects of chronic stress and maladaptive coping behaviors (Cicchetti & Toth, Reference Cicchetti and Toth2004; Danese, Reference Danese2020). Alongside previous research, the current findings support the hypothesis that CSA is likely to contribute, whether directly or indirectly, to a range of adverse outcomes in adulthood (Chartier et al., Reference Chartier, Walker and Naimark2009; Nelson et al., Reference Nelson, Heath, Madden, Cooper, Dinwiddie, Bucholz and Martin2002; Power et al., Reference Power, Li and Pinto Pereira2020). Future research should seek to explain the likely complex and interactive causal mechanisms across the lifecourse that could account for the multiplicity and persistence of problems associated with retrospectively reported CSA.
Beyond efforts to get as close as possible to understanding the causal links between CSA and later outcomes, the main challenge for future research is to produce good quality evidence that can be used to develop policies and interventions to help survivors and reduce the health and wellbeing burden associated with CSA. Prospective longitudinal studies should seek to develop measures of CSA that are both sensitive and specific, and identify modifiable factors that differentiate CSA survivors who do not experience specific problems across adulthood from those who do, with a view to identifying "preventive pathways," including behavioral and psychosocial targets for intervention (Domhardt et al., Reference Domhardt, Munzer, Fegert and Goldbeck2015). Building on our findings up to midlife that show higher prevalence of risk factors for later age-related disease (e.g., smoking, Ambrose & Barua, Reference Ambrose and Barua2004; systemic inflammation, Pearson et al., Reference Pearson, Mensah, Alexander, Anderson and Cannon2003; mental disorders, Richmond-Rakerd et al., Reference Richmond-Rakerd, D’Souza, Milne, Caspi and Moffitt2021) among participants who reported CSA, further research into the latter half of the lifecourse will provide better information about the relationship between CSA and accelerated aging, and potential mitigations. Finally, econometric studies that describe the breadth and persistence of problems associated with CSA in terms of real public health costs may help to further facilitate the introduction of comprehensive CSA prevention policies (Letourneau et al., Reference Letourneau, Brown, Fang, Hassan and Mercy2018).
Conclusion
This study aimed to determine the extent of the links between CSA and adverse outcomes across multiple life domains, how strong those links are, and whether they are evident across adulthood. Using population-based longitudinal data and a comprehensive set of outcomes repeatedly assessed from young adulthood to midlife, this study indicates that retrospectively reported CSA is a risk factor for problems across multiple life domains, and that these problems can persist across the 20s, 30s, and well into the 40s. Consistent with the large body of existing literature (Fergusson et al., Reference Fergusson, McLeod and Horwood2013; Hailes et al., Reference Hailes, Yu, Danese and Fazel2019), the higher risk for most specific problems was small to moderate, but taken together, the cumulative risk over a long period and across multiple domains reflect considerable individual and societal burden.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579422001146
Acknowledgements
We thank the Dunedin Multidisciplinary Health and Development Study members, Unit research staff, and Study founder Dr Phil Silva, and University of Otago. The Dunedin Multidisciplinary Health and Development Research Unit is based at University of Otago within the Ngāi Tahu tribal area who we acknowledge as first peoples, tangata whenua, of this land.
Funding statement
The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council and New Zealand Ministry of Business, Innovation and Employment. This research was also funded by National Institute on Aging grant nos. R01AG032282 and R01AG049789, and the UK Medical Research Council grant no. MR/P005918/1.
Conflicts of interest
The authors have no competing interests to declare.












