AUDs are prevalent (SAMHSA, 2019), affecting about 30% of individuals aged 18 or older in the United States (Grant et al., Reference Grant, Goldstein, Saha, Patricia Chou, Jung, Zhang, Pickering, June Ruan, Smith, Huang and Hasin2015) and associated with significant personal, interpersonal, and societal costs (Sacks et al., Reference Sacks, Gonzales, Bouchery, Tomedi and Brewer2015). Initiation of alcohol use typically occurs in adolescence, and early onset alcohol use (age 14 or younger), in particular, has been associated with prolonged negative outcomes including increased risk for AUD (Gruber et al., Reference Gruber, Diclemente, Anderson and Lodico1996; Hingson et al., Reference Hingson, Heeren and Winter2006; Hingson & Zha, Reference Hingson and Zha2009), in part due to influences on the developing brain (Spear, Reference Spear2018; Squeglia et al., Reference Squeglia, Jacobus and Tapert2014). Thus, understanding the etiology of adolescent alcohol use is important to inform early prevention and intervention. There is strong evidence that both genetic predispositions and social environments contribute to alcohol use problems, and that genetic influences vary as a function of environmental experiences (i.e., gene–environment interaction; G×E), and vice versa (Dick & Kendler, Reference Dick and Kendler2012; Enoch, Reference Enoch2012). However, prior genetically informative research has primarily focused on alcohol use outcomes among adolescents and adults who have already initiated alcohol use or developed AUD, limiting our understanding about how genetic risk for AUD unfolds across development. In the present study, we took a developmental approach to examine how genetic risk of AUD influences early precursors of alcohol use (i.e., childhood impulsivity) and how familial contextual factors (i.e., parenting and family conflict) moderate genetic risk. By shifting the focus from problematic alcohol use to childhood precursors or intermediate phenotypes that underlie alcohol use and AUD, such as impulsivity, we can better understand how genetic risk of AUD manifests earlier in development (Dick et al., Reference Dick, Barr, Cho, Cooke, Kuo, Lewis, Neale, Salvatore, Savage and Su2018), which can inform early prevention and intervention before alcohol use even begins.
Genetic risk of AUD and childhood impulsivity
Alcohol use and AUD are complex behavioral outcomes best understood from a developmental perspective (Trucco & Hartmann, Reference Trucco and Hartmann2021). Developmental cascade models depict adolescent alcohol and substance use as a result of a sequential progression from temperamental differences in childhood (e.g., impulsivity, behavioral control) to problem behaviors in early adolescence to riskier behaviors, such as alcohol and drug use during mid/late-adolescence, with this cascade sequence thought to be initiated by genetic and biologically based differences (Dodge et al., Reference Dodge, Malone, Lansford, Miller, Pettit and Bates2009). Accordingly, temperament traits such as childhood impulsivity are considered important early precursors of alcohol use and AUD.
We focus on examining the influence of genetic risk for AUD on childhood impulsivity as an early precursor and prime intermediate phenotype for AUD for several reasons. First, impulsivity is a robust predictor of alcohol use outcomes, with extensive literature linking impulsivity to alcohol use and problems in human studies and animal models (Coskunpinar et al., Reference Coskunpinar, Dir and Cyders2013; Dick et al., Reference Dick, Smith, Olausson, Mitchell, Leeman, O’Malley and Sher2010). Prospective studies show that impulsivity in childhood predicts alcohol use in adolescence and adulthood (Elam et al., Reference Elam, Wang, Bountress, Chassin, Pandika and Lemery-Chalfant2016; Pedersen et al., Reference Pedersen, Molina, Belendiuk and Donovan2012) and the development of AUD (Clark et al., Reference Clark, Vanyukov and Cornelius2002; Dawes et al., Reference Dawes, Tarter and Kirisci1997). Second, impulsivity shares genetic etiology with alcohol phenotypes. Twin studies indicate that a variety of different disorders that are characterized by impulsive behavior, including alcohol and drug dependence, childhood conduct disorder, and adult antisocial behavior, overlap largely due to an underlying shared genetic liability (Kendler et al., Reference Kendler, Prescott, Myers and Neale2003). Personality traits related to impulsivity also load on this latent genetic factor (Krueger et al., Reference Krueger, Hicks, Patrick, Carlson, Iacono and McGue2002; Young et al., Reference Young, Stallings, Corley, Krauter and Hewitt2000), which has been referred to interchangeably as behavioral disinhibition, behavioral undercontrol, or impulsivity. A recent study with a sample of college students showed that impulsivity dimensions, as measured by the UPPS-P scale (Cyders et al., Reference Cyders, Smith, Spillane, Fischer, Annus and Peterson2007), mediate the relation between alcohol use genome-wide polygenic scores (PRS) and alcohol consumption (Ksinan et al., Reference Ksinan, Su, Aliev and Dick2019), suggesting that impulsivity may be a manifestation of a genetic risk for alcohol use problems. Furthermore, prior research suggests that impulsivity and related traits are modifiable by interventions (Hentges et al., Reference Hentges, Weaver Krug, Shaw, Wilson, Dishion and Lemery-Chalfant2020), making them promising targets for early interventions aimed at reducing long-term risk of AUD.
Impulsivity is a multidimensional construct that has been conceptualized and measured in various ways, including the use of questionnaires and laboratory tasks (Dick et al., Reference Dick, Smith, Olausson, Mitchell, Leeman, O’Malley and Sher2010). In an effort to address the lack of consensus in the literature and integrate different approaches to impulsivity, researchers developed the UPPS-P model, which operationalizes impulsivity as five related but distinct dimensions, including negative urgency (i.e., tendency to act rashly when experiencing negative emotions or affect), positive urgency (i.e., tendency to act rashly as a result of positive affect), lack of premeditation (i.e., lack of careful thinking and planning before action), lack of perseverance (i.e., inability to remain with a task or see it finished), and sensation seeking (i.e., the tendency to seek out excitement and adventure) (Cyders et al., Reference Cyders, Smith, Spillane, Fischer, Annus and Peterson2007; Whiteside & Lynam, Reference Whiteside and Lynam2001). Each dimension has been related to alcohol use outcomes and other forms of externalizing behavior (e.g., aggression) (Berg et al., Reference Berg, Latzman, Bliwise and Lilienfeld2015). Some of the dimensions, most strongly negative urgency, have also been associated with depression and anxiety (Berg et al., Reference Berg, Latzman, Bliwise and Lilienfeld2015). Thus, differences in aspects of impulsivity may represent core underlying processes contributing to both the externalizing and internalizing pathways that have consistently been associated with the development of alcohol problems in the literature (Hussong et al., Reference Hussong, Jones, Stein, Baucom and Boeding2011; Zucker et al., Reference Zucker, Donovan, Masten, Mattson and Moss2008). Therefore, characterizing genetic and environmental processes in relation to impulsivity is critical to inform prevention and intervention efforts aimed at reducing alcohol problems.
G×E: The role of parenting and family environment
Bronfenbrenner’s bioecological model (Bronfenbrenner & Morris, Reference Bronfenbrenner and Morris2007) emphasizes the importance of the interactions between person-level characteristics (e.g., genetics) and social contexts in shaping human development. Family is one of the most important microsystems or immediate social environments that influences child development. Indeed, numerous studies have linked specific parenting behaviors, as well as the overall family environment, to child outcomes. For example, parenting behaviors such as parental monitoring and acceptance have been associated with lower levels of alcohol use among adolescents (Nash et al., Reference Nash, McQueen and Bray2005; Webb et al., Reference Webb, Bray, Getz and Adams2002). Parental monitoring may lead parents to be more aware if their child begins engaging in or socializing with peers who engage in alcohol use (Branstetter & Furman, Reference Branstetter and Furman2013; Soenens et al., Reference Soenens, Vansteenkiste, Luyckx and Goossens2006). Parents with greater knowledge of their child’s lives may be more successful in influencing their adolescent’s friend group and restricting access to alcohol (Bountress et al., Reference Bountress, Chassin and Lemery-Chalfant2017). Parental acceptance has been associated with less drinking, decreased stress, and fewer alcohol-related problems in adolescence (Nash et al., Reference Nash, McQueen and Bray2005). Similarly, parenting behaviors characterized by high warmth and acceptance have been linked to higher self-control and lower impulsivity among children and adolescents (Brody et al., Reference Brody, Murry, McNair, Chen, Gibbons, Gerrard and Wills2005; Conway, Reference Conway2020; Eisenberg et al., Reference Eisenberg, Zhou, Spinrad, Valiente, Fabes and Liew2005). The emotional climate in the family environment, such as family conflict, has also been associated with alcohol use and related outcomes (Baer et al., Reference Baer, Garmezy, McLaughlin, Pokorny and Wernick1987; Bray et al., Reference Bray, Adams, Getz and Baer2001). Family conflict may contribute to both internalizing and externalizing problems among adolescents, which in turn can increase risk for problematic alcohol use (Chan et al., Reference Chan, Kelly and Toumbourou2013; Timmons & Margolin, Reference Timmons and Margolin2015). Previous studies and meta-analysis demonstrate that family conflict predicts lower self-control among adolescents (Willems et al., Reference Willems, Li, Hendriks, Bartels and Finkenauer2018, Reference Willems, de Zeeuw, van Beijsterveldt, Boomsma, Bartels and Finkenauer2020), which has been linked to increased risk for alcohol misuse (Rømer Thomsen et al., Reference Rømer Thomsen, Buhl Callesen, Hesse, Lehmann Kvamme, Mulbjerg Pedersen, Uffe Pedersen and Voon2018; Stautz & Cooper, Reference Stautz and Cooper2013). These findings suggest that parenting behaviors, such as monitoring and acceptance, and family conflict may influence alcohol use and impulsivity among children and adolescents through multiple direct and indirect pathways.
Parenting and the family environment can also play an important role in moderating genetic influences. Different hypotheses regarding the role of social context in moderating genetic influences have been proposed by researchers (Shanahan & Hofer, Reference Shanahan and Hofer2005). The social context as compensation hypothesis of G×E posits that positive and enriched environments (e.g., parental acceptance) can prevent the expression of a genetic diathesis. Similarly, the social context as social control hypothesis of G×E proposes that environments that offer strong social control (e.g., parental monitoring) can suppress or attenuate genetic risk. Prior research using different genetically informed designs has provided evidence supporting these hypotheses. Twin studies and research using PRS approaches have been used to assess how parenting behaviors may moderate genetic risk for impulsivity and alcohol use. These studies found that high levels of parental monitoring attenuated genetic influences for alcohol-related problems (Cooke et al., Reference Cooke, Meyers, Latvala, Korhonen, Rose, Kaprio, Salvatore and Dick2015; Salvatore et al., Reference Salvatore, Aliev, Bucholz, Agrawal, Hesselbrock, Hesselbrock, Bauer, Kuperman, Schuckit, Kramer, Edenberg, Foroud and Dick2015). The contextual triggering or diathesis-stress hypothesis of G×E posits that social context can act as a stressor that triggers or activates a genetic diathesis (Shanahan & Hofer, Reference Shanahan and Hofer2005). Accordingly, stressors in the family environment, such as family conflict, may exacerbate genetic risk of AUD. We note that research has yet to incorporate PRS to examine the role of family conflict in moderating genetic influences on alcohol use and related impulsive traits. Collectively, these studies demonstrate the potential role of both specific parenting behaviors (e.g., parental monitoring and acceptance) and the family environment (e.g., family conflict) in modifying genetic risk for alcohol use and related outcomes. Notably, prior research suggests that environmental factors, including parenting and family conflict, are in part influenced by genetic factors (i.e., gene-environment correlation or rGE; Elam et al., Reference Elam, Chassin, Lemery-Chalfant, Pandika, Wang, Bountress, Dick and Agrawal2017; Kendler & Baker, Reference Kendler and Baker2007). Thus, it is important to account for rGE when examining G×E effects.
Studying G×E in diverse populations
The majority of genetically-informative research has been conducted with populations of European ancestry (EA) (Dick et al., Reference Dick, Barr, Guy, Nasim and Scott2017; Popejoy & Fullerton, Reference Popejoy and Fullerton2016). The underrepresentation of racial/ethnic minority populations in genetic research is problematic, which may exacerbate existing health disparities among racial/ethnic minorities (Martin et al., Reference Martin, Kanai, Kamatani, Okada, Neale and Daly2019). Discoveries in genetic research are beginning to be used to inform personalized diagnosis and treatment for biomedical conditions (e.g., diabetes); yet precision medicine is primarily benefiting EAs (Grubb et al., Reference Grubb, McDonald, Rutters, Donnelly, Hattersley, Oram, Palmer, Van Der Heijden, Carr, Elders, Weedon, Slieker, t Hart, Pearson, Shields and Jones2019; Patel et al., Reference Patel, Oram, Flanagan, De Franco, Colclough, Shepherd, Ellard, Weedon and Hattersley2016; Udler et al., Reference Udler, McCarthy, Florez and Mahajan2019). Using genetically informed designs to understand pathways of risk for alcohol problems in diverse populations is critical to better understand and reduce racial/ethnic disparities in alcohol related outcomes and to ensure all of us equally benefit from health advances related to genetic discoveries. Racial/ethnic minorities, such as Black/African Americans (AA) and Hispanics/Latino (LA), on average consume less alcohol but experience similar or more negative social and health consequences related to alcohol use compared to EAs (Caetano et al., Reference Caetano, Vaeth, Chartier and Mills2014; Chartier & Caetano, Reference Chartier and Caetano2010; Mulia et al., Reference Mulia, Ye, Greenfield and Zemore2009). In addition, there are differences in the environmental conditions and stressors experienced by racial/ethnic minorities compared to EAs, such as lower SES and experiences of racial discrimination (Wallace & Muroff, Reference Wallace and Muroff2002; Williams et al., Reference Williams, Mohammed, Leavell and Collins2010), which may trigger alcohol use and exacerbate genetic risk. Moreover, cultural factors such as ethnic-racial identity (Walker et al., Reference Walker, Derlan Williams, Cage, DeLaney, Lozada and Dick2020) and cultural values (e.g., familism) also affect alcohol use (Shih et al., Reference Shih, Miles, Tucker, Zhou and D’Amico2012; Zemore, Reference Zemore2007), and may attenuate genetic risk due to stronger social control. Finally, there are important differences in genetic diversity, allele frequencies, and linkage disequilibrium patterns across populations, implying potential differences in the effects of genetic factors on alcohol use and related phenotypes (Campbell & Tishkoff, Reference Campbell and Tishkoff2008; Gelernter et al., Reference Gelernter, Kranzler, Sherva, Almasy, Koesterer, Smith, Anton, Preuss, Ridinger, Rujescu, Wodarz, Zill, Zhao and Farrer2014). Together, these differences in environmental, cultural, and genetic factors suggest that G×E processes related to alcohol use and related outcomes may vary across racial/ethnic groups, highlighting the importance of studying G×E among racially/ethnically diverse populations.
The present study
The goals of this study were two-fold. First, we examined the influence of genetic risk of AUD on childhood impulsivity, a robust early precursor and intermediate phenotype of alcohol use and AUD. Second, we examined the role of parenting behaviors (i.e., parental monitoring and acceptance) and family environment (i.e., family conflict) in moderating genetic risk in racially and ethnically diverse youth. Moving beyond the candidate-gene approach, which does not capture the fact that complex traits and behaviors like impulsivity and alcohol use are polygenic (i.e., influenced by many genes of small effect sizes; Plomin et al., Reference Plomin, Haworth and Davis2009), we characterized individuals’ genetic risk of AUD by using the PRS approach. This approach constructs weighted sums of risk allele counts of SNPs associated with a phenotype (i.e., AUD) based on published results from GWASs and captures the polygenic nature of complex behavioral outcomes (Bogdan et al., Reference Bogdan, Baranger and Agrawal2018). We hypothesized that higher AUD polygenic risk scores (AUD-PRS) would be associated with higher levels of impulsivity. We further hypothesized that parenting behaviors and family environment would moderate genetic influences, such that the association between AUD-PRS and impulsivity would be attenuated by high levels of parental monitoring and acceptance and exacerbated by high levels of family conflict.
Method
Sample
Data for the present study were drawn from the Adolescent Brain Cognitive Development (ABCD) Study (Volkow et al., Reference Volkow, Koob, Croyle, Bianchi, Gordon, Koroshetz, Pérez-Stable, Riley, Bloch, Conway, Deeds, Dowling, Grant, Howlett, Matochik, Morgan, Murray, Noronha, Spong and Weiss2018). The ABCD Study is an ongoing study aimed at understanding brain and behavioral development, which examines youth from ages 9–10 for approximately 10 years into young adulthood. Started in 2016, the ABCD study has completed recruitment for the baseline study sample (N = 11,875; youth = 9–10 years old at baseline; 47.8% female; 52.1% non-Hispanic White, 15.0% non-Hispanic Black, 20.3% Hispanic/Latino, 2.1% Asian, and 10.5% other [e.g., biracial]) that reflects the sociodemographic variation of the U.S. population (Karcher & Barch, Reference Karcher and Barch2021). A national, multi-stage probability sampling strategy was used to recruit eligible youth through schools across 21 sites in the U.S., with some participants (<10%) recruited via other means such as community events, non-targeted schools, and referral systems (Garavan et al., Reference Garavan, Bartsch, Conway, Decastro, Goldstein, Heeringa, Jernigan, Potter, Thompson and Zahs2018). The ABCD study collects rich data on neurocognitive, biospecimen, behavioral, and environmental measures from participants, which is shared with the research community through annual data releases via the NIMH Data Archive. For the purpose of the present study, we used data from the baseline assessment included in the ABCD data release 3.0. We focused on youth who had genomic data available and were identified as non-Hispanic White (n = 5,911, 53% male), non-Hispanic Black/African American (n = 1693, 50% male), or Hispanic/Latino (n = 2,118, 53.4% male) by parent report, the largest three groups within the ABCD sample for which there are sufficient sample sizes for within-group analyses.
Measures
Impulsivity
Participants completed a 20-item youth short-version of the UPPS-P at baseline. This version was developed for the ABCD study and maintained the response format of the original child version (Zapolski et al., Reference Zapolski, Stairs, Settles, Combs and Smith2010) of the UPPS-P, which has been validated across populations (Magid & Colder, Reference Magid and Colder2007; Smith et al., Reference Smith, Fischer, Cyders, Annus, Spillane and McCarthy2007). This measure included five subscales (four items each, responses ranged from 1 = not at all like me to 4 = very much like me): negative urgency (e.g., “when I am upset I often act without thinking”), positive urgency (e.g., “when I am in a great mood, I tend to do things that can cause me problems”), lack of perseverance (e.g., “I almost always finish projects that I start”), lack of premeditation/planning (e.g., “I tend to stop and think before doing things”), and sensation seeking (e.g., “I like new, thrilling things, even if they are a little scary”). Scores were coded and averaged across items within each subscale, such that higher scores indicate higher levels of impulsivity. Confirmatory factor analyses indicated that a one-factor latent factor model of the UPPS-P dimensions of impulsivity did not yield good model fit, with some dimensions having very small factor loadings (Supplemental Figure 1). Thus, the five UPPS-P dimensions of impulsivity were examined separately as outcome variables in subsequent analysis.
Parental monitoring
Participants completed the Parental Monitoring Scale which assessed parents’ monitoring and knowledge of their children’s whereabouts and who their children were spending time with (Gonzalez et al., Reference Gonzalez, Thompson, Sanchez, Morris, Gonzalez, Feldstein Ewing, Mason, Arroyo, Howlett, Tapert and Zucker2021). The scale consists of a total of five items (e.g., “how often do your parents/guardians know where you are?” and “how often do your parents know who you are with when you are not at school and away from home?”). The participants were asked to indicate the extent to which they agreed with each item based on a scale ranging from 1 (not at all) to 5 (very often). Total scores were calculated by averaging the individual’s responses across all five items.
Parental acceptance
Participants were asked to complete a subscale of the Child Report of Behavior Inventory (CRPBI; Schaefer, Reference Schaefer1965) that measured their perceptions of their caregiver’s warmth, acceptance, and responsiveness (e.g., “my caregiver makes me feel better after talking over my worries with him/her” and “my caregiver smiles at me often”). The ABCD study’s acceptance subscale utilizes five of the original scale’s ten items with the highest factor loadings (Gonzalez et al., Reference Gonzalez, Thompson, Sanchez, Morris, Gonzalez, Feldstein Ewing, Mason, Arroyo, Howlett, Tapert and Zucker2021). The participants were asked to respond to items related to the perceived acceptance levels of their two primary caregivers. The participants reported the extent to which they agreed with each item based on a scale ranging from 1 (not at all) to 3 (very much). A total parental acceptance score was calculated by averaging the scores on the five items across the two caregivers.
Family conflict
Participants completed nine items from the Family Conflict subscale of the Moos Family Environment Scale (FES), which assessed the amount of openly expressed conflict among family members (Moos & Moos, Reference Moos and Moos1976). Participants were asked to indicate whether statements about conflict in the family were true or false in their home environment (e.g., “we fight a lot in our family” and “family members sometimes get so angry they throw things”). Items were scored either 1 or 0 (i.e., true or false) with appropriate reverse coding for certain items (e.g., “family members hardly ever lose their temper”). Raw scores were calculated by adding up all the individual items (with appropriate reverse coding). Prorated scores were calculated by multiplying the raw scores by the total number of items and dividing by the number of items completed by the participant. If a participant answered less than five items, their scores were not counted and coded as missing. Higher scores indicate more conflict within the family environment.
Genotyping and AUD genome-wide polygenic scores
Saliva samples were collected at the baseline visit and shipped from the collection site to Rutgers University Cell and DNA Repository (RUCDR) for genotyping. The Smokescreen Genotyping Array (Baurley et al., Reference Baurley, Edlund, Pardamean, Conti and Bergen2016) was used for genotyping. RUCDR performed DNA quality controls based on calling signals and variant call rates, and the quality-controlled (QCed) genotyping data contains 11,099 unique individuals with 516,598 genetic variants in the ABCD study. Imputation was performed via the TOPMed imputation server using mixed ancestry and Engle v2.4 phasing. SNPs with a genotyping rate <0.95 or that violated Hardy–Weinberg equilibrium (p < 10−6) or with minor allele frequency <0.01 were excluded from analysis.
The predictive power and accuracy of PRS depends largely on the sample size and statistical power of the discovery GWAS (Dudbridge, Reference Dudbridge2013) and the genetic ancestral similarities between the discovery and target samples (Duncan et al., Reference Duncan, Shen, Gelaye, Meijsen, Ressler, Feldman, Peterson and Domingue2019; Martin et al., Reference Martin, Kanai, Kamatani, Okada, Neale and Daly2019). Thus, we used results from GWAS of AUD with the Million Veteran Program (MVP) sample (Kranzler et al., Reference Kranzler, Zhou, Kember, Vickers Smith, Justice, Damrauer, Tsao, Klarin, Baras, Reid, Overton, Rader, Cheng, Tate, Becker, Concato, Xu, Polimanti, Zhao and Gelernter2019), the largest published GWAS of alcohol phenotypes with a multi-ancestry sample, to calculate AUD-PRS in the ABCD sample. The MVP sample includes 209,020 individuals of European Ancestry (EA), 57,340 of African Ancestry (AA), 14,425 of Latinos/Latin Ancestry (LA), 1410 of East Asian Ancestry, and 196 of South Asian Ancestry. GWAS was conducted separately in each group and then meta-analyzed using a sample-size-weighted scheme; PRS derived from this GWAS study were associated with alcohol-related disorders in two independent samples of European and African ancestry (Kranzler et al., Reference Kranzler, Zhou, Kember, Vickers Smith, Justice, Damrauer, Tsao, Klarin, Baras, Reid, Overton, Rader, Cheng, Tate, Becker, Concato, Xu, Polimanti, Zhao and Gelernter2019). We used the EA GWAS results to calculate AUD-PRS for non-Hispanic Whites in the ABCD sample, using the PRS-CS method, a Bayesian regression and continuous shrinkage prior method shown to improve predictive power above traditional methods of PRS construction (Ge et al., Reference Ge, Chen, Ni, Feng and Smoller2019). An extension of this method (PRS-CSx) has recently been developed to improve polygenic prediction in non-EA populations by integrating GWAS summary statistics from multiple populations and leveraging linkage disequilibrium diversity across discovery samples (Ruan et al., Reference Ruan, Feng, Chen, Lam, Global, Initiatives, Sawa, Martin, Qin, Huang and Ge2021). We used PRS-CSx to calculate AUD-PRS for the non-Hispanic Black/African American and Hispanic/Latino subsamples in our study. Specifically, summary statistics from the MVP EA and AA GWAS were used to calculate AUD-PRS for Black/African Americans, and summary statistics from the MVP EA and LA GWAS were used to calculate AUD-PRS for Hispanic/Latinos. AUD-PRS were standardized to aid in interpretation of results.
Covariates
We included participants’ age and sex as control variables given prior evidence that impulsivity, parenting, and family factors may differ between males and females and across age (Cross et al., Reference Cross, Copping and Campbell2011; Webb et al., Reference Webb, Bray, Getz and Adams2002). Because socioeconomic status is associated with impulsivity, parenting, and family environment (Assari et al., Reference Assari, Caldwell and Mincy2018; Farley & Kim-Spoon, Reference Farley and Kim-Spoon2017), we also included parental education and family income as covariates. Parents answered the question “What is the highest grade or level of school you have completed or the highest degree you have received?”. Response options ranged from 1 (never attended school or Kindergarten only) to 21 (doctoral degree). For those who indicated that they had a partner, they also answered the same question about their partner’s education. Scores across the two questions were averaged, and higher scores indicate higher levels of parental education. Parents also reported their total combined family income for the past 12 months, with responses ranging from 1 = less than $5,000 to 10 = $200,000 or greater. Finally, we also included the first ten genetic ancestry principal components (PC1-PC10) as covariates to account for potential population stratification in genetic analyses (Hellwege et al., Reference Hellwege, Keaton, Giri, Gao, Velez Edwards and Edwards2018).
Analytic strategy
We first conducted preliminary analyses to examine descriptive statistics and correlations between study variables using SPSS 25.0. All analyses were conducted separately for White, Black/African American, and Hispanic/Latino youth. To test our hypotheses, we conducted a series of hierarchical linear regression analyses using Mplus version 8.3. We included participants’ age, sex, parental education, family income, and PC1-PC3 as covariates in all analyses. We first examined the main effects of AUD-PRS on impulsivity (Step 1). UPPS-P dimensions of impulsivity (i.e., negative urgency, sensation seeking, lack of premeditation, lack of perseverance, and positive urgency) were examined as separate outcome variables in parallel analyses. Next, we added parental monitoring, parental acceptance, and family conflict as additional predictors to the regression model to examine main effects of parenting and family conflict (Step 2). To examine interaction effects between AUD-PRS and family environmental factors, we created product terms of AUD-PRS and mean-centered parental monitoring, parental acceptance, and family conflict and added them as additional predictors to the regression model (Step 3). We also examined potential rGE by testing correlations between AUD-PRS and parenting and family conflict. Significant rGE were accounted for in our models testing G×E effects, by specifying AUD-PRS and parenting/family conflict to be correlated using the “WITH” command in Mplus. Missing data were accounted for using the full information maximum likelihood estimation method. Complex sampling (e.g., sibling and twin pairs) and recruitment procedures (e.g., across different study sites) for the ABCD Study were accounted for using cluster correction (Cluster = family ID) and stratification sampling (Stratification = study site) procedures in Mplus. In order to account for multiple testing (five impulsivity outcomes), we used a Bonferroni-corrected p value (p < .01) to evaluate statistical significance of coefficients in each of our analytic subsamples.
Results
Preliminary analysis
Descriptive statistics and correlations between variables are presented in Table 1. AUD-PRS was not significantly correlated with impulsivity, parenting, and family conflict among White, Black/African American, and Hispanic/Latino youth. Across racial/ethnic groups, there were significant negative correlations between parental monitoring/acceptance and dimensions of impulsivity, except that parental acceptance was positively correlated with sensation seeking for White and Hispanic/Latino youth; family conflict was positively correlated with dimensions of impulsivity, with the correlation coefficients varying to some extent across different dimensions of impulsivity.
Table 1. Descriptive statistics and bivariate correlations among key study variables
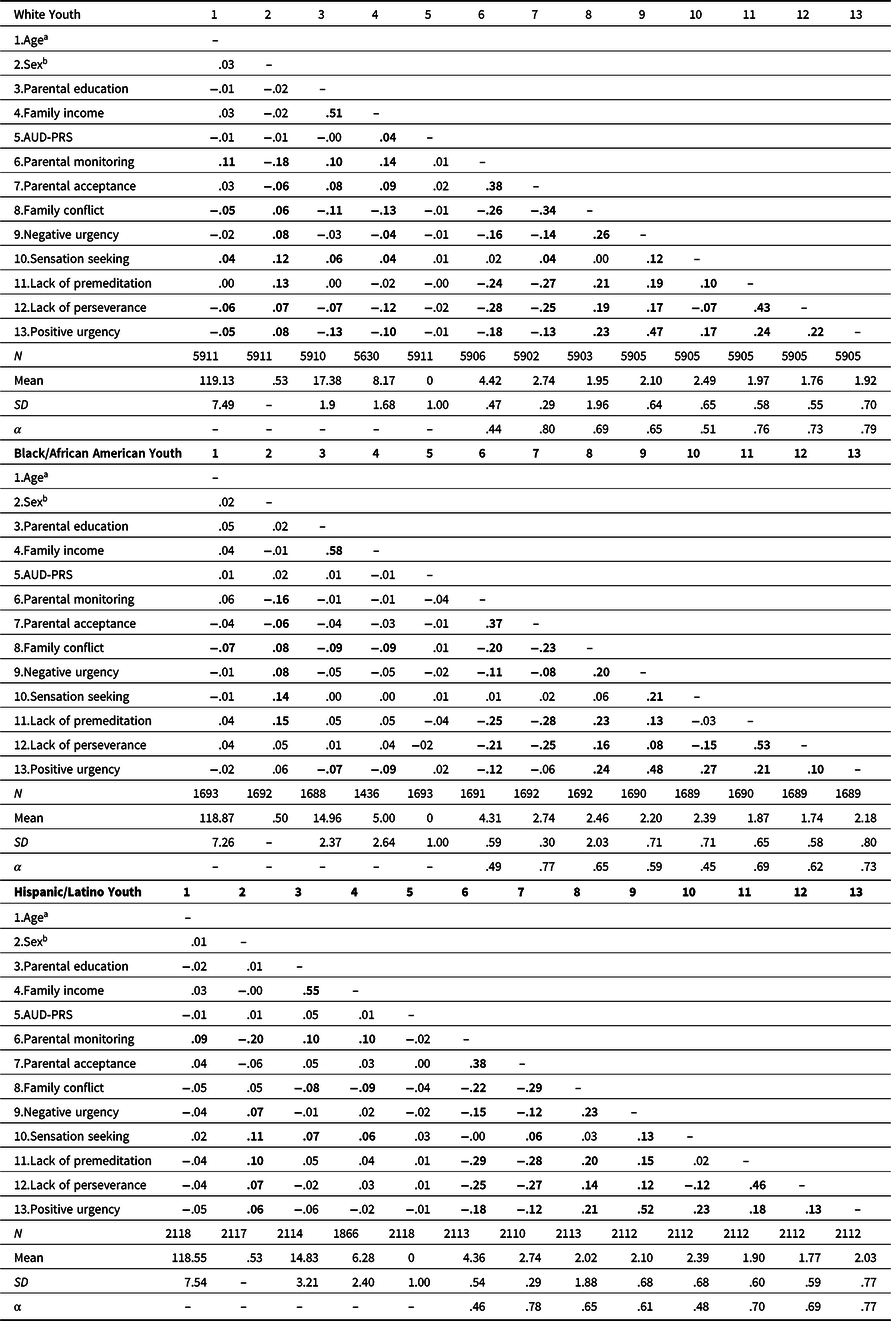
Note. AUD-PRS = alcohol use disorder genome-wide polygenic score. Coefficients with p < .01 were bolded. α = Cronbach’s alpha.
a age was coded in months.
b sex was coded 1 = male, 0 = female.
Predicting childhood impulsivity from AUD-PRS, parenting, and family conflict
White youth
Results from hierarchical multiple regression models predicting impulsivity among White youth are presented in Table 2. Contrary to our hypothesis, there was no significant main effect of AUD-PRS on any of the UPPS-P impulsivity dimensions (Step 1). Consistent with expectation, higher parental monitoring was significantly associated with lower levels of impulsivity across all UPPS-P dimensions above and beyond the effects of age, sex, parental education, and family income, except that it was not associated with sensation seeking. Higher parental acceptance was associated higher sensation seeking, lower lack of premeditation, and lower lack of perseverance, but was not significantly associated with positive and negative urgency. Higher family conflict was associated with higher levels of impulsivity across all UPPS-P dimensions, except for sensation seeking (Step 2). There were two nominally significant interaction effects: the interaction between AUD-PRS and parental acceptance in relation to negative urgency (β = .04, p = .02), and the interaction between AUD-PRS and family conflict in relation to positive urgency (β = .03, p = .04) (Step 3). We conducted post hoc follow-up analysis to further evaluate these two interaction effects, by including AUD-PRS by covariate (age, sex, parental education, family income, PC1-PC10) and family factor (parental acceptance or family conflict) by covariate interaction terms in the regression model to further account for potential confounding effects (Keller, Reference Keller2014; see Supplemental Tables 1 and 2). Neither of these interaction effects were statistically significant at p < .01 in the robustness analysis. Thus, we did not further probe or discuss these interaction effects.
Table 2. Predicting childhood impulsivity from alcohol use disorder polygenic scores, parenting, and family conflict among White/European American youth
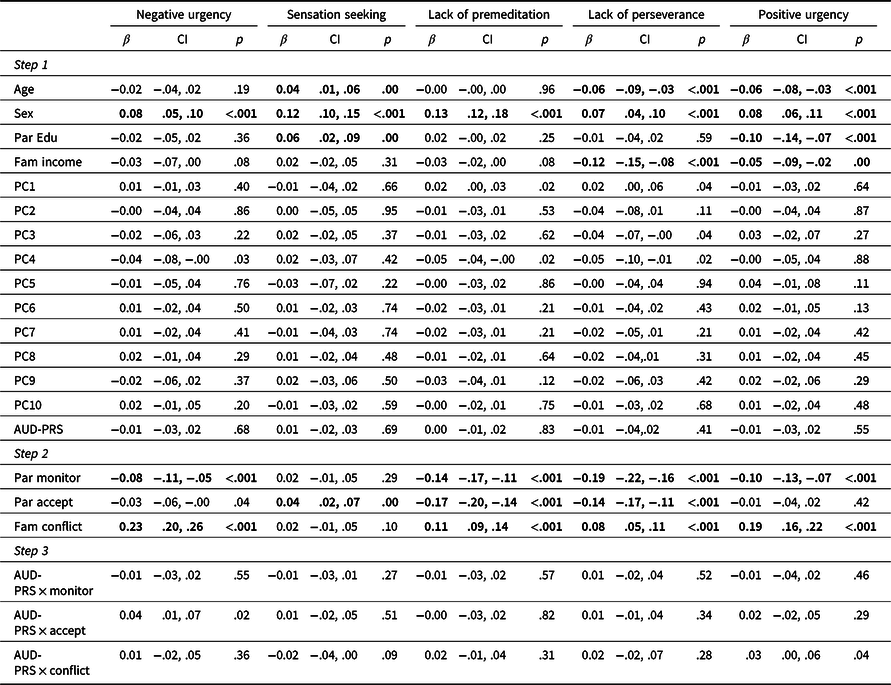
Note. AUD-PRS = alcohol use disorder genome-wide polygenic score; Par Edu = parental education; Fam income = family income; PC = genetic ancestry principal components; Par monitor = parental monitoring; Par accept = parental acceptance; Fam conflict = family conflict. Sex was coded 1 = male, 0 = female. CI = 95% confidence intervals. Bolded coefficients p < .01.
Black/African American youth
Results from hierarchical multiple regression models predicting impulsivity among Black/African American youth are presented in Table 3. Consistent with findings for White youth, there was no significant main effect of AUD-PRS on impulsivity (Step 1). The patterns of associations between parental monitoring, parental acceptance, family conflict, and impulsivity dimensions were largely the same as those observed for White youth, except for the associations with sensation seeking. Specifically, higher parental monitoring was associated with lower levels of impulsivity across all UPPS-P dimensions above and beyond the effects of covariates, except for sensation seeking. Higher parental acceptance was associated with lower lack of premeditation and lower lack of perseverance, but was not significantly associated with negative urgency, sensation seeking, and positive urgency. Family conflict was associated with higher levels of impulsivity across all UPPS-P dimensions (Step 2). Finally, there was suggestive evidence of interaction between AUD-PRS and family conflict in relation to positive urgency (B = .024, SE = .011, 95% CI = [.006, .042], β = .059, p = .032) (Step 3). Follow-up analysis indicated that this interaction effect became statistically significant in follow up analysis where AUD-PRS by covariate (age, sex, parental education, family income, PC1-PC10) and family conflict by covariate interaction terms were included in the regression model (B = .026, SE = .010, 95% CI = [.010, .042], β = .065, p = .007, see Supplemental Table 1), suggesting robustness of the interaction effect. As illustrated in Figure 1, simple slope analysis indicated that AUD-PRS was significantly associated with higher positive urgency when family conflict was high (+1 SD; B = .07, 95% CI = [.03, .11], β = .08, p = .005) but not when family conflict was low (−1 SD; B = −.03, 95% CI = [−.08, .01], β = −.04, p = .283). We note that the follow-up analysis was post hoc and should be considered preliminary and interpreted with caution.
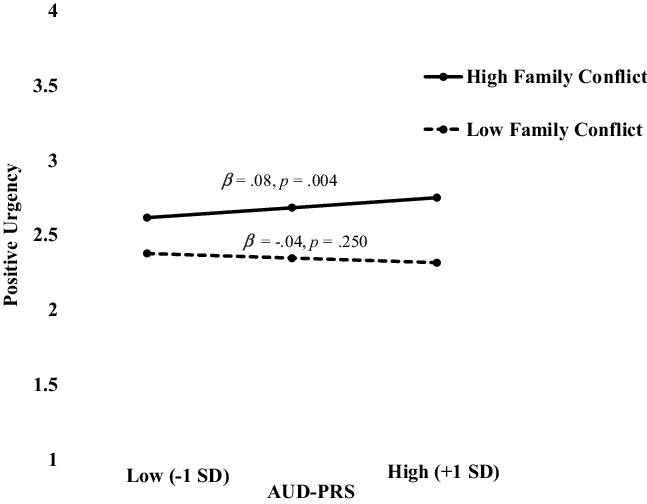
Figure 1. AUD-PRS by family conflict in relation positive urgency among Black/African American youth. Predicted values of positive urgency are plotted at prototypical values (+1/−1 SD) of AUD-PRS and family conflict.
Table 3. Predicting childhood impulsivity from alcohol use disorder polygenic scores, parenting, and family conflict among Black/African American youth
Note. AUD-PRS = alcohol use disorder genome-wide polygenic score; Par Edu = parental education; Fam income = family income; PC = genetic ancestry principal components; Par monitor = parental monitoring; Par accept = parental acceptance; Fam conflict = family conflict. Sex was coded 1 = male, 0 = female. CI = 95% confidence intervals. Bolded coefficients p < .01.
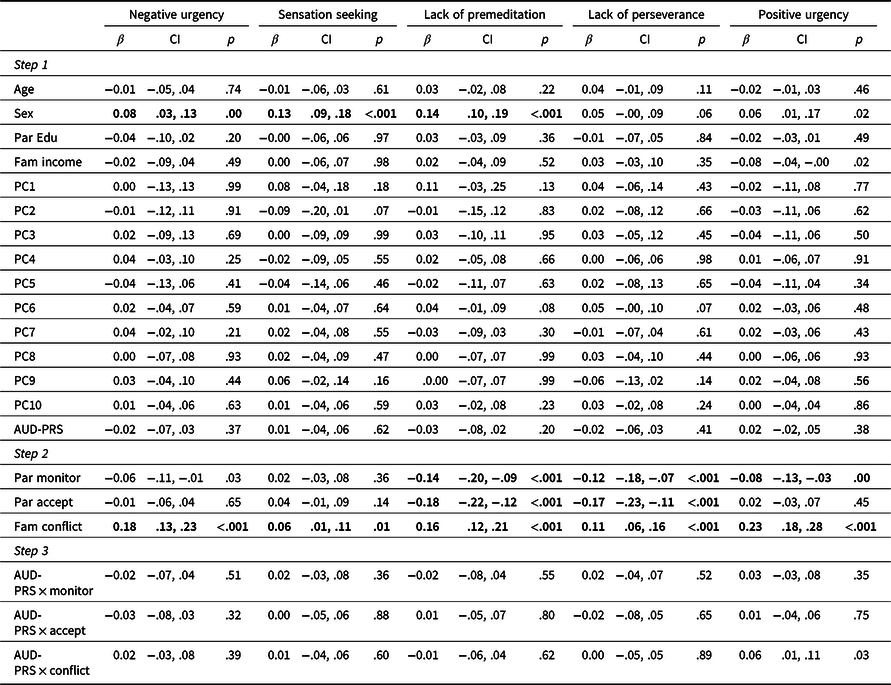
Hispanic/Latino youth
Results from hierarchical multiple regression models predicting impulsivity among Hispanic/Latino youth are presented in Table 4. Consistent with findings for White and Black/African American youth, there were no significant main effects of AUD-PRS on dimensions of impulsivity (Step 1). The patterns of associations between parental monitoring, parental acceptance, family conflict, and impulsivity dimensions were largely the same as those observed for White youth (see above), except that the association between family conflict and lack of perseverance was not statistically significant after adjusting for multiple testing (p = .04) for Hispanic/Latino youth. There were no significant interactions between AUD-PRS and parental monitoring, parental acceptance, and family conflict in relation to dimensions of impulsivity (Step 3).
Table 4. Predicting childhood impulsivity from alcohol use disorder polygenic scores, parenting, and family conflict among Hispanic/Latino youth
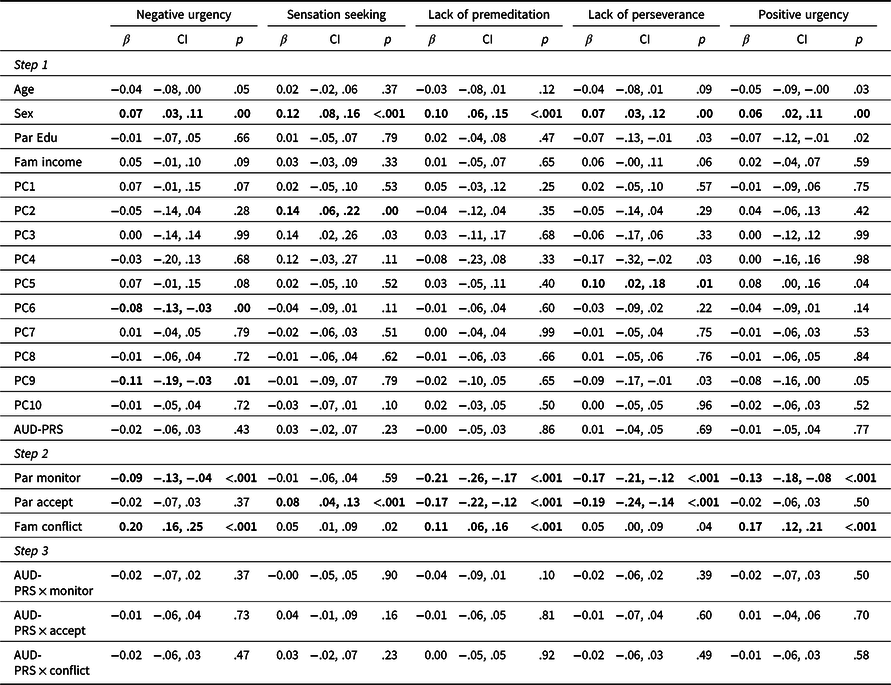
Note. AUD-PRS = alcohol use disorder genome-wide polygenic score; Par Edu = parental education; Fam income = family income; PC = genetic ancestry principal components; Par monitor = parental monitoring; Par accept = parental acceptance; Fam conflict = family conflict. Sex was coded 1 = male, 0 = female. CI = 95% confidence intervals. Bolded coefficients p < .01.
Discussion
In this study, we examined the independent and interactive effects of genetic risk for AUD, indexed by AUD-PRS, parenting behaviors (i.e., parental monitoring and acceptance), and family environment (i.e., family conflict) on childhood impulsivity among White, Black/African American, and Hispanic/Latino youth in the ABCD study. We found that AUD-PRS was not significantly associated with childhood impulsivity as measured by the UPPS-P scale across racial/ethnic groups. In general, parental monitoring and acceptance were associated with lower levels of impulsivity, whereas family conflict was associated with higher levels of impulsivity, with associations varied to some extent across dimensions of impulsivity. In addition, findings suggest that family conflict may exacerbate the effect of genetic risk for AUD on childhood impulsivity (i.e., positive urgency), particularly among Black/African American youth.
It is well-known that genetics play an important role in AUD (Verhulst et al., Reference Verhulst, Neale and Kendler2015). Little is known about how genetic risk of AUD manifests early in development (e.g., childhood), because genetic studies of AUD have primarily focused on adolescents and adults (Dick et al., Reference Dick, Barr, Cho, Cooke, Kuo, Lewis, Neale, Salvatore, Savage and Su2018). GWAS studies indicated that alcohol phenotypes have a polygenic architecture that overlaps with substance use and other psychiatric traits (Kranzler et al., Reference Kranzler, Zhou, Kember, Vickers Smith, Justice, Damrauer, Tsao, Klarin, Baras, Reid, Overton, Rader, Cheng, Tate, Becker, Concato, Xu, Polimanti, Zhao and Gelernter2019; Liu et al., Reference Liu, Jiang, Wedow, Li, Brazel, Chen, Datta, Davila-Velderrain, McGuire, Tian, Zhan, Agee, Alipanahi, Auton, Bell, Bryc, Elson, Fontanillas, Furlotte and Vrieze2019; Walters et al., Reference Walters, Polimanti, Johnson, McClintick, Adams, Adkins, Aliev, Bacanu, Batzler, Bertelsen, Biernacka, Bigdeli, Chen, Clarke, Chou, Degenhardt, Docherty, Edwards, Fontanillas and Agrawal2018). Research using PRS to characterize genetic risk for alcohol and related phenotypes has shown that alcohol PRS predicts alcohol outcomes, impulsivity, externalizing behaviors, and related traits (Barr et al., Reference Barr, Ksinan, Su, Johnson, Meyers, Wetherill, Latvala, Aliev, Chan, Kuperman, Nurnberger, Kamarajan, Anokhin, Agrawal, Rose, Edenberg, Schuckit, Kaprio and Dick2020; Ksinan et al., Reference Ksinan, Su, Aliev and Dick2019). However, most GWAS and PRS studies focused on adult samples, and limited research has examined whether and how PRS derived from adult-based GWAS predicts childhood traits. The present study filled this gap in the literature by examining the role of AUD-PRS in predicting childhood impulsivity. Contrary to our hypotheses, there was no significant main effect of AUD-PRS on various aspects of childhood impulsivity. This non-significant finding may suggest developmental changes in genetic influences. That is, genetic factors that influence behaviors and traits (e.g., AUD) in adulthood may be distinct from genetic factors that contribute to behaviors and traits earlier in development (Dick, Reference Dick2011; Elam et al., Reference Elam, Ha, Neale, Aliev, Dick and Lemery-Chalfant2021). However, there is some evidence suggesting that PRS for adult alcohol dependence and related traits are associated with childhood psychopathology (Akingbuwa et al., Reference Akingbuwa, Hammerschlag, Jami, Allegrini, Karhunen, Sallis, Ask, Askeland, Baselmans, Diemer, Hagenbeek, Havdahl, Hottenga, Mbarek, Rivadeneira, Tesli, van Beijsterveldt, Breen and Lewis2020; Jansen et al., Reference Jansen, Jansen, Savage, Kraft, Skarabis, Polderman and Dieleman2021). For example, higher PRS for adult alcohol dependence predicted higher risk of case (versus control) status in a child and adolescent psychiatric sample with a variety of psychiatric disorders (Jansen et al., Reference Jansen, Jansen, Savage, Kraft, Skarabis, Polderman and Dieleman2021). Thus, while AUD-PRS did not predict childhood impulsivity as measured in the present study, it is possible that it predicts other childhood traits. Future studies need to expand the present study to examine other childhood precursors of AUD, such as externalizing behaviors and other aspects of temperament (e.g., negative emotionality). Alternatively, the null finding could be due to low predictive power of the AUD-PRS. We attempted to maximize the predictive power of AUD-PRS in the present study by using estimates from the largest multi-ancestry GWAS and applying state of the science approaches (PRS-CS and PRS-CSx). However, we note that the MVP sample was of smaller sample size compared to other large GWAS of alcohol phenotypes (Liu et al., Reference Liu, Jiang, Wedow, Li, Brazel, Chen, Datta, Davila-Velderrain, McGuire, Tian, Zhan, Agee, Alipanahi, Auton, Bell, Bryc, Elson, Fontanillas, Furlotte and Vrieze2019), and thus may be underpowered. In addition, it is also possible that AUD-PRS derived from GWAS with veterans may not generalize to the broader population and to early adolescence.
Numerous studies have documented the role of parenting behaviors, such as parental monitoring and acceptance in influencing adolescent alcohol use outcomes (Ryan et al., Reference Ryan, Jorm and Lubman2010; Yap et al., Reference Yap, Cheong, Zaravinos-Tsakos, Lubman and Jorm2017). We built on the literature to examine associations between these parenting behaviors and childhood impulsivity. Consistent with our hypotheses, higher parental monitoring and acceptance were associated with lower levels of impulsivity across various UPPS-P dimensions, with similar patterns of associations observed across racial/ethnic groups. These findings demonstrate that parental knowledge of adolescent’s activities and supportive behaviors may be important pathways through which caregivers can improve the cognitive and socioemotional regulatory skills of their children. Somewhat unexpectedly, we found that higher parental acceptance was associated with higher sensation seeking among White and Hispanic/Latino youth. Sensation seeking in childhood may primarily involve seeking fun and new experiences that are not necessarily risky. It is possible that high parental acceptance offers a strong secure base for children to explore and seek out new experiences. Nevertheless, we consider this finding preliminary and future efforts to replicate this finding are warranted. Despite these main effects of parenting behaviors on impulsivity, we did not find any significant interaction effects between AUD-PRS and parenting behaviors in relation to dimensions of impulsivity. This is contradictory to our hypotheses, as well as prior evidence that parenting behaviors moderate genetic influence on alcohol use and related behaviors in adolescence and adulthood (Cooke et al., Reference Cooke, Meyers, Latvala, Korhonen, Rose, Kaprio, Salvatore and Dick2015; Salvatore et al., Reference Salvatore, Aliev, Bucholz, Agrawal, Hesselbrock, Hesselbrock, Bauer, Kuperman, Schuckit, Kramer, Edenberg, Foroud and Dick2015; Su et al., Reference Su, Supple, Leerkes and Kuo2019). It is possible that parenting behaviors play a stronger role in modifying genetic influences on behavioral outcomes later in development compared to temperamental traits in childhood. Alternatively, these findings could suggest that parenting behaviors are important influences on childhood impulsivity regardless of genetic predispositions. It is also possible that the present study was not well-powered to detect significant interactions between AUD-PRS and parenting behaviors, in part due to the limited predictability of AUD-PRS.
In addition to specific parenting behaviors, our findings indicated that the emotional climate in the family environment (i.e., family conflict) also plays an important role in relation to childhood impulsivity. Higher levels of family conflict were associated with higher levels of impulsivity across various UPPS-P dimensions and across racial/ethnic groups. These findings are consistent with prior research showing that family conflict was associated with lower self-control and higher impulsivity in children and adolescents (Wang et al., Reference Wang, Buu, Lohrmann, Shih and Lin2020; Willems et al., Reference Willems, Li, Hendriks, Bartels and Finkenauer2018, Reference Willems, de Zeeuw, van Beijsterveldt, Boomsma, Bartels and Finkenauer2020). Furthermore, consistent with our hypothesis, we found suggestive evidence of interaction effect between AUD-PRS and family conflict in relation to one dimension of childhood impulsivity. Specifically, AUD-PRS was associated with higher positive urgency when family conflict was high but not when family conflict was low among Black/African American youth. This finding is consistent with the contextual triggering or diathesis-stress hypothesis of G×E (Shanahan & Hofer, Reference Shanahan and Hofer2005), which posits that contextual stressors can exacerbate genetic influences by triggering or activating a genetic diathesis. Our findings extend the literature by showing the role of family conflict in exacerbating polygenic risk of AUD in relation to a childhood precursor of alcohol use. Collectively, these findings highlight the importance of reducing and managing conflict in the family environment in order to lower impulsivity and promote well-being among children. Although AUD-PRS was not correlated with parenting and family conflict in the present study, prior research suggests that there are significant genetic influences on environmental factors, including parenting and family conflict (Kendler & Baker, Reference Kendler and Baker2007). Thus, efforts aimed at reducing family conflict and promoting positive family environment may be more effective by also considering child and parent genetic factors.
It is interesting that we only found suggestive evidence of G×E effects for positive urgency, but not other dimensions of impulsivity. This may suggest that positive urgency is a salient aspect of impulsivity in childhood where genetic risk of AUD manifests. Indeed, prior research suggests that positive urgency had the greatest representativeness of children’s impulsivity compared to other UPPS-P dimensions (Wang et al., Reference Wang, Buu, Lohrmann, Shih and Lin2020). In our sample, positive urgency also had the highest factor loading among all UPPS-P dimensions on a latent factor of impulsivity (see Supplemental Figure 1). These findings further highlight the importance of examining impulsivity as a multidimensional construct related to alcohol use and AUD (Dick et al., Reference Dick, Smith, Olausson, Mitchell, Leeman, O’Malley and Sher2010). We note that the interaction effect between AUD-PRS and family conflict in relation to positive urgency among Black/African American youth was the only significant interaction effect found among a total of 45 tests (five impulsivity dimensions, three parenting/family factors, and three subsamples). Thus, it is possible that this was a false positive, and we consider this finding preliminary. Future research is needed to replicate our findings of G×E effects.
There are several notable strengths of this study, including the use of a PRS approach to examine G×E, examination of multiple familial contextual factors (i.e., both specific parenting behaviors and family conflict), and the focus on racially and ethnically diverse youth. By studying G×E in a sample of White, Black/African American, and Hispanic/Latino youth, our findings contribute to the limited literature on genetically-informed research among racial/ethnic minority populations. In addition, unlike the focus of prior genetically-informed research on adult and adolescent alcohol use outcomes, the current study took a developmental approach by examining how genetic influences for adult AUD manifest in childhood. A developmental approach can allow us to better understand if the genetic influences for adolescent and adult AUD are associated with precursor traits in childhood, which may help identify at-risk children for intervention and prevention efforts. Despite these strengths, our findings need to be interpreted in light of several limitations. First, we used data from the baseline assessment in order to assess impulsivity in childhood (age 9–10) and maximize the sample size for analysis. This means that parenting and family conflict were measured at the same time as impulsivity. Although we conceptualized parenting and family conflict as predictors of impulsivity in the present study, we acknowledge the possibility of bidirectional associations between them (Wang et al., Reference Wang, Buu, Lohrmann, Shih and Lin2020). Second, we only used UPPS-P to measure dimensions of impulsivity. Despite that UPPS-P is a commonly used measure, we recognize that there are alternative approaches to conceptualize and measure impulsivity, such as using laboratory tasks (Dick et al., Reference Dick, Smith, Olausson, Mitchell, Leeman, O’Malley and Sher2010). Third, some of the scales used in the study (e.g., parental monitoring [α < .50], sensation seeking [α < .52]) had low reliability. Measurement errors for these variables may result in bias in analysis and results. In addition, despite using the state-of-the-science polygenic scoring approach, the AUD-PRS in the present study still had limited predictability and we were underpower to detect G×E effects. Furthermore, we conducted a total of 45 tests of G×E effects, raising concerns about Type-I errors in our finding due to multiple testing. Finally, all of the measures were self-report and may subject to reporting bias.
In conclusion, our study extended the literature by taking a developmental approach to examine the role of genetic risk for AUD, in conjunction with parenting behaviors and family conflict, in relation to childhood impulsivity in racially and ethnically diverse youth. Our findings indicated that positive parenting behaviors such as monitoring and acceptance can play important role in reducing childhood impulsivity, whereas family conflict can be a risk factor associated with higher levels of childhood impulsivity among White, Black/African American, and Hispanic/Latino youth. In addition, we found suggestive evidence that family conflict may exacerbate genetic risk of AUD in relation to childhood positive urgency, although this was only found in the Black/African American subsample. These findings highlight the importance of efforts aimed at promoting positive parenting behaviors and managing family conflict as ways to reduce impulsivity among children.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S095457942200092X
Acknowledgements
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from NIMH Data Archive Release 3.0 (DOI 10.15154/1520591). DOIs can be found at https://nda.nih.gov/abcd.
Funding statement
This research was supported by funding from the National Institute of Health/National Institute on Minority Health and Health Disparities (NIMHD/NIH), award 2U54 MD002316 (F. Marsiglia, P.I.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMHD or the NIH.
Conflicts of interest
None.










