Introduction
Borderline personality disorder was long regarded as a static and untreatable condition, but the perspective has shifted toward recognition of its changeable nature. Similar to healthy personality characteristics, their pathological counterparts turned out to be subject to development across the life span [Reference Newton-Howes, Clark and Chanen1]. Despite apparent changes in prevalence and symptomology over time, disease burden of borderline personality disorder is tremendous and remains impactful throughout the life course. For instance, functional impairments and comorbid somatic and mental disorders are commonly found in borderline personality disorder [Reference Lenzenweger, Lane, Loranger and Kessler2, Reference Zanarini, Frankenburg, Hennen and Silk3] and are pervasive in both younger and older patients [Reference Zanarini4–Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman7]. Even subthreshold personality disorders, such as borderline personality traits, are associated with these negative consequences [Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof and Kleinjan8]. Quality of life (QoL) is increasingly viewed as a main indicator of disease burden and an important aspect of treatment outcome [Reference IsHak, Elbau, Ismail, Delaloye, Ha and Bolotaulo9,Reference Spitzer, Kroenke and Linzer10]. In order to further understand the variform impact of borderline personality traits across the life span, we focus our study on the relation between borderline personality traits, age, and QoL.
Healthy personality traits may explain up to 45% variance in mental and up to 39% of variance in physical health-related (HR)-QoL [Reference Huang, Lee, Ketheeswaran, Jones, Revicki and Wu11]. However, studies on the relationship between pathological personality traits and QoL in the general population are quite scarce. Typically, samples consist of psychiatric patients and moreover lack inclusion of adults older than 65 years [Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman7]. A systematic review containing predominantly studies on patient populations suggests that borderline personality disorder is associated with a lower QoL in young and middle-aged adults [Reference IsHak, Elbau, Ismail, Delaloye, Ha and Bolotaulo9]. In later life, borderline personality disorder is associated with several age-related conditions like somatic comorbidity [Reference Oltmanns and Balsis12], higher risk for serious life events [Reference Powers, Gleason and Oltmanns13] and more functional impairment than younger adults with borderline personality disorder [Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman7]. This underscores that when studying the impact of borderline personality disorder across the life span, it is vital to include older persons in the sample, as well as persons with subthreshold levels of borderline personality disorders (i.e., borderline personality traits).
Borderline personality traits appear to amplify the overall impact of an increasing age on QoL. Nonetheless, empirical data on the bivariate association between borderline personality traits and QoL in older adults are particularly scarce [Reference Oltmanns and Balsis12,Reference Powers, Gleason and Oltmanns13]. For instance, among outpatients with borderline personality disorders, QoL was significantly lower among patients aged 46 years and older compared to younger patients [Reference Frías, Palma, Solves, Martínez and Salvador14]. Among older patients with depression, cluster B personality traits (including borderline traits) were found to be negatively associated with QoL [Reference Abrams, Alexopoulos, Spielman, Klausner and Kakuma15]. This effect remained when the depression was remitted at 1-year follow-up, albeit the effect size was small and not adjusted for potential confounders such as physical and mental health indices. Other studies in older adults demonstrate direct associations between personality disorders and QoL, but these studies did not intentionally include patients with borderline personality disorder [Reference Condello, Padoani, Uguzzoni, Caon and De Leo16,Reference Holzer and Huang17]. It can be concluded that empirical findings are thus far insufficient to make distinct inferences about the impact of borderline personality traits on the association between age and HR-QoL in the general population.
The prevalence of a personality disorder according to psychiatric diagnostic criteria is thought to become lower with increasing age [Reference Beatson, Broadbear, Sivakumaran, George, Kotler and Moss18]. Nonetheless, the prevalence of any personality disorder is still estimated at 8.1–11.4% among persons aged 65 years and over [Reference Schuster, Hoertel, Le Strat, Manetti and Limosin19,Reference Reynolds, Pietrzak, El-Gabalawy, Mackenzie and Sareen20]. Well-substantiated prevalence rates for borderline personality disorder in older adults are scarce. Similar to young adults, cluster B personality disorders (including borderline personality disorder) are less common among older people than personality disorders in cluster A and C [Reference Abrams and Bromberg21,Reference Balsis, Woods, Gleason and Oltmanns22]. Data from the second wave of the comprehensive NESARC study also demonstrate a decline in all personality disorders in older adults, including borderline personality disorder [Reference Reynolds, Pietrzak, El-Gabalawy, Mackenzie and Sareen20]. The AUDADIS-IV was used as the assessment tool to examine all psychiatric disorders whereas in the first NESARC wave the International Personality Disorder Examination (IPDE) was used. Despite the overall decline across age groups, the found prevalence rate of borderline personality disorder for adults older than 55 (3.2%) is remarkably higher than that of adults in general (commonly estimated around 1% [Reference Lenzenweger, Lane, Loranger and Kessler2,Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof and Kleinjan8]). However, despite the impressive sample, this remains the finding of a single study. Multiple explanations have been put forward for the decline in borderline personality disorders in older adults, such as high morbidity and mortality due to risk behavior, suicide and somatic comorbidity [Reference Fok, Stewart, Hayes and Moran23,Reference Fok, Chang, Broadbent, Stewart and Moran24], and a decrease in impulsive and aggressive behavior when comes to age. For personality disorders in general, it has been demonstrated that 29% of the diagnostic criteria are not age neutral, which could lead to under detection of personality disorders in later life [Reference Balsis, Gleason, Woods and Oltmanns25]. If indeed borderline personality disorder in later life is harder to detect but still impactful [Reference Beatson, Broadbear, Sivakumaran, George, Kotler and Moss18], it would be valuable to further comprehend the consequences of possessing borderline personality traits throughout a person’s life. This is especially relevant considering a meta-analysis showing that in depressed patients, a comorbid personality disorder doubles the odds of a poor outcome for depression compared to those with no personality disorder [Reference Newton-Howes, Tyrer, Johnson, Mulder, Kool and Dekker26], while psychotherapy for personality disorders in later life appears promising [Reference Videler, van Alphen, van Royen, van der Feltz-Cornelis, Rossi and Arntz27].
Aims of the study
The aim of this study is to investigate whether the presence of borderline personality traits affect the association between age and HR-QoL in the general population. We will specifically distinguish between physical and mental HR-QoL [Reference Walters, Munro and Brazier28]. We hypothesize that physical HR-QoL may be more affected by an increasing age (due to the inevitable increase of the somatic disease burden) than mental HR-QoL (as mental resilience and coping may increase with age [Reference Terrill, Molton, Ehde, Amtmann, Bombardier and Smith29] and prevalence rates of affective disorders decrease with age [Reference Walters, Munro and Brazier28,Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha and Bryson30]). Since borderline personality traits interfere with coping abilities and mental health, we hypothesize that negative effects of increasing age on QoL will become stronger in the presence of borderline personality traits.
Methods
Sample
The Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2) is a representative epidemiological cohort study of the general Dutch population aged 18–65 at the first wave (N = 6,646, response rate 65.1%). One participant per household was randomly selected and interviewed at home. The first wave (T0) was completed during the period of November 2007 to July 2009. The entire T0 group was contacted for follow-up 3 years later and 5,303 respondents (response rate 80.4%, excluding deceased persons) were interviewed again from November 2010 to June 2012 [Reference De Graaf, Van Dorsselaer, Tuithof and Ten Have31]. Data on borderline personality traits were collected at this second wave (T1). Attrition at T1 was not meaningfully associated with all main categories and individual 12-month mental disorders at T0 after controlling for sociodemographic characteristics [Reference De Graaf, Van Dorsselaer, Tuithof and Ten Have31].
The NEMESIS-2 study protocol was approved by a medical ethics committee and all participants provided written informed consent at all waves. For a comprehensive description of the NEMESIS-2 study design, we refer to De Graaf et al. [Reference De Graaf, Ten Have and Van Dorsselaer32].
Measures
Borderline personality traits
The eight questions of the IPDE corresponding with DSM-IV criteria for a borderline personality disorder were used to measure borderline traits [Reference Loranger33,Reference Loranger, Sartorius, Andreoli, Berger, Buchheim and Jacobsberg34]. The IPDE does not measure one BPD-criterion, namely recurrent suicidal behavior, gestures or threats, or self-mutilating behavior. The IPDE questions are part of the Composite International Diagnostic Interview (CIDI) version 3.0, a structured lay-administered interview [Reference Huang, Kotov, De Girolamo, Preti, Angermeyer and Benjet35]. These eight IPDE questions are answered in a true-false format, with the added number of true answers resulting in a total score (range 0–8). The internal consistency was low (α = 0.53), but expectedly so because a single IPDE item is designed to measure just one borderline trait. An IPDE score of 5 and higher can be considered as an indication of a BPD, because of the correspondence with the minimum level of required DSM symptoms (5 out of 9) to meet DSM-IV criterion A for a borderline personality disorder diagnosis. The cut-off of 5 out of 8 IPDE questions has repeatedly been demonstrated to be a valid method of assessing the presence of a borderline personality disorder [Reference Lenzenweger, Lane, Loranger and Kessler2,Reference De Graaf, Van Dorsselaer, Tuithof and Ten Have31,Reference Loranger, Sartorius, Andreoli, Berger, Buchheim and Jacobsberg34,Reference Magallón-Neri, Forns, Canalda, De La Fuente, García and González36].
Primary outcome
HR-QoL was assessed with the Medical Outcomes Study Short Form Health Survey (MOS SF-36) [Reference Ware and Sherbourn37]. The MOS SF-36 is commonly used in research to measure HR-QoL and has been validated in the general population [Reference Brazier, Harper, Jones, O’Cathain, Thomas and Usherwood38]. This self-report questionnaire consists of 36 items which ask how respondents felt over the last 4 weeks using different Likert scales (2-, 3-, 5- and 6-point Likert scales). The 36 items comprise in total 8 health domains or subscales, which culminate in a well-validated physical and mental component summary score [Reference Ware and Kosinski39].
Covariates
All covariates were selected on their putative association with both borderline personality traits and HR-QoL. As demographic characteristics, we included sex, age, and level of education [Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof and Kleinjan8]. Next, mood disorder (major depression, dysthymia, or bipolar disorder), anxiety disorder (panic disorder, agoraphobia, social phobia, specific phobia, or generalized anxiety disorder), and substance use disorder (alcohol/drug abuse or dependence) in the last 12 months were considered as three separate potential confounders. The presence of these disorders was assessed using the CIDI 3.0. The CIDI 3.0 is a fully structured psychiatric interview and a psychometrically sound instrument to assess common mental DSM-IV diagnoses in the general population [Reference Haro, Arbabzadeh-Bouchez, Brugha, De Girolamo, Guyer and Jin40]. Finally, the presence of somatic disorders (yes/no), based on self-reported presence of a chronic somatic disease (≥1 of 17 chronic physical disorders treated or monitored by a medical doctor in the past 12 months, assessed with a standard checklist, was considered a potential confounder).
Statistical analyses
Since the number of borderline personality traits was not normally distributed, neither after log-transformation, nor the number of respondents with five or more traits was low (n = 58), descriptive statistics are presented, stratified for persons with no, one, or two or more borderline personality traits. Differences between these three groups on the covariates and HR-QoL were tested with either a χ 2 test (for categorical variables) or one-way ANOVA (for continuous variables).
Next, we examined the association between all covariates as well as borderline personality traits (entered simultaneously as independent variables) with HR-QoL (dependent variable) by multiple linear regression analyses. Separate analyses were conducted for mental and physical HR-QoL.
Next, we examined whether the presence of borderline personality traits interacted with age in explaining variance in HR-QoL. In case of significant interaction (p < 0.05), results were stratified according to the presence of no, one, and two or more borderline personality traits. A sensitivity analyses was performed by testing the association between age and HR-QoL, stratified by presence of a borderline personality disorder (≥5 traits) or not. To facilitate clinical interpretation of results, we also explored the interaction between each borderline personality trait and age separately on explaining either physical or mental HR-QoL by multiple linear regression.
Analyses were based on unweighted data as we are primarily interested in associations between characteristics. Data were analyzed using SPSS version 26 [41]. p-values of <0.05 are considered statistically significant.
Results
Sample characteristics
In the total sample (age range 21–72), 71.3% reported having no borderline personality traits, while 24.1% had 1–2 traits, 3.5% had 3–4 traits, and 1.1% had ≥5 traits. Table 1 presents the baseline characteristics stratified by the numbers of borderline personality traits, that is none (n = 3,783, 71.3%), one trait (n = 936, 17.7%), or two or more traits (n = 584, 11.0%). The presence of borderline personality traits was significantly related to younger age, female sex, lower education level, higher somatic comorbidity, having a mood disorder, anxiety disorder, substance use disorder, and lower mental and physical HR-QoL (see Table 1).
Table 1. Baseline characteristics of participants (n = 5,303), stratified by the number of borderline personality traits.

Abbreviation: SD, standard deviation.
a One-way ANOVA or χ 2-test.
Association of borderline personality traits with HR-QoL
Multiple linear regression analyses showed that, without consideration of interaction terms, increasing age was related to lower physical HR-QoL but not to mental HR-QoL (see Table 2). Furthermore, an increasing number of borderline personality traits was significantly associated with lower mental HR-QoL and physical HR-QoL. The associations between borderline personality traits and HR-QoL were confirmed by a sensitivity analysis on the presence of BPD (5 or more traits) for both mental HR-QoL (B = −19.00 [standard error, SE = 1.75], β = −0.14, p < 0.001) and physical HR-QoL (B = −14.95 [SE = 2.34], β = −0.08, p < 0.001).
Table 2. Multiple linear regression analyses on health-related quality of life.

Abbreviations: QoL, quality of life; SE, standard error.
Interaction with age
Multiple linear regression analyses yielded a statistically significant interaction between borderline personality traits and age on the association with mental HR-QoL (one trait: p = 0.044; two or more traits: p < 0.001) as well as physical HR-QoL (one trait: p = 0.094; two or more traits: p < 0.022) in the fully adjusted models. Therefore, Table 3 presents the association between age and HR-QoL stratified by the number of borderline personality traits.
Table 3. Association between age and HR-QoL by multiple linear regression,a stratified by the number of borderline personality traits.
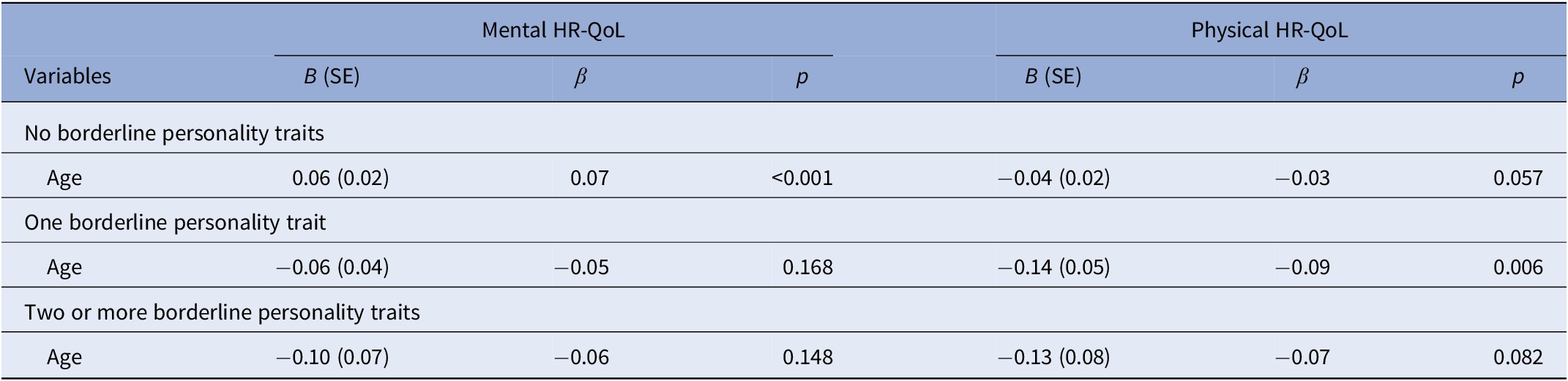
Abbreviation: HR-QoL, health-related quality of life.
a Adjusted for sex, level of education, somatic comorbidity, and psychopathology (presence of a mood disorder, presence of an anxiety disorder and presence of a substance use disorder).
The stratified analyses showed that among persons with no borderline personality traits, mental HR-QoL is better in older individuals compared to younger individuals. In contrast, among persons with one or two or more borderline personality traits, higher age was associated with a lower mental HR-QoL, albeit these effects were not significant. With respect to physical HR-QoL, irrespective of the number of borderline personality traits, an increasing age was associated with a worse HR-QoL. The impact of age, however, was lowest in the subgroup of persons without any borderline personality trait (see Table 3).
A sensitivity analysis of age by the presence of a borderline personality disorder (5 or more traits present, n = 58), also yielded a significant interaction of borderline by age with mental-HR-QoL (p = 0.003) as well as with physical HR-QoL (p = 0.033). Stratified analyses among persons with a borderline personality disorder showed a strong negative association between age and HR-QoL, although not statistically significant (mental HR-QoL: B = −0.29 [SE = 0.31], β = −0.13, p = 0.348; physical HR-QoL: B = −0.26 [SE = 0.31], β= −0.10, p = 0.417), in contrast to persons without BPD (mental HR-QoL: B = 0.04 [SE = 0.02], β = 0.04, p = 0.004; physical HR-QoL: B = −0.05 (SE = 0.02), β = −0.04, p = 0.007).
Post-hoc, we tested whether the association between the eight specific borderline personality traits interacted with age in explaining variance in either mental or physical HR-QoL. We found that four traits significantly interacted with age in explaining mental HR-QoL, that is chronic feelings of emptiness (p = 0.002), affective instability (p = 0.006), inappropriate, intense anger or difficulty controlling anger (p < 0.001) and transient, stress-related paranoid ideation or dissociative symptoms (p < 0.001). Furthermore, we also found four traits that significantly interacted with age in explaining physical HR-QoL, that is chronic feelings of emptiness (p < 0.001), affective instability (p = 0.031), impulsivity (p = 0.045), and transient, stress-related paranoid ideation or dissociative symptoms (p < 0.001). Table 4 presents the associations of age with either mental or physical HR-QoL stratified for the presence of the particular traits, for those traits which showed a significant interaction with age. Regarding mental HR-QoL, in persons with these specific personality traits increasing age is not associated with a better mental HR-QoL anymore. Regarding physical HR-QoL, in persons with these specific traits the association between increasing age and a lower physical HR-QoL becomes significantly stronger.
Table 4. Association between age and HR-QoL by multiple linear regression,a stratified by the presence of a specific borderline personality trait.b
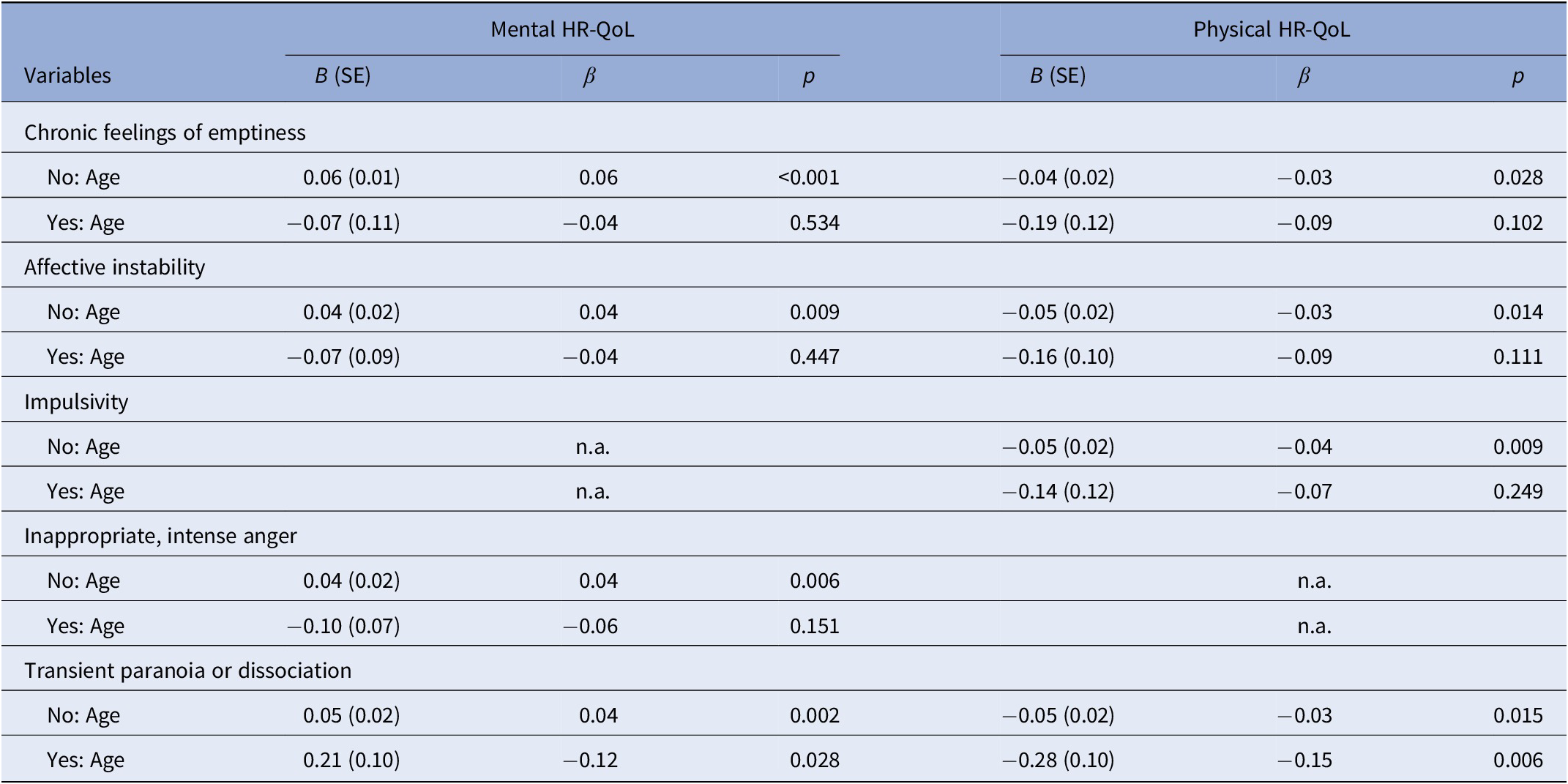
Abbreviations: HR-QoL, health-related quality of life; n.a., not applicable; SE, standard error.
a Adjusted for sex, level of education, somatic comorbidity, and psychopathology (presence of a mood disorder, presence of an anxiety disorder and presence of a substance use disorder).
b Only criteria with a significant interaction with age are presented.
Discussion
To the best of our knowledge, this is the first study presenting empirical findings on the impact of borderline personality traits on the relationship between age and HR-QoL in the general population including older persons. Previous studies on personality disorders in different life stages and QoL were confined to psychiatric samples [Reference Frías, Palma, Solves, Martínez and Salvador14], the physical component of HR-QoL [Reference Holzer and Huang17], or typically lacked respondents with BPD or established borderline personality traits [Reference Abrams, Alexopoulos, Spielman, Klausner and Kakuma15,Reference Holzer and Huang17]. Furthermore, adults older than 65 years were entirely absent in most samples [Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman7]. The present study demonstrates that presence of borderline personality traits modifies the association between age and both aspects of HR-QoL in line with our hypotheses. Older individuals possess a significantly better mental HR-QoL than younger adults, however, in the presence of one or more borderline personality traits, an increasing age was not associated with better mental HR-QoL anymore. This remained the case after controlling for mental disorders that frequently co-occur with borderline personality traits [Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof and Kleinjan8]. Furthermore, physical HR-QoL turned out to become lower with increasing age, but even more so in the presence of borderline personality traits. The association between age and HR-QoL was strongest among persons meeting the criteria for a borderline personality disorder, although not statistically significant due to the low number of respondents meeting the criteria for a borderline personality disorder. Nonetheless, even the presence of one borderline personality trait already resulted in differential associations between age and HR-QoL. This suggests that growing older with any number of borderline personality traits is associated with a higher level of mental and physical health issues, which has a negative impact on the QoL. Our results are in line with a previous study reporting that among patients with borderline personality disorder age was associated with a lower level of mental and physical HR-QoL [Reference Frías, Palma, Solves, Martínez and Salvador14].
We found that among persons without borderline personality traits an increasing age is associated with a higher mental HR-QoL. This contrasts with studies in the literature that describe a stable HR-QoL across different life stages, but these studies did not stratify by the presence of borderline personality traits [Reference Netuveli and Blane42]. Moreover, most previous studies may have been confounded by comorbid mental and somatic disorders. We adjusted for these comorbidities to estimate the impact of age itself on mental HR-QoL scores. The finding that older adults do not experience a decline in mental HR-QoL may be explained in the first place by older adults possessing better (passive) emotional coping skills that protect them when experiencing serious/negative life events such as bereavement or loss of a professional life [Reference Blanchard-Fields, Mienaltowski and Seay43]. As a deficiency in emotional coping skills is one of the core symptoms of borderline personality disorder, it is conceivable that older adults with borderline personality traits do not profit from the common development of emotional skills associated with aging [Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof and Kleinjan8]. Accordingly, events such as widowhood and divorce are indeed associated with a lower QoL in older adults with a personality disorder [Reference Condello, Padoani, Uguzzoni, Caon and De Leo16]. Another explanation is that borderline personality traits in themselves lead to more negative interpersonal life events which subsequently affect QoL [Reference Powers, Gleason and Oltmanns13]. Lastly, interaction between age and number of borderline personality traits on mental health related QoL might be confounded by differences in severity of particular traits between younger and older persons. One may imagine that milder traits may improve over time, while more severe traits may persist lifelong and have a stronger impact on QoL. Nonetheless, to explore this hypothesis the individual borderline personality traits should have been assessed dimensionally (for which valid assessment instruments are lacking).
Lower physical HR-QoL in older adults has also been associated with having a dependent, obsessive–compulsive or paranoid personality disorder [Reference Holzer and Huang17]. In the present study, we demonstrated that even subthreshold levels of borderline personality traits are related to lower physical HR-QoL when controlled for somatic comorbidity. Several explanations can be put forward. First, the presence of borderline personality traits may negatively interfere with coping with chronic somatic diseases. Secondly, personality disorders in general are related to a broad range of physical health problems, such as sleeping problems and physical pain, which do not necessarily translate into somatic disorders [Reference Dixon-Gordon, Conkey and Whalen44]. Moreover, borderline-related behavior such as auto-mutilation, suicide attempts, physical harm from impulsive decision making, and substance abuse may further contribute to physical disability, bad health behavior or worsen the course of already present chronic somatic diseases [Reference Doering45].
These results can have several practical implications, pertaining to various stages of life. Firstly, the lifelong harmful physical and mental effects emphasize that possession of borderline personality traits needs to be viewed as a serious risk factor for a person’s wellbeing throughout life. Borderline personality traits should be targeted by health policies and health care professionals from early on. Timely recognition of borderline personality traits and providing of the appropriate treatment may prevent the occurrence of comorbid physical and mental health problems that would otherwise accumulate with aging. Moreover, attention for all aspects of a healthy life (e.g., life style, physical health, and self-management) is justified, as has been advocated by others [Reference Doering45–Reference Hutsebaut, Videler, Verheul and Van Alphen47]. Secondly, as pertaining to later life stages, it would be erroneous to assume that absence of clinically established borderline personality disorder in older adults equals the absence of borderline-related health problems. It appears that while some behavioral borderline-related symptoms may diminish across the life span, underlying pathological personality traits remain stable. This concept is described as heterotypical continuity and is supported by several literature reviews [Reference Oltmanns and Balsis48–Reference Debast, van Alphen, Rossi, JHA, Bolwerk and JJL50]. It is conceivable that this would easily lead to under detection of borderline personality disorders in older adults, while missing clinically relevant personality pathology [Reference Balsis, Woods, Gleason and Oltmanns22]. This is even more relevant knowing the impact of subthreshold levels of borderline traits. As appears from our results of the specific borderline criteria, especially traits in the affective-internalizing domain such as chronic feelings of emptiness or affective instability may be considered as indicators of underlying pathology that is related to a lower HR-QoL with an increasing age (see Table 4). Studies that discuss the idea of heterotypical continuity also identify affective symptoms as the temporally stable traits in older BPD patients, as opposed to externalizing traits [Reference Beatson, Broadbear, Sivakumaran, George, Kotler and Moss18]. Our finding that low levels of borderline traits negatively affect older adults might also have implications for treatment. If affective symptoms reported by an older patient are indeed persistent and related to borderline personality traits, long-term insightful psychotherapy might be preferred over short-term symptom-based therapy. Schema therapy for example appears to be a good option, as the evidence of effectivity in older adults is taking shape [Reference Videler, van Alphen, van Royen, van der Feltz-Cornelis, Rossi and Arntz27]. In order to investigate the possibility that older adults with borderline personality traits can attain better levels of QoL by means of psychotherapy, more empirical research is needed.
Several limitations apply to the interpretation of the results as described above. Firstly, the described associations cannot be causally interpreted due to the cross-sectional nature of this study. Secondly, this study did not include socioeconomic factors that might serve as determinants of QoL in later life and might either explain or confound the association with borderline personality traits [Reference Pinquart and Sörensen51]. Since socioeconomic status is generally lower in the older population, our results may be even conservative estimates. Thirdly, while the IPDE can be considered a good psychometric instrument for general research purposes, the use of a self-report instrument might have led to underreporting of borderline personality traits [Reference Magallón-Neri, De la Fuente, Canalda, Forns, García and González52,Reference Samuel, Sanislow, Hopwood, Shea, Skodol and Morey53]. This has probably attenuated our findings. The addition of semi-structured interviews allowing interpretation of answers by well-trained clinicians would increase diagnostic accuracy of borderline personality traits.
Final conclusion
Borderline personality traits, even when the criteria for a full borderline personality disorder are not met, modify the association between age and HR-QoL. The presence of borderline personality traits precludes the increase of mental HR-QoL with age and results in a stronger decline in physical HR-QoL with age. Therefore, borderline personality traits should be treated as markers of serious health problems across the life span. Also, more attention is warranted from clinicians and researchers for subthreshold personality problems in middle-aged and older persons, in order to increase understanding of their impact on HR-QoL and improve diagnostics and treatment options in clinical practice. So that, hopefully, older patients also, instead of suffering ever more, can reap the benefits of aging.
Abbreviations
- BPD
borderline personality disorder
- HR-QoL
health-related quality of life
- CIDI
Composite International Diagnostic Interview
- IPDE
International Personality Disorder Examination
- MOS SF-36
Medical Outcomes Study Short Form Health Survey 36
- NEMESIS-2
Netherlands Mental Health Survey and Incidence Study-2
- QoL
quality of life
Conflicts of Interest
The authors declare that they have no conflicts of interest concerning this article.
Financial Support
NEMESIS-2 is conducted by the Netherlands Institute of Mental Health and Addiction (Trimbos Institute) in Utrecht. Financial support has been received from the Ministry of Health, Welfare and Sport, with supplementary support from the Netherlands Organization for Health Research and Development (ZonMw) and the Genetic Risk and Outcome of Psychosis (GROUP) investigators. The funding sources had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.









Comments
No Comments have been published for this article.