More than two-thirds of adolescents(Reference Eaton, McKnight-Eily and Lowry1,Reference Wheaton, Jones and Cooper2) and one-third of adults(Reference Liu3) do not get the recommended amount of sleep. Poor sleep behaviours increase the risk for a variety of negative outcomes, including poor dietary quality(Reference Córdova, Barja and Brockmann4–Reference Chaput16) and obesity(Reference Magee and Hale17–Reference Li, Zhang and Huang20). Although research has traditionally focused on sleep duration as a key contributor to poor diet and diet-related chronic diseases, there is growing interest in understanding the role of sleep timing, in particular late bedtime(Reference Chaput16,Reference Fleig and Randler21–Reference Jarrin, McGrath and Drake24) . Later bedtime could affect dietary behaviours and diet-related health outcomes through several pathways. For example, later bedtimes may be a driver of shorter sleep duration: individuals who go to bed later may not be able to compensate by sleeping later the next morning due to work, school and social schedules(Reference Gibson and Shrader25,Reference Giuntella and Mazzonna26) . In turn, shorter sleep duration has been associated with worse dietary quality(Reference Córdova, Barja and Brockmann4–Reference Chaput16). Later bedtime may also worsen dietary quality independently of its effects on sleep duration(Reference Golley, Maher and Matricciani23), as eating late at night is associated with higher energetic intake and lower dietary quality compared with eating at other times of day(Reference Chaput16,Reference Spaeth, Dinges and Goel27,Reference Baron, Reid and Kern28) .
While evidence suggests that later bedtime could contribute to both shorter sleep duration and less-healthy dietary choices, these questions remain understudied. Research has not investigated whether later bedtime is associated with shorter sleep duration. Likewise, only a handful of studies have examined the relationship between bedtime and dietary behaviours in adolescents(Reference Golley, Maher and Matricciani23,Reference Thellman, Dmitrieva and Miller29–Reference Agostini, Lushington and Kohler31) or adults(Reference Baron, Reid and Kern28,Reference Ogilvie, Lutsey and Widome32,Reference Mossavar-Rahmani, Weng and Wang33) , and none has been conducted in probability samples of the US population. These relationships are particularly important to assess in adolescence, emerging adulthood and young adulthood, as these are three key developmental stages for changing sleep patterns(Reference Maslowsky and Ozer34) and for the development of dietary behaviours and obesity(Reference Lawlor and Chaturvedi35–Reference Alberga, Sigal and Goldfield38). Understanding these associations will shed light on whether sleep timing is a potentially promising target for interventions aiming to improve sleep duration, dietary quality and weight.
To address these gaps, we examined cross-sectional associations between bedtime, sleep duration and eating behaviours using a large national probability sample followed in adolescence, emerging adulthood and young adulthood. Our objectives were to: (1) investigate the association between usual bedtime and sleep duration and (2) examine the association between usual bedtime and eating behaviours, independent of sleep duration. We examined cross-sectional associations within development stages, rather than longitudinal associations across these stages, because sleep behaviours are expected to exert relatively immediate impacts on eating behaviours. We hypothesised that: (1) later bedtimes would be associated with shorter sleep duration, and (2) later bedtimes would independently be associated with less healthy eating behaviours.
Methods
Study sample
We used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative sample of approximately 20 000 individuals recruited from middle and high schools in 1994–1995 and followed into adulthood(Reference Harris, Halpern and Whitsel39). We used data from wave I (collected in 1994–1995), wave II (1996), wave III (2001–2002) and wave IV (2008). Wave V did not assess sleep timing.
We examined participants in three developmental stages: adolescence (waves I and II, including participants age ≥12 and ≤18 years), emerging adulthood (wave III, age >18 and ≤24 years) and young adulthood (wave IV, age >24 and ≤34 years) (see online supplementary material, Supplemental Figs. 1–4), following previous studies(Reference Sokol, Grummon and Lytle40).
Measures
Usual bedtime
The main exposure variable was participants’ self-reported usual bedtime. In waves I and II, participants reported their usual bedtime on ‘weeknights’ during the school year (see online supplementary material, Supplemental Table 1 provides details on key study variables). In waves III and IV, participants reported their usual bedtimes for days when they go to work, school or similar activities (‘weekdays’) and for days when they do not have to wake up at a certain time (‘weekends’). We calculated a weighted average of these variables, following previous studies(Reference Krueger, Reither and Peppard41,Reference Larson, Dewolfe and Story42) . In all waves, we converted bedtimes to decimal hours after 12.00 hours (e.g. we coded a bedtime of 21.30 hours as 9·5), such that larger values indicated later bedtime.
Usual sleep duration
In waves I and II, participants self-reported usual sleep duration in hours/night. In waves III and IV, participants reported their usual bedtime and wake time for weekdays and weekends, as described above. We used responses to those items to calculate usual sleep duration in decimal hours (e.g. 30 min equals 0·5 decimal hours), again calculating a weighted average of sleep duration on weekdays and weekends.
Eating behaviours
We examined participants’ self-reported eating behaviours (online supplementary material, Supplemental Table 1). Different behaviours were assessed in each wave; for each wave, we identified eating behaviours that could be easily defined as ‘healthier’ or ‘less healthy.’ In wave I, data were available on whether the participant had consumed fruits, vegetables and sweets in the past day (coded as yes/no). In wave II, we examined consumption of fruits, vegetables, soda, pizza, desserts and sweets, and French fries in the past day (coded as yes/no), as well as on the frequency of fast-food consumption (days in past week ate fast food). In wave III, we examined frequency of fast-food consumption (days in past week ate fast food). Finally, in wave IV, we examined frequency of fast-food consumption (times in past week ate fast food) and amount of sugar-sweetened beverage consumption (number of sugar-sweetened beverages consumed in the past week).
Covariates
Covariates included potential confounders of the relationship between bedtime, sleep duration and eating behaviours, including sociodemographic characteristics (e.g. age, parental education and income to reflect socio-economic status, nativity), screen time behaviours and depressive symptoms(Reference Kruger, Reither and Peppard12,Reference Cappuccio, Taggart and Kandala18,Reference Golley, Maher and Matricciani23,Reference Thellman, Dmitrieva and Miller29–Reference Ogilvie, Lutsey and Widome32) (online supplementary material, Supplemental Table 1).
Statistical analysis
Analytic samples included participants with complete information on key variables and valid sampling weights. To reduce the influence of outliers, we decided a priori to remove outlying observations with implausible values on sleep duration and bedtime, excluding from analyses respondents further than 2·576 sd from sample means on these variables (online supplementary material, Supplemental Figs. 1 through 4), similar to previous studies(Reference Sokol, Grummon and Lytle40). Participants excluded from analysis due to missing or extreme data were similar to included participants in their average sleep duration, bedtime and eating behaviours, but differed slightly in some demographic characteristics (online supplementary material, Supplemental Table 2).
To evaluate the relationship between bedtime and sleep duration within each developmental stage, we estimated multivariable ordinary least squares models stratified by developmental stage, regressing sleep duration on bedtime and covariates. To examine the relationship between bedtime and each eating behaviour within each developmental stage, we regressed each eating behaviour variable on bedtime, stratifying by developmental stage and controlling for both sleep duration and covariates. We used logistic regression for dichotomous eating behaviour variables (e.g. ate fruit yesterday) and negative binomial regression for count variables (e.g. fast food times/week). We report adjusted OR and unstandardised coefficients/marginal effects (Bs). All analyses accounted for Add Health’s complex sampling design.
We conducted analyses using Stata version 15.1 (StataCorp LLC). The University of North Carolina Institutional Review Board granted human subjects’ research approval for this study.
Results
The analytic samples included 9427–13 048 individuals per wave (Table 1). Average sleep duration increased somewhat across waves. Average bedtime was similar in waves I, II and IV (22.30–22.42 hours), and later in wave III (24.06 hours).
Table 1 Sample characteristics by developmental stage, National Longitudinal Study of Adolescent to Adult Health*
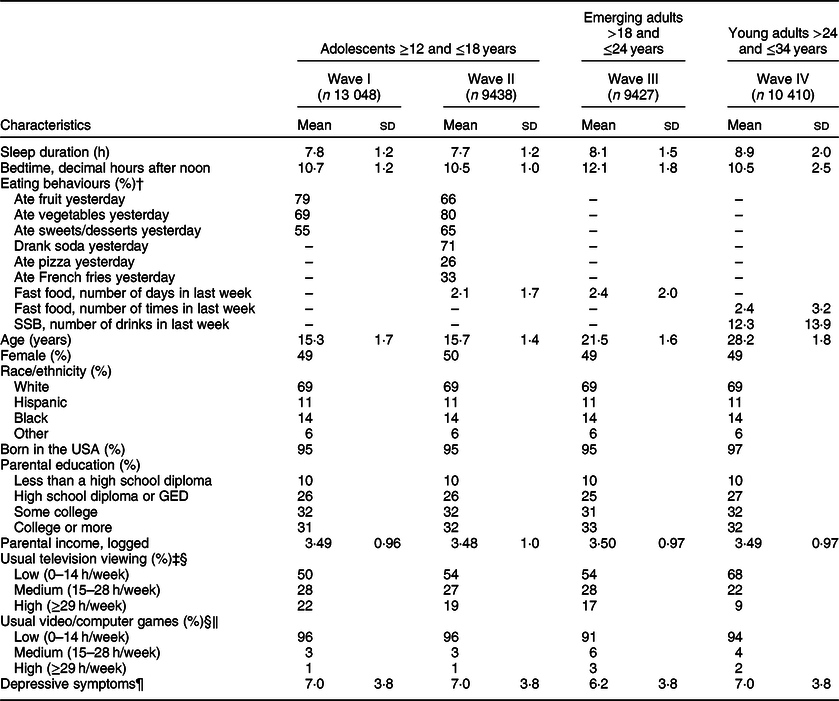
* Means, sd and % adjusted for complex survey features of Add Health. Eating behaviours listed as ‘–’ were not assessed in this survey wave.
† See online Supplementary material, Supplemental Table 1 for information on measurement of eating behaviours in each wave.
‡ Participants reported on the usual number of hours per week they spent watching television during the past 30 d.
§ We trichotomised screen time variables using the categories reported in Kruger et al. (Reference Kruger, Reither and Peppard12).
‖ Participants reported on the usual number of hours per week they spent playing video or computer games during the past 30 d.
¶ Sum score on the nine items from Center for Epidemiological Studies Depression Scale(Reference Eaton, Smith, Ybarra and Maruish55) that were assessed in all four waves. Score on each item ranged from 0 to 3 yielding a possible sum scores of 0–27, where higher scores indicate more depressive symptoms.
In all developmental stages, later bedtime was associated with shorter sleep duration, independently of demographic characteristics, screen time behaviours and depressive symptoms (range of Bs: –0·55 to –0·23 h/night, all Ps < 0·001, Table 2). Associations between bedtime and sleep duration significantly differed across the four waves (adjusted Wald test F (3,126) = 82·12, P < 0·001). The negative association was strongest among young adults, for whom going to bed 1 h later was associated with a reduction in usual sleep duration of 0·55 h (~33 min) per night.
Table 2 Association of later bedtime with usual sleep duration, by developmental stage, National Longitudinal Study of Adolescent to Adult Health*
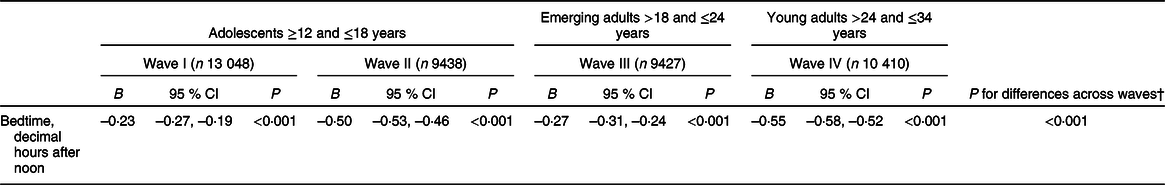
* Table shows the association between bedtime and usual sleep duration in hours/night from regressions of sleep duration on bedtime, controlling for age, sex, race/ethnicity, nativity, parental educational attainment, logged parental income, usual time spent watching television, usual time spent playing video/computer games and depressive symptoms. Bedtime was calculated in decimal hours after 12.00 hours, such that larger values indicate later bedtimes. Bs reported are unstandardised regression coefficients. All analyses accounted for complex survey features of Add Health.
† P value reported is for an adjusted Wald test examining whether all coefficients were equal in seemingly unrelated estimation, F(3,126) = 82·12.
Generally, later bedtime was also associated with less healthy eating behaviours in each development stage, even after controlling for usual sleep duration (Fig. 1). Of the thirteen associations tested, all but two were statistically significant (Ps < 0·05) and all the significant associations were in the expected direction, with later bedtime being associated with less healthy eating behaviours. Only eating sweets yesterday as reported by adolescents in wave 1 (adjusted OR: 0·06, P = 0·08) and eating French fries yesterday as reported by adolescents in wave 2 (adjusted OR: 1·06, P = 0·08) were not significantly associated with bedtime, though the associations were in the expected directions. Stronger associations were seen between bedtime and consumption of fruits and vegetables in adolescents, bedtime and the frequency of fast-food consumption in adolescents, and bedtime and sugar-sweetened beverage consumption in young adults.
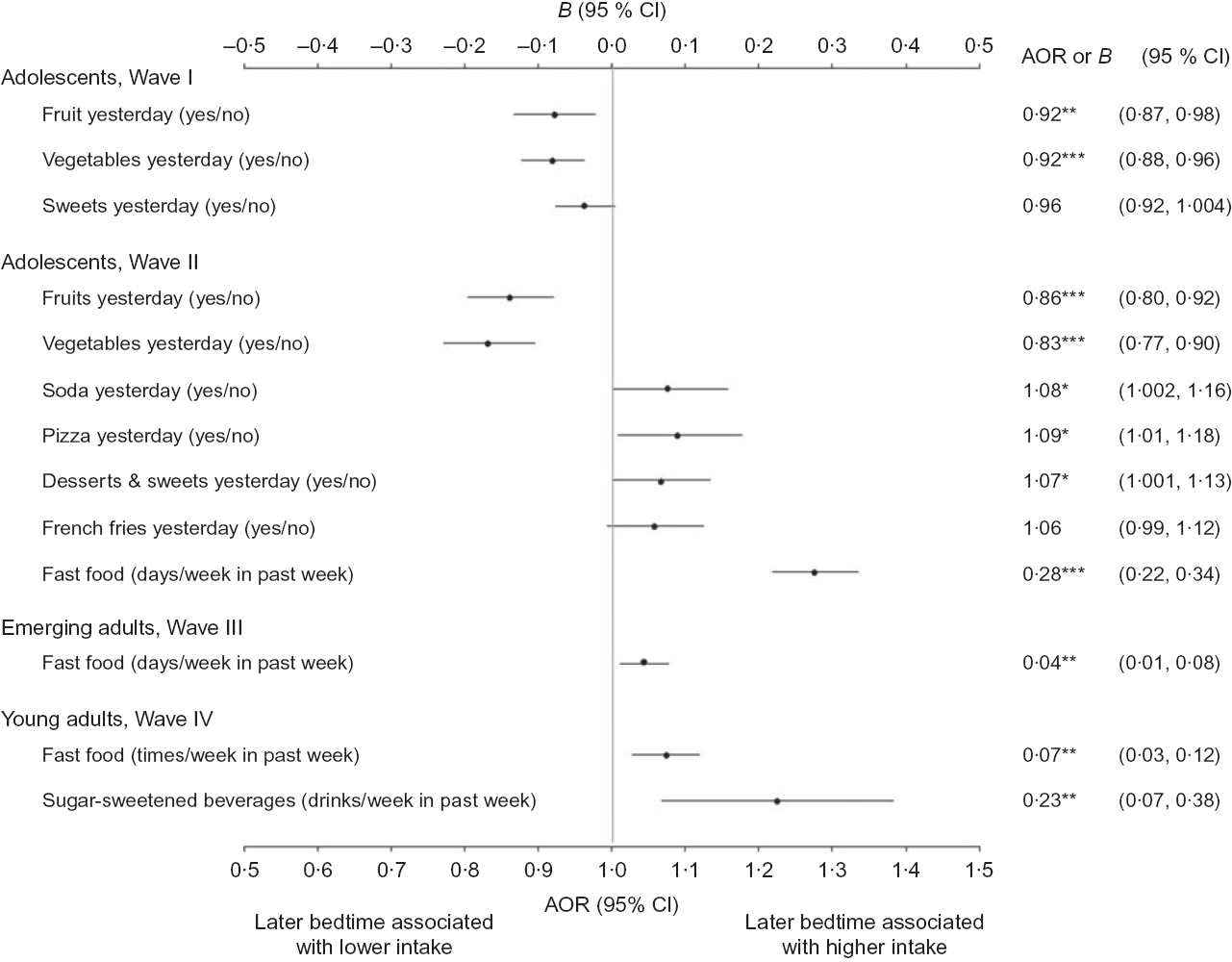
Fig. 1 Associations of later bedtime with eating behaviours, controlling for sleep duration, National Longitudinal Study of Adolescent to Adult Health. Figure shows associations between bedtime and eating behaviours. Bedtime was calculated in decimal hours after 12.00 hours, such that larger values indicate later bedtimes. Figure shows unstandardised regression coefficients (Bs) for continuous outcomes (top horizontal axis) and adjusted OR (AOR) for binary outcomes (bottom horizontal axis), controlling for usual sleep duration, age, sex, race/ethnicity, nativity, parental educational attainment, logged parental income, usual time spent watching television, usual time spent playing video/computer games and depressive symptoms. All analyses accounted for complex survey features of Add Health. *P < 0·05, **P < 0·01, ***P < 0·001
Discussion
In this cross-sectional study with a large national sample, bedtime was negatively associated with sleep duration among adolescents, emerging adults and young adults. Going to bed 1 h later was associated with 14–33 fewer minutes of usual sleep duration per night. This reduction could be clinically meaningful: previous studies have found that a 1-h reduction in usual sleep duration is associated with an 80 % increase in odds of obesity among adolescents(Reference Gupta, Mueller and Chan43) and a 0·35 kg/m2 increase in BMI among adults(Reference Cappuccio, Taggart and Kandala18).
Across developmental stages, later bedtimes were generally associated with reporting lower consumption of healthier foods and higher consumption of less healthy foods. For example, adolescents who reported later bedtimes had lower odds of fruit and vegetable consumption and higher odds of consuming soda, desserts and pizza. Likewise, later bedtime was associated with greater frequency of fast-food consumption in all developmental stages. These findings are consistent with studies examining bedtime and eating behaviours in non-national samples(Reference Golley, Maher and Matricciani23,Reference Thellman, Dmitrieva and Miller29,Reference Agostini, Lushington and Kohler31,Reference Ogilvie, Lutsey and Widome32) . While some of the observed associations were small, the consistent pattern of results suggests that these small associations could add up to meaningful differences in overall dietary quality and diet-related health outcomes. For example, fruit and vegetable consumption(Reference Aune, Giovannucci and Boffetta44) and fast-food intake(Reference Pereira, Kartashov and Ebbeling45) have been found to be associated with health outcomes such as heart disease and insulin resistance.
Several mechanisms could underlie the observed associations between bedtime and eating behaviours. For example, those who go to bed later may be eating more energy-dense snacks that are convenient for late night eating, contributing to higher energetic intake and lower dietary quality compared with eating during other times of day(Reference Chaput16,Reference Spaeth, Dinges and Goel27,Reference Baron, Reid and Kern28) . Another possibility is that poorer sleep behaviours are a marker for a general profile of riskier behaviours, rather than later bedtime being a driver of less healthy dietary choices, though research on this question is mixed(Reference Larson, Dewolfe and Story42,Reference Dumuid, Olds and Lewis46–Reference Kaar, Schmiege and Vadiveloo49) . Additional research should also explore the complex interplay of sleep behaviours, diet, adiposity, and hunger, satiety, and growth hormones(Reference Beccuti and Pannain50–Reference Spiegel, Tasali and Leproult52).
Strengths of our study include its use of a large population-based national sample, examination of three developmental stages critical to the development of eating behaviours and obesity(Reference Lawlor and Chaturvedi35–Reference Alberga, Sigal and Goldfield38), and inclusion of important potential confounders in analyses, particularly screen time(Reference Chaput16) and depressive symptoms(Reference Chang, Ford and Mead53). By examining the cross-sectional relationships over three developmental periods, we demonstrate that the behaviours co-vary during each developmental stage and that some behavioural patterns are stable across developmental stages.
Limitations of our study include the inconsistency of eating behaviour questions used across the four waves and our inability to examine overall dietary quality. Another limitation is that sleep behaviours were self-reported. While self-reported and objectively measured sleep variables are significantly correlated(Reference Lauderdale, Knutson and Yan54), future research should examine these associations using gold standard measures of sleep whenever possible. Third, we used complete case analysis to account for missing data. While participants included in analysis had similar sleep and eating behaviours as those excluded from analysis, we cannot rule out sample selection bias. Finally, we cannot rule out alternate explanations for the observed associations, including residual confounding and reverse causality (i.e. eating certain foods causes individuals to go to bed later).
Conclusions
In a national probability sample, later bedtime was associated with shorter sleep duration during adolescence, emerging adulthood and young adulthood. Further, later bedtime was generally associated with less healthy eating behaviours, even after controlling for sleep duration. Given the cross-sectional design of this study, future research using longitudinal and experimental designs is needed to clarify the relationships between bedtime, sleep duration and eating behaviours. If bedtime is causally related to eating behaviours and sleep duration, encouraging earlier bedtimes could be a promising strategy to incorporate into interventions aiming to improve eating behaviours, increase sleep duration or prevent obesity.
Acknowledgements
Acknowledgements: The authors thank the Add Health study team at the University of North Carolina. Financial support: General support and training support for A.H.G. were provided by the Carolina Population Center (P2C HD050924 and T32 HD007168), and training support for R.L.S. was provided by the Carolina Consortium for Human Development (T32 HD07376). The funders had no role in the study design; collection, analysis or interpretation of the data; writing of this report; or decision to submit the manuscript for publication. Conflicts of interest: None. Authorship: A.H.G. conceptualised the study, analysed the data, drafted the initial manuscript, and reviewed and revised the manuscript. R.L.S. contributed to data preparation analysis, provided intellectual input on study design and interpretation, and critically reviewed the manuscript. L.A.L. provided intellectual input on study design and interpretation and critically reviewed the manuscript. All authors reviewed and approved the final content. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the University of North Carolina Institutional Review Board. This study used de-identified secondary data.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020002050






