Iodine is an essential micronutrient of the thyroid hormone. Both insufficient and excessive iodine intake can cause thyroid hormone disorders. Iodised salt has been widely distributed in many countries including China to prevent disorders caused by iodine deficiency. However, excessive iodine intake may cause thyroid goitre, overt hyper- and hypothyroidism, subclinical hyper- and hypothyroidism, autoimmune thyroid disease, iodine allergies and iodine poisoning, loss of intelligence, etc.(Reference Yu, Zhu and Chen1–Reference Liu, Lam and Zeng5). Sources of iodine are naturally found in food and water. Japan was the first country to discover food-source goitre in the world about 40 years ago. Suzuki et al. (Reference Suzuki, Higuchi and Sawa6) reported that Hokkaido fishermen had a high prevalence of goitre because of over-consumption of seaweed, and school-aged children had a prevalence of 6·8–8·9 %. After this report in Japan, China also reported iodine-excess goitre cases in 1980(Reference Yu and Ma7). These cases were related to over-eating ‘kelp salt’, which contained iodine levels as high as 226·5–1382 mg/kg. Zimmermann et al. (Reference Zimmermann, Ito and Hess8) also found that high dietary intakes of iodine in children result in high thyroid volume.
China was the first country to report water-source iodine-excess goitre cases. A high prevalence of goitre was found among fisherman in Hebei Province in the 1970s. Following these findings, a series of epidemiological and clinical investigations and animal experiments were conducted in the province. Zhao et al. (Reference Zhao, Guo and Yu9) reported that water iodine level was very high, i.e. 661·2 μg/l in a deep well (about 600–700 m), and goitre was more prevalent among 4344 fishermen who drank the water compared with those who did not (28·36 v. 8·37 %). Between 1984 and 2003, other provinces in China also reported water-related iodine-excess goitre cases. Goitre prevalence was from 10·84 to 73 %, and median urinary iodine was from 586·7 to 2428·5 μg/l(Reference Yu, Zhu and Chen10, Reference Liu, Zhao and Zhang11). Zhao et al. (Reference Zhao, Wang and Shang12) studied 2471 individuals in twelve towns of the Jiangsu Province, China, and reported that townships with a higher median level of iodine in well water had a higher median urinary iodine concentration, prevalence of goitre and abnormal thyroid volume.
Iodine-deficiency disorder has been primarily controlled in China through widely providing iodised salt. With this prevention strategy, the challenge is how to prevent goitre in populations who reside in areas with high levels of iodine in drinking-water. Therefore, we conducted a Chinese national investigation to identify the geographical distribution of drinking-water with high iodine levels in China. We conducted physical measurements for goitre and urinary iodine among children aged 8–10 years to determine the relationship between high iodine levels in drinking-water and goitre prevalence.
Experimental methods
Water sample collections and iodine level measurement
We included all 129 counties that were suspected to have high levels of water iodine in eleven provinces (i.e. Anhui, Beijing, Fujian, Hebei, Henan, Jiangsu, Inner Mongolia, Shandong, Shanxi, Tianjin and Xinjiang), based on previous investigations and results of national iodine-deficiency disorder monitoring. In these counties, each of the 1978 towns was divided into five districts (i.e. east, west, south, north and centre). From each district, one village was randomly selected. For villages with less than five wells, we collected water samples from all available wells. For those with more than five wells, the village was divided into five areas (i.e. east, west, south, north and centre), and one well was randomly selected from each area for those with more than one well. In the village where water was provided through pipelines, we collected a sample from the source of the water supply. In total, we collected 28 857 water samples from the 1978 towns. In addition to high iodine content, drinking-water in these areas meets China Standards for Drinking Water Quality.
Water samples were stored in 50 ml plastic bottles and kept in a refrigerator maintained at 4°C. The bottles were washed twice with water samples before sampling. Iodine level was examined within a week after the sample collection. Water iodine was determined using the As–Ce catalytic spectrophotometric method for high water iodine. Considering the high level of iodine in the water samples, we adopted the China Iodine Deficiency Disorder Laboratory standard for iodine measurement. Validity of the measurement was assessed using standardised samples from the China External Quality Control.
Physical measurement for determining goitre
Study population
Based on the analysis of water iodine levels, the towns were categorised into three groups: those with median water iodine < 150, 150–300 and >300 μg/l. The categories were determined by the national standard ‘Determination and Classification of the Areas of High Water Iodine and the Endemic Areas of Iodine Excess Goiter’(Reference Liu, Zhao and Zhu13), stating that iodine goitre is more likely to occur in areas with median water iodine >300 μg/l, uncertain in areas with 150–300 μg/l and less likely to occur in areas with < 150 μg/l.
Due to limited financial and time resources, physical measurement for goitre was conducted among children aged 8–10 years during 2005 and 2006, mainly in towns with a median water iodine of 150–300 μg/l and in some towns with median water iodine >300 μg/l. Towns with median water iodine < 150 μg/l were not included. A total of 277 towns with iodine levels of 150–300 μg/l and twenty-two towns with iodine levels >300 μg/l were randomly selected from nine provinces (i.e. Anhui, Beijing, Hebei, Henan, Jiangsu, Inner Mongolia, Shandong, Shanxi and Tianjin).
Each town was divided into five districts (i.e. east, south, west, north and centre). In each district, one primary school was randomly selected if there was more than one school. From each primary school, forty children (twenty boys and twenty girls) aged 8–10 years were randomly selected to examine the thyroid. For those schools with less than forty students aged 8–10 years, all were included.
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Ethics Committee of the Center for Endemic Disease Control, Chinese Center for Disease Control and Prevention. Verbal informed consent was obtained from all subjects, and the consent was witnessed by teachers and formally recorded by investigators.
Goitre determination and urine iodine level measurement
Physicians who were working at provincial and municipal centres for disease control examined the randomly selected children. All physicians had been working at the Centre for Disease Control, specifically for domestic disease diagnosis and treatment. Therefore, they had rich experience in examining the thyroid. Before the study, the physicians were further trained and examined some children in order to reduce physician variation in identifying goitre. Examination was made by two physicians, separately; when the results were inconsistent, they would reconsider. The diagnosis was made based on the Chinese national standard ‘diagnostic criteria for endemic goiter’(Reference Liu, Chen and Jia14) and WHO/UNICEF/ICCIDD(15)-recommended criteria. Because of limited budget, goitre in 56 575 children in 299 towns was determined by palpation. We identified children with goitre through measuring thyroid volume by ultrasound among 1413 children in fifteen towns of Tianjin. Goitre prevalence identified by ultrasound was similar to that identified by palpation, 10·33 and 11·25 %, respectively.
Goitre is graded according to the following classification:
Grade 0: no palpable or visible goitre.
Grade 1: a goitre that is palpable but not visible when the neck is in the normal position (i.e. the thyroid is not visibly enlarged). (A thyroid gland will be considered goitrous when each lateral lobe has a volume greater than the terminal phalanx of the thumbs of the subject being examined.) Thyroid nodules in a thyroid, which is otherwise not enlarged, fall into this category.
Grade 2: a swelling in the neck that is clearly visible when the neck is in a normal position and is consistent with an enlarged thyroid when the neck is palpated.
It is recommended that a total goitre rate (number with goitres of grades 1 and 2 divided by total number examined) of 5 % or more in schoolchildren 6–12 years of age be used to signal the presence of a public health problem.
From the participants, we collected the middle portion of the urine (not less than 5 ml) in dry and clean polyethylene or glass tubes, sealed tightly to prevent evaporation. The urine samples were stored in a refrigerator maintained at 4°C and analysed within 1 month. Urinary iodine was determined in accordance with the China health standard ‘Method for determination of iodine in urine by As3+–Ce4+ catalytic spectrophotometry’(Reference Yan, Zhang and Liu16). Validity of measurement was assessed using the quality-control samples from the China External Quality Control.
The WHO/UNICEF/ICCIDD(15) have recommended the following epidemiological criteria for assessing iodine nutrition based on median urinary iodine concentrations in school-aged children: < 100 μg/l, insufficient; 100–199 μg/l, adequate; 200–299 μg/l, above requirements; ≥ 300 μg/l, excessive.
Statistical analyses
Descriptive statistics were employed to describe the geographical distribution. The Spearman rank correlation was used for testing the correlation between goitre and water iodine and urine iodine levels. The relative risk (RR) for goitre was calculated across urinary iodine levels.
Results
There were 488 towns with a median water iodine of 150–300 μg/l and 246 towns with a median water iodine >300 μg/l. These towns were mainly located in the middle of China (Fig. 1). Based on local population reports, 18·87 million resided in areas with water iodine levels of 150–300 μg/l and 12·11 million resided in areas with water iodine >300 μg/l.
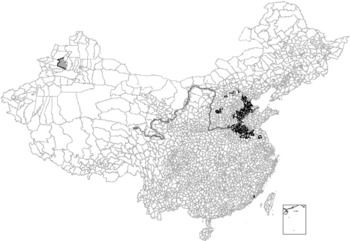
Fig. 1 Geographical distribution of drinking-water iodine (WI) in China. ![]() , WI ≥ 300 μg/l (n 64);
, WI ≥ 300 μg/l (n 64); ![]() , 150 ≤ WI < 300 μg/l (n 44);
, 150 ≤ WI < 300 μg/l (n 44); ![]() , WI < 150 μg/l (n 21);
, WI < 150 μg/l (n 21); ![]() , Yellow River.
, Yellow River.
Goitre prevalence was 6·33 and 11·03 % among children who resided in towns with a median water iodine of 150–300 and >300 μg/l, respectively (Table 1). The prevalence varied across provinces, ranging from 1·22 to 14·35 %.
Table 1 Goitre prevalence and median urine iodine across provinces in China among children aged 8–10 years
(Median values, number of towns, children and goitres, and percentages)
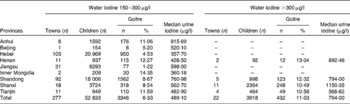
Table 2 and Fig. 2 show the correlation between median water iodine and goitre prevalence. Goitre prevalence increased with the increase in median water iodine. For example, goitre prevalence was 6·24 % in the districts with a median water iodine of 150–199 μg/l, which was much lower than 15·81 % in the district with median water iodine >500 μg/l.
Table 2 Relationship between water iodine, urine iodine, and goitre prevalence among children aged 8–10 years
(Median values, number of towns, children and goitres, and percentages)
Fig. 2 Relationship of water iodine (WI) level and goitre prevalence among children aged 8 to 10 years. TGR, thyroid goitre prevalence.
Table 2 also shows the inter-relationship between water iodine level, urine iodine level and goitre prevalence. Urine iodine level increased with the increase in water iodine level. Goitre prevalence increased with the increase in water iodine and urine iodine levels.
We analysed the relationship between goitre prevalence and median urine iodine. For children with a median urine iodine of 300–399 μg/l, goitre prevalence was 5·16 %, which was slightly higher than the national standard of 5 %(Reference Zhang, Chen and Ge17) and WHO/UNICEF/ICCIDD-recommended criteria(15). Compared with goitre prevalence among children with urine iodine of 100–199 μg/l, the RR for goitre increased with the increase in urine iodine: 1·56 for those with urine iodine of 300–399 μg/l; 2·27 for those with urine iodine of 600–699 μg/l; 3·46 for those with urine iodine of 900–999 μg/l; 3·69 for those with urine iodine of >1500 μg/l.
Discussion
This Chinese national investigation demonstrated that high iodine in drinking-water was found in eleven provinces out of thirty-one in China. Approximately 31 million people are living in these high water iodine areas. Seven provinces (Shandong, Hebei, Henan, Tianjin, Jiangsu, Anhui and Shanxi) had extremely high levels of iodine in their drinking-water. We also found that goitre prevalence was correlated with the iodine level in drinking-water and urine among children.
There are three possible reasons for the geographical distribution of high levels of iodine in drinking-water. One possible reason is that the Yellow River caused iodine deposits in the areas through several divesting floodings. The second longest river in China originates in Qinghai Province, in western China, and ends at the Bohai Sea. Currently, the river flows through nine provinces of China, including two high drinking-water iodine provinces of Shandong and Henan. The river has flooded numerous times due to its low basin and has changed its main course a few times historically. High drinking-water iodine areas of Hebei, Jiangsu, Anhui, Tianjin and Beijing used to be courses of the river at some point in time in the past. The distribution indicated that high levels of iodine might be caused by the sediment-laden river. Another possible reason is that changes in the sea coast resulted in iodine being deposited inland. Bohai and Huang Huai Seas are rich in iodine, and their coast lines have changed several times. Each change has left iodine in the land. The third possible reason is that iodine was leached or eroded down to a low-lying area inland, which was accumulated in the specific area due to a poor drainage system, such as the Shanxi Province.
A cause of goitre is iodine deficiency or excess. In our sample, goitre prevalence was correlated with the level of iodine in drinking-water (correlation coefficient 0·93), and increased with urinary iodine levels. Our analysis of urine iodine further supports that excess iodine contributes to goitre. Goitre prevalence was above 5 % among children with a median urine iodine of 300–399 μg/l. This supports the WHO/UNICEF/ICCIDD's cut-off point of excessive iodine intake (i.e. median urine iodine >300 μg/l). WHO/UNICEF/ICCIDD(15) have recommended that iodine nutrition was optimal when median urine iodine was 100–200 μg/l. So taking total goitre rate at the time of median urine iodine of 100–200 μg/l as a standard, we calculated the RR of suffering from goitre for children aged 8–10 years with different urinary iodine levels. The RR was more than 1·5 times when median urine iodine was >300 μg/l. The strength of association reached the middle class. The RR was more than 3·0 times when median urine iodine was >900 μg/l. The strength of association reached the strong class. To prevent iodine-deficiency disorders, iodised salt (35 ± 15 parts per million iodine; mean ± 2 sd) has been provided nationally since 1995, including the areas with a high level of iodine in drinking-water. Therefore, iodised salt (may have) facilitated goitre occurrence rather than prevented the disease in areas with high levels of iodine in the water. The present study mapped the geographical distribution of high iodine in drinking-water in China. Based on these findings, the following three preventive recommendations have been provided to the Chinese government: (1) to stop and eliminate the sale of iodised salt in these areas; (2) to change drinking-water and provide pipeline water with an appropriate amount of iodine; (3) monitor drinking-water iodine and goitre occurrence.
The present study has four limitations. First, we conducted this investigation in eleven provinces based on sporadic reports on water iodine level. We may have missed some districts with high levels of iodine in drinking-water. Second, our investigation focused mainly on districts with water iodine levels of 150–300 μg/l, and only sampled a few towns with water iodine levels >300 μg/l. Third, some residents in high water iodine districts took iodised salt when we conducted this survey. This might have confounded the effect of water iodine on goitre occurrence. Fourth, we did not assess the agreement among the physicians who conducted the physical examination for detecting goitre. However, we controlled face validity through extensive training.
Despite these limitations, this large Chinese national investigation on water iodine and goitre identified districts with high iodine in drinking-water and demonstrated the relationship between water iodine and goitre prevalence. Our findings provide evidence to prevent goitre in these areas.
Acknowledgements
This survey was supported by grant from the China Ministry of Health. Thanks are extended to the many people who participated in the investigation, including physicians, children, teachers and government staff. The authors declare that there is no conflict of interest. The contribution of each author was as follows: H. S. participated in the planning of the study, supervision of the investigation, collecting of the data and interpretation of the results. S. L. and D. S. participated in the planning of the study, supervision of the investigation and interpretation of the results. S. Z. and X. S. participated in the supervision of the investigation and collecting the data. Y. S. and H. H. participated in the collection of the data.








