The purpose of this article is to describe a series of recent studies from the authors and many of their colleagues aimed at improving the food environments of adolescents in the Netherlands and thereby improving their food choices. These studies were performed in the wider context of national and local strategies for the prevention of overweight and obesity in the Netherlands.
Obesity in adolescents in the Netherlands
The Netherlands does not have a health examination survey to assess the nationwide prevalence of overweight and obesity with measured heights and weights of adolescents and it is therefore difficult to give a reliable estimate of the overweight and obesity figures. There are local surveys carried out by the municipal health services but these usually are not annually carried out for every age group and are based on self-reported height and weight. Also Statistics Netherlands has carried out annual health interview surveys based on the self-report of height and weight and the overall average response rate was 45–50 %(1). This suggests that prevalence data are probably an underestimation of the true prevalence, especially since the response rates are lowest in groups with lower socioeconomic position where the obesity prevalence is higher(2).
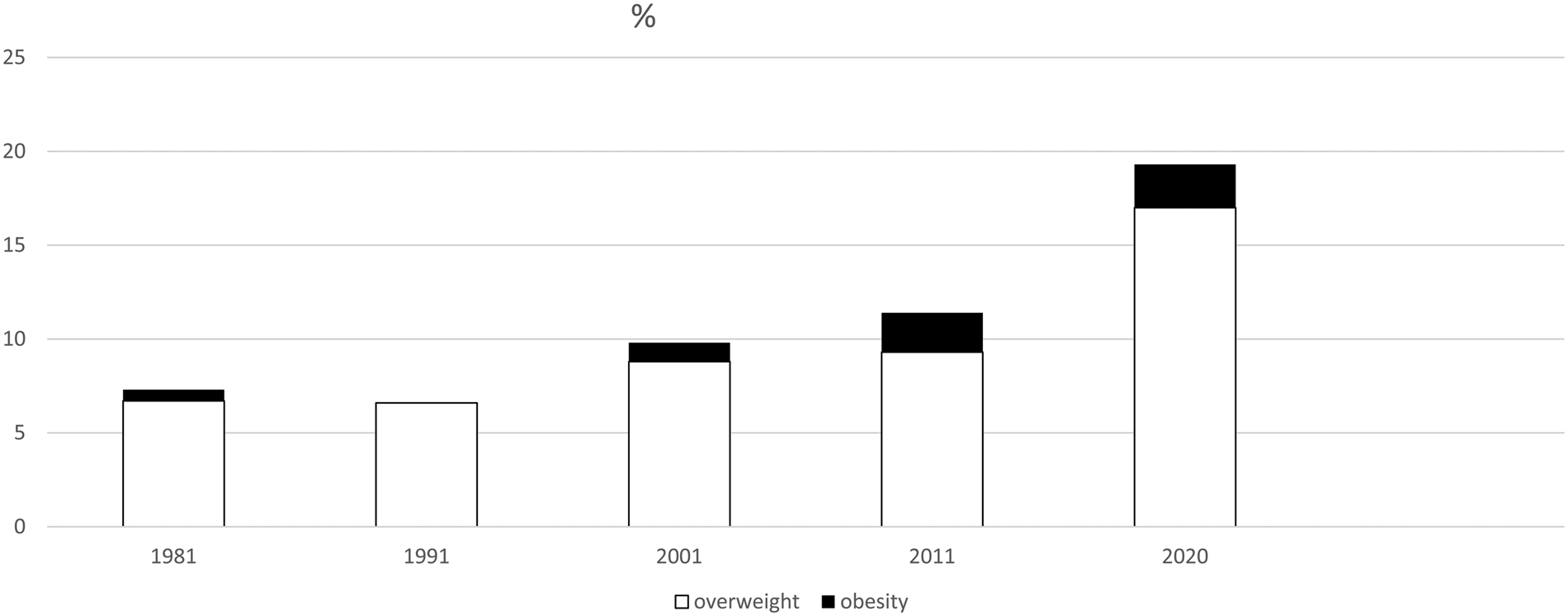
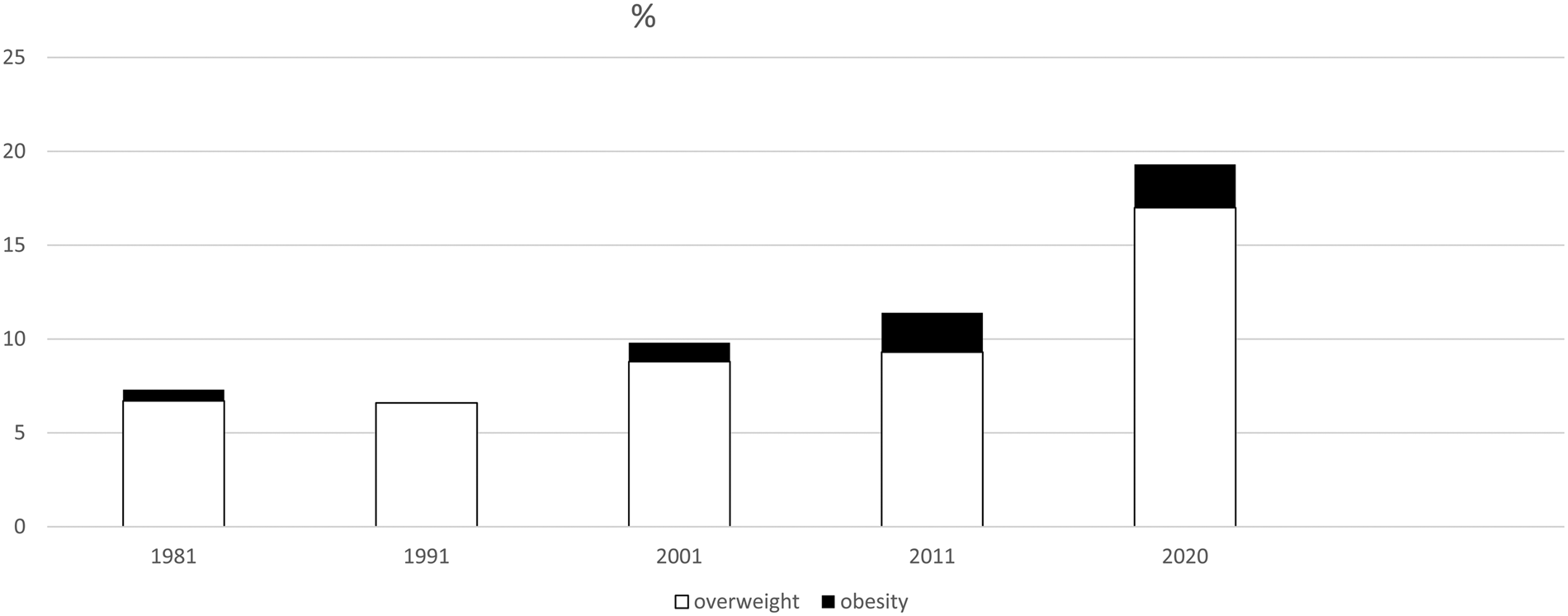
Fig. 1 shows the prevalence of overweight and obesity in 12–16 years old Dutch children in selected years (10 years apart) for the past 40 years(1). Similar trends are observed for boys and girls. Overweight and obesity are defined based on the international Cole cut points that correspond with a BMI between 25 and 30 kg/m2 for adults(Reference Cole and Lobstein3). The figures suggest that there was a sharp increase in 2020 (the year during which partial lockdowns were carried out because of the COVID-19 epidemic). The combined prevalence of overweight and obesity for 2019 was about 15 % in both boys and girls(1). This is slightly lower than the 2020 prevalence but also noticeable higher than 2011. Whether or not 2020 was an exceptional year or reflects a continued increase in overweight and obesity remains to be seen in the upcoming years.
Overall local and national policies aimed at reducing obesity in adolescents
As has been described recently elsewhere, there are a number of national and local policies in the Netherlands that are aimed at prevention and management of obesity in population in general and in adolescents(Reference Seidell and Halberstadt4). For example, In the Dutch national prevention agreement, seventy organisations set around 200 agreements on how the Netherlands can become healthier in 2040 in terms of smoking, overweight and alcohol abuse. For instance, manufacturers stated that they will make sugary sweetened beverages, candy and dairy products healthier(5).
The national policies in the Netherlands rely heavily on self-regulation by stakeholders such as supermarkets, restaurants and the food industry and are considered to be insufficiently effective to achieve the targets set by the national prevention agreement in 2040(5). The National Institute of Public Health and the Environment together with public health experts has recommended additional policies to reduce obesity. These targets (as described elsewhere(Reference Seidell and Halberstadt4)) include the reduction of the prevalence of overweight and obesity to those in the Netherlands two decades ago. The most strongly recommended policy was to raise the prices of unhealthy products and lower those of healthy products. Taxes could, for instance, be levied on sugary drinks and the VAT on products in the wheel of five (based on the Dutch food-based dietary guidelines) could be removed. The experts also suggest that stricter agreements should be made with employers regarding healthy food in the workplace and that fast food should be sold in fewer places(Reference Seidell and Halberstadt4). Another study assessed the level of implementation of national government policies which have a (potential) influence on the healthiness of the food environment in the Netherlands(Reference Djojosoeparto, Kamphuis and Vandevijvere6). The authors concluded that the Dutch government is lagging behind with policies that are having the potential to improve food environments for children such as a ban on marketing of unhealthy foods to children, price regulations and fast-food outlets in the vicinity of schools and propose several policy actions that could improve Dutch food environments(Reference Djojosoeparto, Kamphuis and Vandevijvere6).
The most sustained and most widely implemented programme to reduce childhood obesity levels in the Netherlands is ‘youth at a healthy weight’ (JOGG)(Reference Seidell and Halberstadt4). This programme was first implemented in 2010 and currently 183 municipalities participate in this programme. JOGG is a programmatic local approach that was originally modelled on the French programme EPODE (‘Ensemble Prévenons ‘l Obésité Des Enfants’; together we prevent obesity in children)(Reference Van Koperen, Jebb and Summerbell7). EPODE is a large-scale, centrally coordinated, capacity-building approach for local communities to implement effective and sustainable strategies to prevent obesity.
A recent study evaluated data of over 200 000 children who either lived in municipalities that implemented JOGG or in municipalities without JOGG were compared for the period 2013–1018(Reference Kobes, Kretschmer and Timmerman8). The results showed that overweight prevalence decreased from 25 to 16 % in JOGG areas whereas the prevalence in non-JOGG areas changed from 14 to 13 %. These results also show that municipalities that had higher prevalences of obesity were thus more likely to implement JOGG. The reduction in obesity was particularly large in municipalities where JOGG was implemented for at least 6 years (the prevalence was reduced from about 32 to 18 %). Important was that the decrease in prevalence was mainly visible in lower socioeconomic neighbourhoods in the long-term JOGG areas(Reference Kobes, Kretschmer and Timmerman8).
The city Zwolle (north-east of the Netherlands, 119 000 inhabitants in 2010) was the first city to formally adopt the integrated JOGG approach (under the name Zwolle healthy city approach) and it has been evaluated what different stakeholders after 10 years of implementation considered to be key elements that contributed to the success of the Zwolle healthy city approach(Reference Wilderink, Bakker and Schuit9). These stakeholders identified the following key elements:
(1) collaboration between a variety of local organisations that want to have an impact on the health of citizens;
(2) support for the approach on the strategic, tactical and operational level of involved organisations;
(3) proper communication and coordination, both for the network and within the organisations;
(4) embeddedness in organisations' policies and processes;
(5) collaboration with private organisations is of added value, although there is no ‘one size fits all’(Reference Djojosoeparto, Kamphuis and Vandevijvere6) collaboration with citizens;
(6) profiling the approach like a brand;
(7) moving along with and taking advantage of opportunities;
(8) continuous monitoring and evaluating goals and processes, and learning from the results;
Although this integrated approach seems to be effective in reducing the levels of obesity and in diminishing social inequalities in obesity, it is impossible to understand which interventions are effective on their own. This may, of course, not be needed or even possible because the effectiveness of an integrated approach may just be dependent on the synergy of interventions. Whilst effect-sizes of isolated interventions in single settings may therefore be very small or even absent and they may still be an essential component of an integrated approach. However, many of the stakeholders such as supermarkets would like to know what the effects of interventions may be for their business so that they can assess their costs and benefits. Therefore, we evaluated several isolated interventions to improve food environments or dietary habits. In the following sections, we describe some concrete examples of interventions in adolescents.
Interventions in the school environment
Unlike many countries in Europe, the Netherlands has no tradition of serving a school-lunch and schools have autonomy in terms of how they arrange their food and drink provision. It is common that children bring a packed lunch from home to school, or go home for lunch during a lunch break and that they eat a cold meal during lunch time that mainly consists of bread with different kinds of toppings, water or a package of fruit juice. Most secondary schools (for children aged 12–18 years) in the Netherlands have a canteen where students can purchase additional lunch products (e.g. sandwiches) and other products such as snacks and drinks. Since 2003, the Netherlands Nutrition Centre supports secondary schools to create a healthier school canteen (v. with the ‘healthy school canteen programme’)(Reference Evenhuis, van Wezenbeek and Vyth10). This programme is commissioned and financed by the Dutch Ministry of Health, Welfare, and Sports and is available to all Dutch secondary (vocational) schools. Part of this was the development of the guidelines for healthier canteens in 2014. The guidelines combine the offer of healthier products, including tap water, (availability) with the promotion and placement of these healthier products (accessibility), and anchoring policy(Reference Evenhuis, van Wezenbeek and Vyth10). It aims to support stakeholders creating healthier canteens through three incremental levels: bronze, silver and gold, although only the levels silver and gold are sufficient to be designated a healthier school canteen. After the development of the guidelines, the next step was their implementation. Evenhuis et al.(Reference Evenhuis, van Wezenbeek and Vyth10, Reference Evenhuis, Vyth and Veldhuis11, Reference Evenhuis, Vyth and Veldhuis12) created tools to support the implementation and evaluated the effect on food purchases. In conclusion, the offered support resulted in healthier canteens. However, there was no direct effect on total school canteen food purchases during the intervention(Reference Evenhuis, Jacobs and Vyth13).
The main reason for the lack of effects on total food purchases was that adolescents in the Netherlands bring most food and drinks from home and additionally buy only a small proportion of additional foods inside the school but purchase a much greater share of snacks and drinks outside school in supermarkets or food outlets close to the school(Reference Evenhuis, Jacobs and Vyth13). Attention to the home environment and the environment around school is therefore needed. Different relevant stakeholders such as parents, shopkeepers and local policy makers should be actively involved in this approach. Moreover, a healthy school environment not only consists of a healthy canteen, including vending machines, but also includes food education, integration with other health promotion school policies(Reference Evenhuis, Vyth and van Nassau14).
Interventions in supermarkets in the school environment
School canteens are important but they only have a minor contribution to food consumption of adolescents during school time. About 70 % of the adolescents studied by Huitink et al. brought foods from home to school, and 89 % of the adolescents reported purchasing foods and drinks in shops and supermarkets outside the school(Reference Huitink, Poelman and Seidell15). From our previous study, we know that foods not contributing to a healthy diet are currently the default in school food environments, and that this is somewhat more the case for schools located in neighbourhoods with lower socioeconomic position(Reference Timmermans, Dijkstra and Kamphuis16). Huitink et al. observed that the supermarket was the main driver of unhealthy food purchases during school hours(Reference Huitink, Poelman and Seidell15). In the Netherlands, these unhealthy foods and drinks are also those most heavily promoted(Reference Hendriksen, Jansen and Dijkstra17). A total of 72 % of the adolescents reported purchasing unhealthy foods and drinks from nearby supermarkets and the three most frequently purchased products included potato chips, savoury pastries and salty snacks and sport- and energy drinks, sugary drinks and water(Reference Huitink, Poelman and Seidell15). Although the cheaper options are usually multi-buy options elsewhere in the store, the presence of unhealthy snacks and drinks at the checkout counters is also an important place for impulse buying of snacks and drinks. Huitink et al. investigated the placement of healthier snacks at checkout counters would either promote healthy or discourage unhealthy snack purchases at the checkouts in the supermarket(Reference Huitink, Poelman and Seidell18, Reference Huitink, Poelman and Seidell19). This approach was combined with pricing interventions whereby discount was applied to these healthier snacks. The placement of healthier snacks at checkouts was associated with a relatively small number of healthier snacks sold but did not lead to a substitution of unhealthy snack purchases with healthier alternatives, neither did an additional price discount. The only placement strategy that limited unhealthy snack purchases was the replacement of the entire unhealthy snack assortment at the checkout with healthier alternatives but this also lead to considerable loss of revenue for the supermarket which makes it an unlikely strategy to be implemented voluntarily by supermarkets(Reference Huitink, Poelman and Seidell19).
Peer education in supermarkets
Since peers play a critical role in the psychosocial development of most adolescents, we investigated the usefulness of peer education as a health promotion strategy in adolescents. Peer education is defined as a system of delivering knowledge that improves social learning and provides psychosocial support. Huitink et al.(Reference Huitink, Poelman and Seidell15) developed a nutrition peer education intervention in supermarkets where young supermarket employees (aged 15–21 years) were trained as healthy supermarket coaches and conducted workshops for adolescents (aged 12–14 years) in order to support healthier food purchases in the supermarket during school hours. Huitink et al.(Reference Huitink, Poelman and Seidell15) observed that nutrition peer education in supermarkets improved adolescents' self-reported determinants of food purchase behaviour, including nutritional knowledge, attitudes and social support towards healthy food purchases. However, adolescents did not improve their actual food purchases in the supermarket. These results are not consistent with the results of previous school-based nutrition peer-education programmes, which showed improvements in, among others, self-reported fruit and vegetable intake after the programmes among adolescents. One difference compared to the studies by Huitink et al. is that those studies used questionnaires to measure food intake, which resulted in self-reported data that are known to be subject to bias. Huitink et al.(Reference Huitink, Poelman and Seidell15) used cash receipt data, which are known to be an objective measure of food purchases. From these studies, we confirm earlier findings that improvements in knowledge and attitudes towards healthier food choices may not result in affect-improved food choices. Unhealthy food choices appear to be too dominant in affecting food purchases because they tend to be tasty, ready-to-eat, cheap, available and heavily marketed.
Participatory action research with adolescents
Wilderink et al.(Reference Wilderink, Bakker and Schuit20) tried to engage young adolescents (10–14 years of age) in developing interventions aimed at healthier food choices. They involved children living in three low-socioeconomic position neighbourhoods in the Netherlands in participatory action research by using the photovoice method. The photovoice method provided comprehensive information from the children's perspectives(Reference Wilderink, Bakker and Schuit20). With the help of the community workers, the children identified feasible actions. It was concluded that it is possible to involve children from low socioeconomic position neighbourhoods in a meaningful way. It was recognised that it is important to start with a concrete question or problem and adapt the participatory action research project to the local context and skills of participants. It is not yet known, however, if these actions will be implemented.
Another large study of several Dutch research groups focused on children in the ages between 10 and 14 years in a relatively low-income neighbourhood in Amsterdam (the LIKE programme). The LIKE programme(Reference Waterlander, Pinzon and Verhoeff21) focuses on the transition period from 10 years old to teenager and was implemented in collaboration with the Amsterdam healthy weight programme. The aim was to develop, implement and evaluate an integrated action programme at the levels of family, school, neighbourhood, health care and city. This study combines systems thinking with participatory action research principles where the target group works in co-creating with the researchers and other stakeholders. We first obtained a dynamic picture of the pre-existing systems that shape adolescents' behaviour relating to diet, physical activity, sleep and screen use by the use of causal loop diagrams. Together with children (aged 10–14 years) and stakeholders, we are developing a subsequent action programme that is dynamic and adaptive, including quick actions focusing on system elements (quick evaluating, adapting and possibly catalysing further action) and more long-term actions focusing on system goals and/or paradigm change. The programme is supported by a developmental systems evaluation, supplemented with routinely collected data on weight status and health behaviour change over a period of 5 years. In the coming years, we will report how this approach has worked to provide a robust understanding of the programme's effectiveness within a complex dynamic system.
Conclusions
In the present paper, we shared some of our experiences of engaging with stakeholders in local interventions aimed to improve the food environment and dietary habits of adolescents in the wider context of national and local policies. It seems that current national policies in the Netherlands are largely ineffective in reducing the prevalence of overweight and obesity. Local integrated programmes in the Netherlands, however, seem to result in a reduction of overweight, especially in low-income neighbourhoods. It is impossible to say which elements of such an integrated approach are effective elements on their own. We found very little evidence for the effectiveness of separate interventions aimed at small changes in the food environment. This suggests that such interventions are only effective in combination with each other and in a wider systems approach. Future studies are needed to further develop the practical methodology of implementation and evaluation of systems science in combination with participatory action research.
Acknowledgements
The authors would like to thank all their colleagues and study participants who were involved in the studies described in the present paper. The authors would particularly like to acknowledge the contributions of Carry Renders, Wilma Waterlander, Lisa Wilderink, Marlijn Huitink and Irma Evenhuis.
Financial Support
None.
Conflict of Interest
None.