Malnutrition is ‘a state resulting from lack of intake or uptake of nutrition that leads to altered body composition and body cell mass leading to diminished physical and mental function and impaired clinical outcome from disease’(Reference Sobotka1,Reference Cederholm, Barazzoni and Austin2) . It affects 13–78 % of the elderly adults(Reference Guigoz3), causing high morbidity and mortality(Reference Chang4–Reference Jeejeebhoy, Keller and Gramlich6) and economic impact on society(Reference Malafarina, Reginster and Cabrerizo7).
The Global Leadership Initiative on Malnutrition recently recommended malnutrition diagnostic criteria. The criteria include the presence of at least one phenotypic criterion (non-volitional weight loss, low BMI and reduced muscle mass) and at least one aetiologic criterion (reduced food intake or assimilation and disease-related inflammation)(Reference Cederholm, Jensen and Correia8). However, Global Leadership Initiative on Malnutrition criteria are more focused on clinical indicators needed to diagnose malnutrition and less concentrated on nutritional risk assessment. Nutritional risk was defined as having any of the following: (i) involuntary loss ≥10 % of usual body weight within 6 months, (ii) involuntary loss ≥5 % of usual weight in 1 month, (iii) BMI < 18·5 or >25 kg/m2, (iv) chronic disease, (v) increased metabolic requirements, (vi) altered diet or (vii) inadequate dietary intake for >7 d(Reference Cederholm, Barazzoni and Austin2,Reference White, Guenter and Jensen9) . The European Society for Clinical Nutrition and Metabolism recommends that all subjects at the time of the first contact with healthcare services should undergo nutritional screening using validated screening tools(Reference Cederholm, Barazzoni and Austin2).
The choice of the screening instruments depends on several factors, such as the setting of the study population (community dwelling v. institutionalised/hospital based) and the simplicity of the screening. Cost-effectiveness, validity carried out for the local languages and applicability of the tool to a broader community also play contributing role(Reference Wham, Redwood and Kerse10).
Validated Mini Nutritional Assessment – Long Form has been commonly used for the last 20 years to screen the nutritional status of patients and diagnose malnutrition among both community dwellers and inpatients(Reference Guigoz, Vellas and Garry11–Reference Vrdoljak15). Power et al. (Reference Power, Mullally and Gibney16) identified an additional thirty-three screening instruments (mainly in the form of questionnaires), validated to be used across different environments.
Recent meta-analysis explored the validity of seventeen screening instruments to identify malnutritional risks among community-dwelling seniors. The results suggested that the Mini Nutritional Assessment – Short Form (MNA-SF), either using BMI (MNA-SF-V1) or calf circumference (MNA-SF-V2), and Seniors in the Community: Risk Evaluation for Eating and Nutrition, version II (SCREEN II) have a good sensitivity and fairly specificity and therefore might be more reliable to detect malnutritional risk in the community-dwelling setting as compared with other screening tools(Reference Isautier, Bosnić and Yeung17).
Mini Nutritional Assessment – Long Form and MNA-SF have been commonly used in family medicine practices of Bosnia and Herzegovina to detect malnutrition. SCREEN II underwent significant reliability analyses in two validation studies, carried out in Canada (n 193)(Reference Keller, Goy and Kane18) and New Zealand (n 45)(Reference Wham, Redwood and Kerse10), exclusively in the English language, and concerning a small sample size.
When compared with the other validated assessments methods, such as nutritionist’s risk rating, it is still unknown if MNA-SF or SCREEN II is more or less effective in screening for nutritional risk among the elderly Bosnian population group.
The current study aimed to compare MNA-SF and SCREEN II as each was used to analyse the prevalence of nutritional risk among Bosnian and Herzegovinian community-dwelling people aged 65 years and above.
Materials and methods
The cross-sectional study was carried out from August to October 2019 and included community-dwelling seniors over 65 years of age from three towns in Bosnia and Herzegovina. The municipalities of Foca, East Sarajevo and Bijeljina were selected purposely. With a population size of 37 182 people older than 65 years, living in these municipalities, the margin of error being ±5 %, 95 % CI and at 3·4 % CI, the minimal sample size was calculated to be 813.
Community-dwelling seniors were selected by the method of systemic sampling. Sampling frames were listed of the senior citizens aggregated across the family practices in each of the three towns. Every third person from the listings was invited by his/her family practice staff to participate in the study. Seniors who were previously diagnosed and treated for any of the following conditions: mental illness, dementia, malignancy, stroke or chronic renal failure (Stage III−V) were not included in the study.
Nutritional risk assessment
Three researchers (primary care providers) underwent 2 weeks of training with the research nutritionist, which included theory and practical training in nutritional assessment, data recording and the analysis. For the purpose of research, a standardised health checklist was created. The list was divided into several sections: (i) socio-demographic characteristics, (ii) general health (co-morbidities, medications), (iii) dietary habits, (iv) social risk factors, (v) basic and instrumental activities of daily living, (vi) cognitive functioning and (vii) anthropometric measurements. A 24-h diet recall questionnaire was used to assess the usual meals, portion size, cooking method and nutrient intakes. Household measures were used to define the portion size calculation.
The researchers carried out the standardised nutritional assessments and recorded the data under the supervision of the nutritionist. To standardise the performance and verify the similarity of the assessment results, sixteen geriatric patients coming to the clinic on week 3 for their regular check-up were asked to undergo multiple nutritional assessments. Nutritionist and three researchers performed the assessment separately with 24 h between the assessments, blinded with respect to each other’s results. Intra-class correlation coefficient for inter-rater reliability (0·803) indicated rater agreement. Intra-rater reliability was tested on weeks 4 and 5. Each rater performed the nutritional assessment of fifteen different patients and repeated the assessment on that group of patients 7 d later. Intra-class correlation coefficient ranged between 0·718 and 0·836, and intra-rater reliability was considered good.
In the main study, one researcher per site performed a standardised nutritional assessment during the face-to-face interview. Katz index (six items)(Reference Katz, Down and Cash19) and the Lawton scale (eight items)(Reference Lawton, Moss and Fulcomer20) evaluated the ability to perform basic and instrumental activities of daily living (higher scores presented higher functioning and independence). The internal consistency of the Bosnian version of Katz index and Lawton scale was considered good (α = 0·874) and excellent (α = 0·952).
Cognitive functions were assessed with the Mini-Cog screening test, including three-item recall and clock drawing test (CDT). One point was allocated for each recalled word (range 0–3). The CDT was considered normal if all numbers were present in the correct sequence and position, and the hands legibly displayed. Patients with the recall of 1–2 words were classified based on the CDT as demented (CDT abnormal) or non-demented (CDT normal). The internal consistency of the Mini-Cog test, based on the Cronbach’s coefficient value of 0·827, was considered good. The sensitivity and specificity of Mini-Cog are 99 and 96 %, respectively(Reference Borson, Scanlan and Chen21).
Standardized techniques were used to measure the mid-arm circumference, calf circumference and BMI(22). After double-checking for completeness and quality, data recordings (except MNA-SF and SCREEN II results) were provided to the research nutritionist.
The nutritionist carefully evaluated the recorded data and provided a probability nutritional risk rating based on a standardised framework, previously used for the validation of SCREEN II in Canada and New Zealand(Reference Wham, Redwood and Kerse10,Reference Keller, McKenzie and Goy23) . Framework criteria have six domains: body composition, weight changes, medical history, diet-related risk factors, other risk factors (physical functioning, living arrangements) and diet. Domains were rated from 0 (low risk) to 10 (high risk) for each study participant individually. Overall rating score was then assigned to one of the three risk categories: low risk (<5), medium risk (5–7) and high risk (>7).
Screening instruments
Before the study started, MNA-SF and SCREEN II questionnaires were translated from English to Serbian language (one of the three languages spoken in Bosnia and Herzegovina) using the dual-panel methodology(Reference Swaine-Verdier, Doward and Hagell24). After the interpreters reached the consensus on the translation, different people reviewed the translation for accuracy and the equivalence of the language.
The pilot testing of questionnaires was carried out with a sample of twenty-five community dwellers, with the mean age of 74·72 years. The principal investigator first administered MNA-SF, waited 10 min and then administered SCREEN II. The interviewees were asked to give their feedback in regard to the understandability of the questions. They considered both questionnaires easy to understand and to answer. However, participants suggested two adjustments in the translation of SCREEN II, using the word ‘glass’ instead of ‘cup’ for estimation of fluid intake and ‘kilograms’ instead of ‘pounds’ for weight change self-assessment. Dr Heather Keller, the author of SCREEN II, approved the adjustments. It took a mean time of 3 min to complete MNA-SF and 5 min to complete SCREEN II.
The researchers administered questionnaires during the main study in face-to-face interviews.
MNA-SF included six items as follows: food intake decline, weight loss, mobility, suffered psychological stress, neuropsychological problems and BMI. Total score was categorised as malnutrition (≤7), a risk of malnutrition (8–11) and normal nutritional status (12–14)(Reference Guigoz, Vellas and Garry11).
SCREEN II composed of fourteen items, with two sub-questions that were scored to equal the total score of 64. The items scored <2 were considered indicators of potential nutritional risk. A total score lower than 50 indicated high risk, 50–53 moderate risk and >53 low nutritional risk(Reference Keller, Goy and Kane18).
Statistical analysis
The statistical analysis was done using the Statistical Package for Social Science version 25 (SPSS; IBM, Inc.). Mean values and sd for continuous variables and numbers/percentages for categorical variables were used to describe outcomes. The mean scores for MNA-SF and SCREEN II were calculated. The internal consistency of the MNA and SCREEN II instrument was analysed by calculating the Cronbach’s coefficient and their reliability with the intra-class correlation coefficient. The linear relationship between the scores was measured with Pearson’s correlation coefficient. The validity of MNA-SF (0–14) and SCREEN II scores (0–64) was compared separately with the research nutritionist risk rating score (0–10). Sensitivity and specificity of proposed cut-off points in the detection of nutritional risk were assessed using receiver operating characteristic curves in relation to any risk (≥5) and high risk (>7) as the criterion. Validity of a questionnaire was considered as good (sensitivity and specificity >80 %, AUC > 0·8), fair (sensitivity or specificity <80 %, but both >50 %, AUC 0·6–0·8) and poor (sensitivity or specificity <50 %, AUC < 0·6)(Reference van Bokhorst-de van der Schueren, Guaitoli and Jansma25). As a level of statistical significance, the usual value of P < 0·05 was taken.
Results
The study included 821 community-living seniors. Of those, 448 (55 %) were females and 373 (45 %) males, with an average age of 74·10 ± 5·41 years. The majority of participants had primary education (37·6 %), were widowed (47 %), had a hobby (66 %), social support (75 %), lived with a spouse or children (61 %) and performed independently basic (93·7 %) as well as instrumental activities of daily living (95·1 %). Eighty percentage of the study participants rated their health as good to excellent. Mini-Cog assessment screened 36 % of respondents positive for cognitive impairments. The mean number of chronic diseases per participant was 2·52 ± 1·58 and of medications 4·92 ± 2·71. The average clinical indicators’ scores are presented in Table 1. The mean score for SCREEN II was 45·9 ± 7·52, with a range 21–60, and for MNA-SF 10·66 ± 1·21 (range 4–14).
Table 1 Demographic and clinical characteristics of study participants
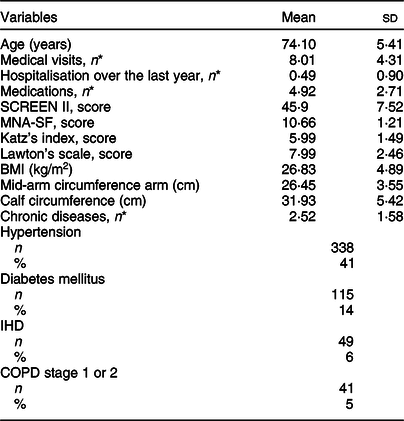
SCREEN II, Seniors in the Community: Risk Evaluation for Eating and Nutrition, version II; MNA-SF, Mini Nutritional Assessment – Short Form; BMI, body mass index; IHD, ischemic heart disease; COPD, chronic obstructive pulmonary disease.
SCREEN II score <54 indicates nutritional risk. MNA-SF score ≤11 indicates nutritional risk. Katz index score (0 = dependent, 6 = independent). Lawton scale score (low functioning = 0, high functioning = 8).
* Mean numbers are given per participant.
Sixteen percentage of the participants lost >2·5 kg and 11 % gained >2·5 kg in the past 6 months. In 8 % of cases, these weight changes were unintentional. In regard to the risk factors, 7 % reported fair or poor appetite, 19 % skipped meals often and 18 % limited certain food. Swallowing and chewing difficulties were found in 37 and 57 % of cases. Seven percentage often had problems in getting their groceries, while 13 % ate their meals alone. Nineteen percentage of the participants perceived cooking as a chore. Most of the participants took ≤3 servings of fruit and vegetables (65 %), ≤1 meat or alternatives servings (70 %), ≤2 milk product servings (94 %) and ≤5 cup fluid a day (48 %). Sixty-nine percentage used no meal supplements.
The Cronbach’s α coefficient for the SCREEN II was 0·640, which indicated that the internal consistency level for the SCREEN II was fair. For the questions set, the values ranged from 0·538 to 0·675. The intra-class correlation coefficient for this questionnaire was 0·610 (moderate reliability).
The Cronbach’s coefficient for the MNA-SF questionnaire was 0·466, and the intra-class correlation coefficient 0·461, suggesting insufficient internal consistency and reliability. A statistically significant, positive, moderate linear relationship (r 0·684, P < 0·001) was found between MNA-SF and SCREEN II. The prevalence of high nutritional risk per nutritionist’s risk rating, SCREEN II and MNA-SF was 26, 60 and 7 %, respectively. The correlation of nutritionist’s risk assessment with MNA-SF (r −0·192, P < 0·001) and SCREEN II (r −0·655, P < 0·001) was inverse and statistically significant, but these relationships were weak and moderate, respectively (Table 2).
Table 2 Nutritionist’s risk rating, Mini Nutritional Assessment – Short Form (MNA-SF) and Seniors in the Community: Risk Evaluation for Eating and Nutrition, version II (SCREEN II) scores
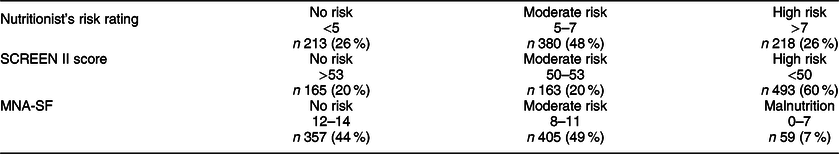
With the nutritionist’s rating score ≥5 as a criterion, the MNA-SF cut-off point of ≤11 (indicating any risk) had poor sensitivity (55·7 %), specificity (46·6 %) and AUC (0·563; P = 0·024). When the criterion of >7 was applied, good sensitivity (95·3 %) and specificity (88·9 %) were obtained for MNA-SF cut-off score of ≤7. AUC for this comparison was 0·742 (considered fair). Cut-off points of <54 (AUC = 0·816) and <50 (AUC = 0·881) for SCREEN II (indicating moderate and high risks) corresponded with good sensitivity (82·2 %; 80·9 %) and fair specificity (72·1 %; 75·0 %) (Table 3 and Fig. 1).
Table 3 Comparison of sensitivity and specificity for Seniors in the Community: Risk Evaluation for Eating and Nutrition, version II (SCREEN II) and Mini Nutritional Assessment – Short Form (MNA-SF)
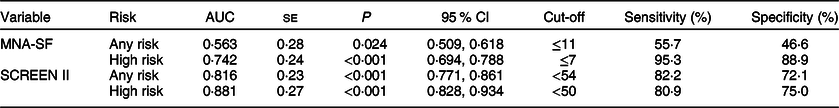
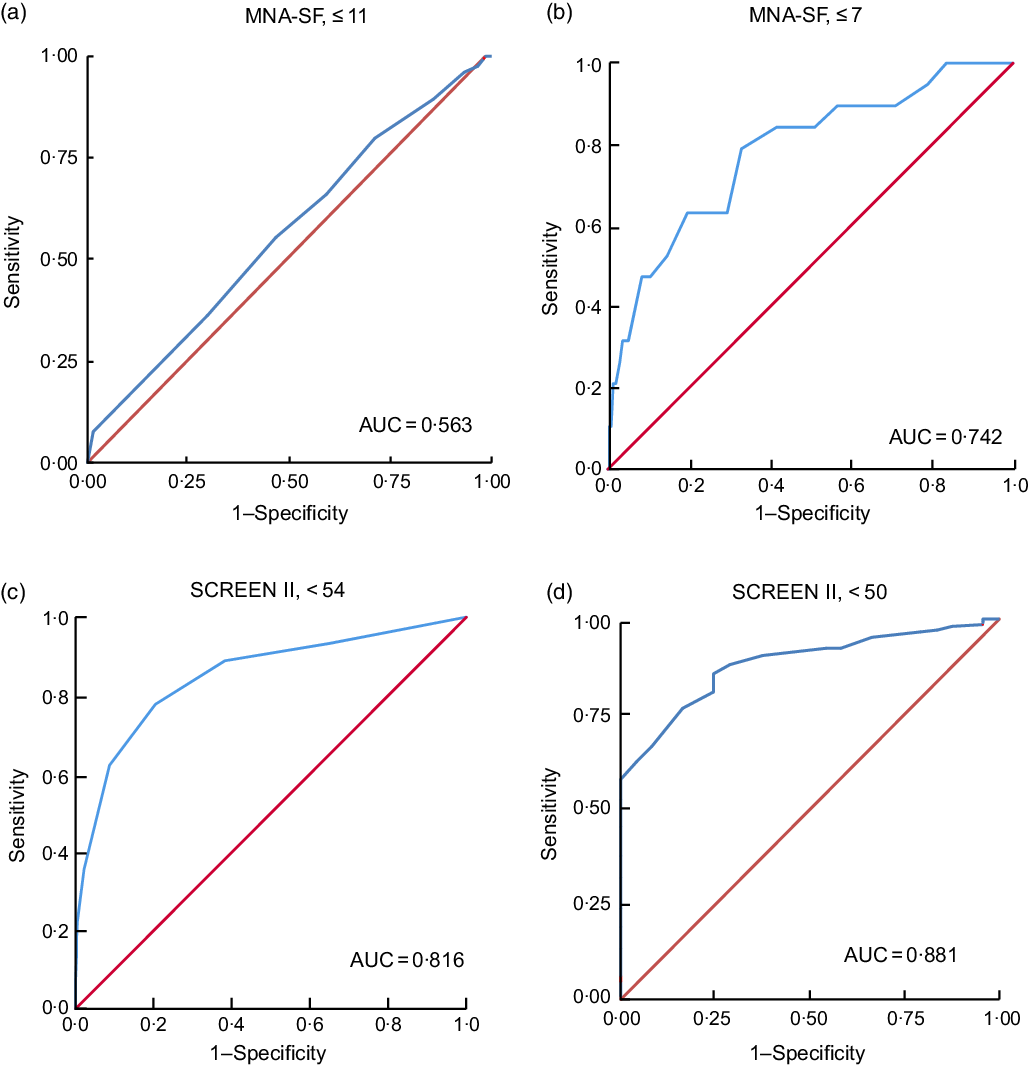
Fig. 1 The receiver operating curves showing sensitivity and specificity of (a) MNA-SF ≤11 (any risk), (b) MNA-SF ≤7 (high risk), (c) SCREEN II <54 (any risk) and (d) SCREEN II <50 (high risk) in identifying nutritional risk compared to nutritionist’s risk rating. MNA-SF, Mini Nutritional Assessment – Short Form; SCREEN II, Seniors in the Community Risk Evaluation for Eating and Nutrition, version II; AUC, area under the curve
Discussion
The current study compared the validity of SCREEN II and MNA-SF in the screening of nutritional risk among elderly community-dwelling individuals.
The sensitivity of the Serbian translation of SCREEN II was lower for both <54 (moderate nutritional risk) and <50 (high nutritional risk) cut-off points; however, specificity to detect nutritional risk was higher in comparison with the original, validation study in Canada(Reference Keller, Goy and Kane18). When compared with the validation study in New Zealand, sensitivity of cut-off point <54 was slightly lower in the current study, but specificity values corresponded(Reference Wham, Redwood and Kerse10). The former study also identified a score of <49 as a new cut-off point to assess high risk among octogenarians, with a sensitivity of 90 % and specificity of 86 %. In the current research, the sensitivity of the cut-off points of <50 was good, specificity fair; moving the cut-off point down the scoring scale did not add much to the accuracy of SCREEN II in identifying high nutritional risk. Although the validation of the Serbian SCREEN II followed the methods used in the previous validation studies, some methodological differences might have had an impact on the outcomes, such as bigger sample size, majority of participants (37·6 %) having only primary education or less (v. 17·5 % in Canada and 15·6 % in New Zealand) and belonging to the age range of 66–99 years (55–99 years in Canada and 85–86 years in New Zealand).
The findings of the current study contradict the results of systematic reviews, which compared the validity of different screening tools among the community-dwelling elderly population(Reference Isautier, Bosnić and Yeung17,Reference Račić, Ivković and Kusmuk26) . A meta-analysis of Isautier et al. (Reference Isautier, Bosnić and Yeung17) demonstrated good sensitivity and specificity for MNA-SF cut-off point ≤11 to identify individuals at the risk of malnourishment. Račić et al. (Reference Račić, Ivković and Kusmuk26) concluded that MNA-SF has good and SCREEN II has satisfactory reliability and validity for the screening of malnutrition in community dwellers. Discordance between the current and the previous studies may be attributed to the validation methodology of the studies included in systematic reviews. Except for the research by Sarikaya et al. (Reference Sarikaya, Halil and Kuyumcu27), validating MNA-SF against nutritional assessment performed by two geriatricians independently, all of the other studies validated MNA-SF against Mini Nutritional Assessment – Long Form. The validation has been potentially subjected to bias as the first six questions are the same(Reference Power, Mullally and Gibney16). On the other hand, previous studies were focused on differentiating the malnourished from well-nourished individuals, but not on nutritional risk in general. Although the validity of MNA-SF ≤ 7 (malnutrition) was good to fair in the current study, internal consistency and reliability were insufficient. The accuracy of cut-off point ≤11 (moderate risk) to classify an older adult as at nutritional risk was weak, which corroborates the finding of Molina Luque et al. (Reference Molina Luque, Muñoz Díaz and Martínez-de la Iglesia28) that MNA-SF has a very limited role in nutritional screening.
Based on a detailed clinical risk rating, nutritional risk was prevalent among community-dwelling seniors in Bosnia and Herzegovina. Previous international studies noted a lower prevalence of risk in high-income(Reference Wham, Redwood and Kerse10,Reference Westergren, Khalaf and Hagell29–Reference Naidoo, Charlton and Esterhuizen31) and a higher prevalence in low-income countries(Reference Damayanthi, Moy and Abdullah32,Reference Lahiri, Biswas and Santra33) . Ageing is associated with the presence of numerous factors potentially influencing dietary practices, such as lack of motivation for cooking, physical disability, chronic diseases, polypharmacy, diminished taste or smell, grieving, depression or poor nutritional habits adopted in younger ages(Reference Leslie and Hankey34). Multi-morbidity also impacts nutritional intake and total protein loss, ultimately leading to malnutrition and poor treatment outcomes(Reference Leslie and Hankey34). Therefore, nutritional screening should be an inseparable part of daily care for geriatric populations in primary healthcare.
The implementation of accurate and reliable screening instruments in family practices influences the process of identifying elderly individuals who need clinical (detailed) nutritional assessment and referral for professional counselling(Reference Skipper, Ferguson and Thompson35). According to AUC and sensitivity, the validity of SCREEN II to identify seniors with nutritional risk is good, but its fair specificity suggests more than 25 % of the screened population would be misclassified or have false-positive results. Internal consistency level (α < 0·70) may explain discordance between nutritionist’s risk rating and SCREEN II scores as well as the overestimation of high nutritional risk grade.
The author of the SCREEN II recommended to involve individuals with cut-off point <54 in nutrition education and those with cut-off points <50 in comprehensive professional assessment or potential treatment(Reference Keller, Goy and Kane18). However, if to be used for a screening purpose in family practices in Bosnia and Herzegovina, our recommendation is that obtaining a score <54 requires further clinical nutritional assessment.
Strength and limitations
To our knowledge, this is the first study comparing the validity of SCREEN II and MNA-SF in identifying community-dwelling seniors at nutritional risk. The questionnaires were validated against the standardised framework. The study was conducted consistently by the same researcher in each of the three study sites.
Several limitations need to be discussed. Study sites were selected purposively and may not be representative of community-dwelling seniors in Bosnia and Herzegovina. Because of the study design, the test−retest assessments of SCREEN II and MNA-SF were not performed. Only one 24-h diet recall may have not been sufficient to characterise dietary intake in study participants. The evaluation of recorded data, even while using the standardised assessment protocol, may have its shortfalls in comparison with the method of interviewing participants one-to-one by nutritionist.
As dietary and weight change assessment was self-reported and relied on memory, recall bias was possible. There might be variables influencing nutritional status not analysed in the current study.
Conclusion
To improve the nutritional status of the geriatric population, primary care institutions need to focus on the implementation of screening procedures. Before choosing a specific nutritional screening tool, healthcare providers need to explore its diagnostic accuracy in measurements supported in the use of each screening tool. MNA-SF has a good validity but poor reliability to distinguish malnourished from well-nourished seniors. Its role in identifying moderate nutritional risk among community-dwelling seniors in Bosnia and Herzegovina may be also limited due to low sensitivity, specificity and reliability. SCREEN II has promising results in regard to validity, but future studies to identify community-dwelling seniors with nutritional risk are required.
As significant diversities in nutritional risk assessment exist, objective, professional nutritional assessment should be carried out whenever feasible.
Take away points
-
Nutritional risk among community-dwelling seniors is prevalent (74 %); therefore, implementation of nutritional screening programmes in primary care settings is recommended.
-
MNA-SF is an inadequate tool for identifying or grading nutritional risk in community-dwelling population in Bosnia and Herzegovina.
-
SCREEN II has modest validity for identifying community-dwelling seniors at nutritional risk, but further studies are warranted.
Acknowledgements
Acknowledgements: We would like to thank Dr Heather Keller, the author of SCREEN II, for permission to translate SCREEN II and valuable discussion. We would also like to thank research assistants and family physicians for their efforts and contributions to the research. Financial support: The current study was supported by a grant awarded by the Ministry for Scientific and Technological Development, Higher Education and Information Society of the Republic of Srpska, Bosnia and Herzegovina, contract no. 19/6-020/961-113/18. Conflict of interest: There are no conflicts of interest. Authorship: J.R.P. and M.N.R. conceived the research question, design of the study and wrote the first draft of the manuscript. J.R.P., Z.S.V., O.V.K. and N.M.I. were responsible for the data collection in their towns. J.R.P. completed analyses and displayed analyses in draft tables. M.N.R. and M.Ž.M. provided guidance on the interpretation of results. All authors reviewed drafts of the paper, provided editorial suggestions and reviewed the final submitted draft. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by Ethical Review Board of Faculty of Medicine Foca, University of East Sarajevo – no. 01-2-1. Written informed consent was obtained from all patients.







