Introduction
Dietary diversity is consuming different food groups within 24 h of the assessment.(1) It illustrates the impression that increasing food variety and quality helps people get enough of the essential nutrients they need.(Reference Madzorera, Isanaka and Wang2) Pregnancy adds to a woman’s normal nutritional needs by increasing nutrient requirements to maintain maternal metabolism demand and foetal growth.(Reference Diana, Christianti and Anwar3) Proper nutrition before and during pregnancy plays a crucial role in decreasing adverse outcomes like intrauterine growth restriction, low birth weight, preterm delivery, intrauterine foetal death, and congenital anomalies.(4) A monotonous diet pattern increases the likelihood of poor micronutrient intake, whose deficiency can result in maternal undernutrition.(Reference Ayensu, Annan and Lutterodt5) In addition, pregnant women often have low and decreasing levels of micronutrients in their blood. To address this issue, it is advisable to promote the maintenance of dietary diversity as a beneficial and potentially sustainable strategy for achieving a well-rounded nutrient intake during pregnancy.(6) Dietary diversity is therefore considered very crucial to providing an adequate supply of nutrients for both the mother and the developing foetus.(Reference Willy, Judith and Peter7,Reference Custodio, Kayikatire and Fortin8)
Maternal nutritional status during pregnancy has a lasting, multigenerational impact that affects not only the health and survival of the women but also that of their children.(Reference Darnton-Hill9) A pregnant woman with higher dietary diversity assures micronutrient adequacy that minimises the risk of developing a deficiency or excess of any one nutrient. Consuming micronutrient-rich foods such as fruits, vegetables, meat, and fortified foods throughout pregnancy is critical for a healthy pregnancy and improved maternal health.(Reference Tefera, Brhanie and Dereje10)
According to the WHO report, the burden of micronutrient malnutrition among pregnant women is still alarmingly high across regions and countries.(4) Micronutrient deficiencies are estimated to account for about 7.3% of the global burden of diseases, and millions of pregnant women are deficient in vitamin A, iron, folate, zinc, or iodine.(Reference Ayensu, Annan and Lutterodt5)
In Africa, where maternal mortality is exponentially higher than in other regions, the extent and consequence of micronutrient deficiency among pregnant women remain unacceptably high.(Reference Darnton-Hill9) In sub-Saharan Africa, maternal micronutrient deficiencies are persistent and a key contributor to morbidity, mortality, and poor birth outcomes such as preterm birth, stillbirth, and low birth weight.(Reference Azene, Aragaw and Wubetie11)
In a systematic review, Azene (2021) found that only 41% of pregnant women in Ethiopia had adequate dietary diversity.(Reference Azene, Aragaw and Wubetie11) Despite the implementation of different nutritional policies, micronutrient deficiencies continued to account for a substantial proportion of poor birth outcomes in Ethiopia.(Reference Zerfu and Biadgilign12,Reference Zerfu, Umeta and Baye13) Even though some studies were conducted in some parts of Ethiopia, the prevalence of adequate dietary diversity and determinant factors varies across studies. Thus, a better understanding of the factors associated with dietary diversity is critical for preventing the risk of micronutrient deficiencies and helps design appropriate interventions by health policymakers to tackle the problem. Therefore, this study aimed to assess the dietary diversity and associated factors among pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Eastern Ethiopia.
Materials and methods
Study setting, design, and period
An institution-based cross-sectional study was conducted at Hiwot Fana Specialized University Hospital (HFSUH), which is located in Harar, 526 kilometres to the east of Addis Ababa. HFSUH is a major referral hospital for the Eastern part of Ethiopia, including Dire Dawa City Administration, Oromia, Ethiopian Somali, and Harari regions. The hospital has 312 beds and 15 case teams to provide services in all specialties. We conducted the study from April 28, 2021, to May 28, 2021.
Source population, study population, and eligibility criteria
All pregnant women receiving antenatal care (ANC) at Hiwot Fana Specialized University Hospital were the source population. All pregnant women receiving ANC at Hiwot Fana Specialized University Hospital during the data collection period were the study population. Pregnant women selected by systematic random sampling technique and participated in the actual data collection interview were the study units. We included all pregnant women receiving ANC at Hiwot Fana Specialized University Hospital during the data collection period. However, we excluded those who were unable to provide information due to a serious illness from the study.
Sample size determination and sampling procedure
A single population proportion formula was used to calculate a sample size, assuming a 95% confidence level, 5% margin of error, 10% non-response rate, and 53% proportion of adequate dietary diversity from a study conducted in Gojjam, Ethiopia.(Reference Yeneabat, Adugna and Asmamaw14) Accordingly, the total sample size was 420. The study participants were selected using a systematic random sampling technique. The sampling interval K was determined by dividing the average number of pregnant women who attended antenatal care follow-up per month at HFSUH by the desired sample size, (i.e. kth value 1166/420 = 3). After randomly selecting the first study participant, subsequent study participants were chosen at every third interval until the total sample size was attained and interviewed at exit from ANC service.
Measurement and data collection tools
Data were obtained from face-to-face interviews using a structured questionnaire. The questionnaire was adapted from the Food and Agriculture Organization (FAO) following guidelines outlined for the calculation of minimum dietary diversity for women of reproductive age, Food and Nutrition Technical Assistance (FANTA) Project household food insecurity access scale,(1,Reference Kearney15) and from different literature, which was pertinent to the topic.(Reference Zerfu and Biadgilign12–Reference Yeneabat, Adugna and Asmamaw14) It consisted of three groups of participants’ characteristics, namely, socio-demographic, dietary information, and food security information, which was prepared in English and translated to local languages (Afan Oromo and Amharic) before data collection. We evaluated respondents’ dietary diversity by relying on the pregnant mother’s recall of food items consumed in the 24 h preceding the survey. A total of ten groups (including (a) grains, white roots and tubers, and plantains (also known as starchy staples); (b) pulses (beans, peas, and lentils); (c) nuts and seeds; (d) dairy; (e) meat, poultry, and fish; (f) eggs; (g) dark green leafy vegetables; (h) other vitamin A-rich fruits and vegetables; (i) other fruits; and (j) other vegetables) were used. Each group was assigned a score of 1 point if they consumed any of the foods in each subgroup at least once in the past 24 h and 0 points if they did not consume the food at all. The minimum dietary diversity score was calculated by adding the number of food categories consumed for 24 h. Participants who consumed five food groups were considered to have adequate dietary diversity, whereas those who consumed less than five food groups were considered to have inadequate dietary diversity.
Quality control
We provided 3 days of training for data collectors on the questionnaire, how to interview, and sampling procedures. A pretest was done on 5% of the samples at Dilchora Hospital with some time gap to decrease information contamination before the actual data collection, and an amendment was made accordingly. A total of six BSc midwives were recruited for the data collection. The principal investigators closely supervised the data collection process.
Data process and analysis
We coded, cleaned, and entered the collected data into EpiData version 3.1 and subsequently exported it to SPSS version 22 (IBM SPSS Statistics, 2013) for analysis. The descriptive analysis was done using frequency tables. Employing binary logistic regression, we used bivariate analysis to establish the relationship between each independent variable and the outcome variable. We considered all variables with a p-value of 0.25 in bivariate analysis eligible for multivariable logistic regression analysis to control for potential confounders and identify true predictors of dietary diversity. We used the variance inflation factor (VIF) and tolerance to test for multicollinearity and found no indication of collinearity effects. We used the Hosmer–Lemeshow goodness-of-fit test to assess model adequacy, and the test yielded a negligible result (p = 0.677), indicating that the model was fit. Finally, we used an adjusted odds ratio and a 95% confidence interval to determine the degree of association between the outcome variable and the independent variables. We used a p-value of 0.05 to declare statistical significance.
Ethical approval
We conducted this study following the guidelines outlined in the Declaration of Helsinki. The Institutional Health Research Ethics Review Committee of Haramaya University, College of Health and Medical Sciences (HU-IHRERC), approved the technical proposal for this study (Ref/No: COH.M.S/100/12940/21). We obtained a permission letter from the hospital administrator. We provided participants with an explanation of the purpose of the research. We told the respondents their participation was fully voluntary and they could opt out at any time or stage of the interview. All study participants provided written informed consent to participate in the study.
Results
Socio-demographic and economic characteristics
In this study, a total of 420 participants were involved with a 100% response rate. The mean (±SD) age of participants was 29.6(±7.1) years. Almost all of the participants 407 (96.9%) were married, and half (52.4%) of them were Oromo. Only 79 (18.8%) of respondents couldn’t read or write, and over two-thirds (74.1%) of respondents were Muslim. In terms of occupation, 128 (30.5%) of respondents were housewives, and 87 (20.7%) had less than 2000 Ethiopian birr (37.95 USD) for monthly family member expenditures. Three hundred sixty-seven (87.4%) of the respondents had families of less than four members, two-thirds (74%) lived in cities, and half (56.8%) of the household heads were between the ages of 30 and 39.
The vast majority of 382 (91 %) respondents’ food sources were found to be purchased from the market. The majority of study participants, 353 (84%), sourced their water from taps, followed by 60 (14.3%) and 7 (1.7%) study participants who get it via pumps and protected wells, respectively. Among the study participants, 293 (69.8%) of them had a private latrine facility, and 141 (48.1%) of them had pit latrines with a slab. About 246 (58.6%) of the study participants engaged in home gardening, and 358 (86.1%) of the respondents had no comorbid illnesses before the data collection period of 4 weeks (Table 1).
Table 1. Socio-demographic characteristics of pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia, 2021
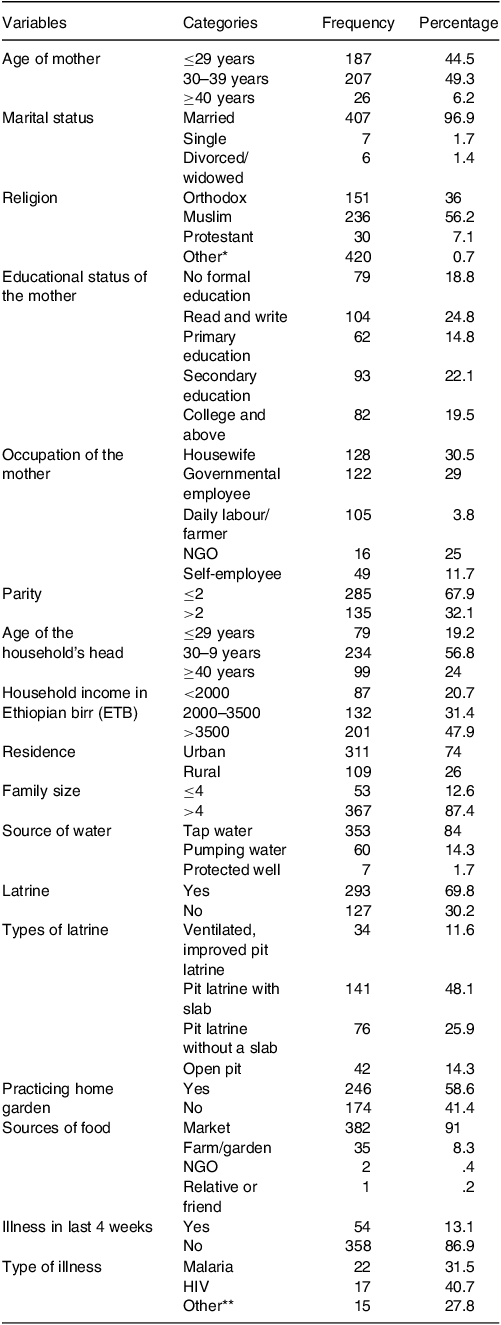
HIV, human immunodeficiency virus; NGO, non-governmental organization; 1ETB, 0.018 USD.
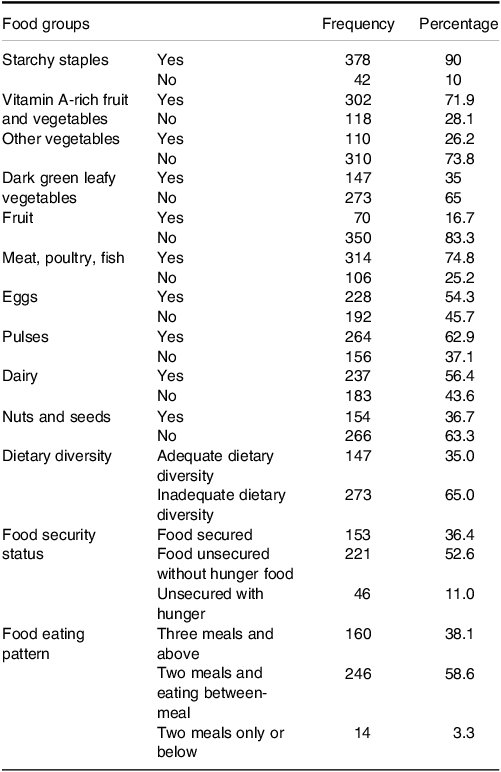
Consumption of food groups, food security, and comorbidity status
In terms of the food groups consumed by pregnant women in the preceding 24 h, the majority of the women 378 (90%) consumed starchy staples. Of them, 110 (26.2%) consumed vitamin A-rich fruit and vegetables, and 154 (36.7%) consumed nuts and seeds. Moreover, foods of animal products were highly consumed by the study participants, with two-thirds (74.8%) consuming meat, poultry, and fish, half (54.3%) consuming eggs, and 237 (56.4%) consuming dairy products. About 147 (35%) of the study population consumed dark green leafy vegetables, and 110 (26.2%) consumed other vegetables (onion, tomato, and eggplants). About 264 (62.9%) consumed pulses, while only 70 (16.7%) consumed fruit. One hundred fifty-three (36.4%) of study participants had secured food, and half (58.6%) of respondents consumed two meals and ate between meals per day (Table 2).
Table 2. Consumption of pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021
Prevalence of dietary diversity score based on 24-hour recall
In the current study, the mean dietary diversity (±SD) score of pregnant mothers was 3.71 ± 2.57 SD with scores ranging from 3 to 8 food groups. The overall prevalence of adequate dietary diversity practice among pregnant women was found to be 35 % (95% CI 30.5 – 39.5) (Fig. 1).
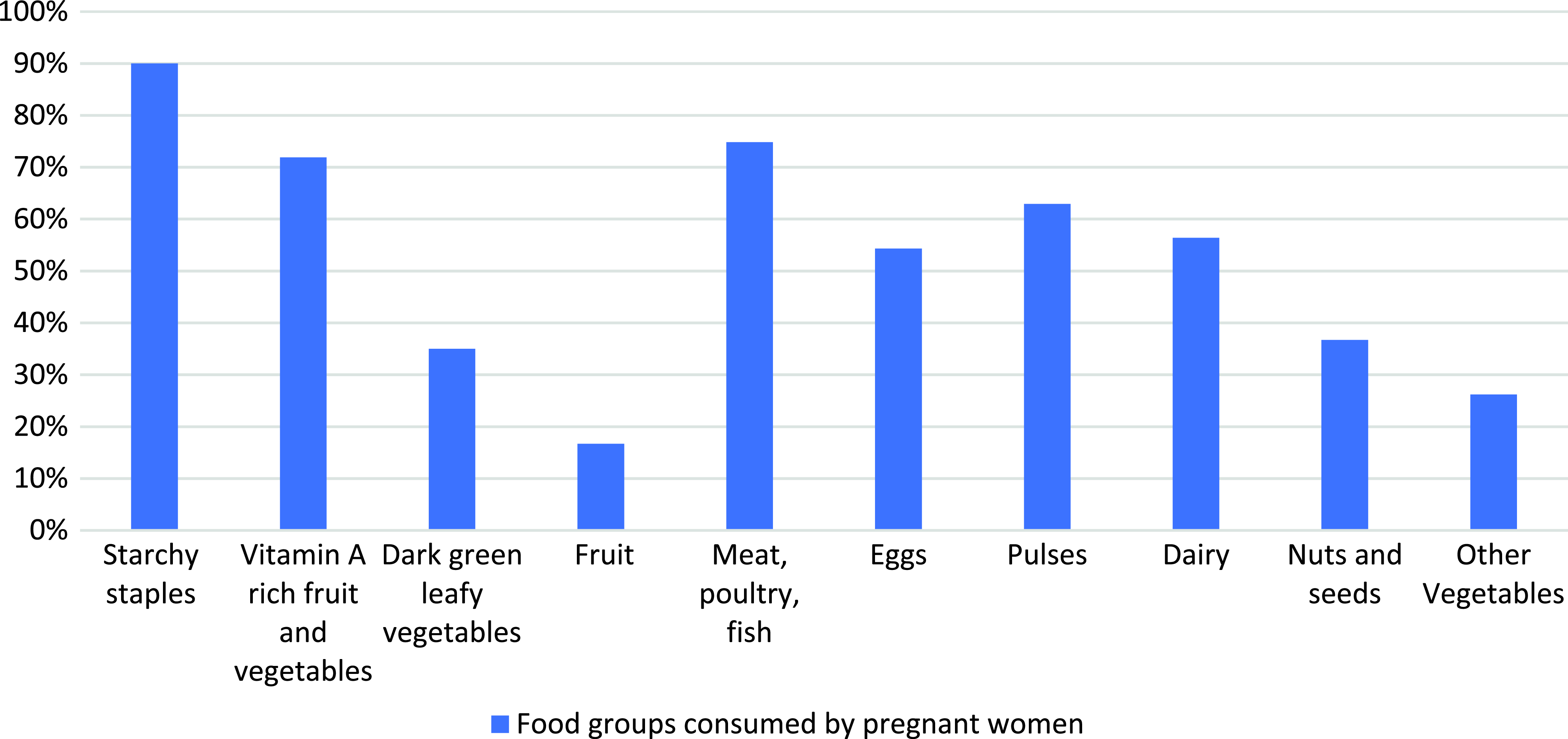
Fig. 1. Food groups consumed by pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia, 2021.
Factors associated with dietary diversity
We used both bivariate and multivariate binary logistic regressions to investigate the relationship between dependent and independent variables. During the bivariate analysis, the educational level, occupation, age, family size, access to latrine, residency, and eating pattern of women were identified as significantly correlated with the dietary diversity of pregnant women in the study area. The multivariable analysis demonstrated that educational level, family size, residency, and eating behaviour were significantly associated with adequate dietary diversity after controlling for potential confounders (Table 3).
Table 3. Factors associated among pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021
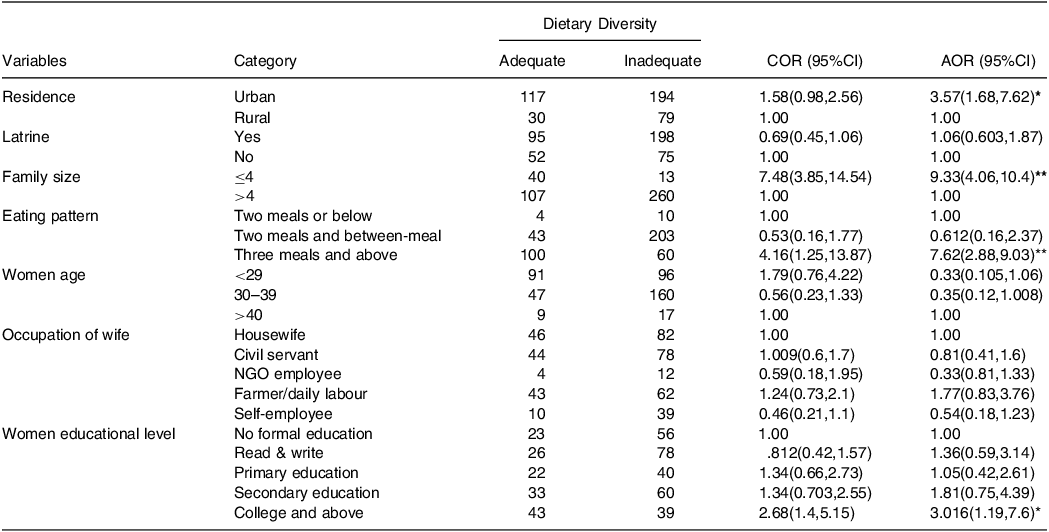
* P-value <0.05.
** P-value = 0.000; CI, confidence interval; COR, crude odds ratio; AOR, adjusted odds ratio.
Participants with a college education or above were three times more likely to have adequate dietary diversity in their diet compared to participants whose education status was elementary school (AOR = 3.01, 95% CI: 1.19 – 7.6). Those who had three meals and above were seven times more likely to have adequate dietary diversity in their diet compared with those who had two meals only and below (AOR = 7.62, 95% CI: 2.88 – 9.03). Respondents who live in urban areas were 3.57 (AOR = 3.57, 95% CI:1.68 – 7.62) times more likely to have adequate dietary diversity in their diet than their counterparts. Those pregnant women who have ≤4 family sizes were nine times more likely (AOR = 9.33, 95% CI: 4.06 – 10.4) to have adequate dietary diversity than those who have >4 (Table 3).
Discussion
The study revealed that about 35% of the pregnant women had consumed ≥5 food groups (adequate dietary diversity), whereas 65% had consumed <5 food groups (inadequate dietary diversity) in the last 24 h. The prevalence of dietary diversity in this study is slightly higher than findings from studies conducted in Shashemane, Ethiopia (25.4%),(Reference Desta, Akibu and Tadese16) and Kenya (20%).(Reference Willy, Judith and Peter7) This discrepancy might be due to variations in the study period, geographical area, socioeconomic, and reporting (hence self-reporting). But it is lower than studies conducted in Gurage zone (42.1%),(Reference Gudeta, Terefe and Mengistu17) Hossana (42.6%),(Reference Kobiro, Delil and Tamiru18) Bale (44.8%),(Reference Hailu and Woldemichael19) Gojjam (55%),(Reference Yeneabat, Adugna and Asmamaw14) Alamata (61.2%),(Reference Jemal and Awol20) and Ghana (46 %).(Reference Saaka, Oladele and Larbi21) The discrepancy may be caused by variations in how dietary diversity was measured and categorised, eating habits, and other socio-demographic factors of women that are found in various areas of the country. Furthermore, socioeconomic status, seasonality, and geographic location may all have a role.(Reference Saaka, Oladele and Larbi21)
The study findings indicated that pregnant women with college or higher education had adequate dietary diversity in their diets, compared to those without formal education. This aligns with similar observations in Alamat, Eastern Gojjam,(Reference Jemal and Awol20) and Hossana, Ethiopia.(Reference Kobiro, Delil and Tamiru18) This might be because educated women are more likely to comprehend nutritional information and incorporate a range of food categories in their meals to achieve the desired level of dietary diversity. Additionally, educated women may participate in income-generating activities, allowing them to buy a variety of foods and adopt a healthy eating attitude.(Reference Murakami, Miyake and Sasaki22)
In our study, respondents who consumed three meals and above had adequate dietary diversity in their diet compared with those who had two meals only and below, which is in line with the findings of studies done in Alamata and Hadiya, Ethiopia.(Reference Kobiro, Delil and Tamiru18,Reference Jemal and Awol20) This might be because increasing the frequency of meals taken by women can help them consume a variety of foods that promote dietary diversity.(Reference Kearney15) Another reason might be the impact of their economic status on diet diversification. Women with a better socioeconomic status may be able to purchase a wider range of food categories more easily, allowing them to increase meal frequency while also improving their nutritional patterns.(Reference Hatløy, Hallund and Diarra23)
Similar to a study in Bale, Ethiopia,(Reference Hailu and Woldemichael19) living in an urban environment is strongly associated with adequate dietary diversity within their diet when compared to individuals who live in a rural area. This could be because city dwellers have easier access to media outlets that disseminate health information and promote public awareness of dietary diversity. Another factor could be that people who live in cities have easy access to well-established marketplaces where they can easily purchase a variety of food items.(Reference Naveena24)
Pregnant women who have ≤4 family sizes had high dietary diversity in their diet compared with those who have >4 family sizes, and this is consistent with data from Bale, Ethiopia.(Reference Hailu and Woldemichael19) This might be because families with fewer members will have a higher chance of having physical and financial access to sufficient food that is safe and nutritious to meet their dietary demands.(4) Furthermore, large family size has an impact on intra-household food distribution, which may necessitate limiting the type and quantity of food groups.(Reference Shahbaz, Haq and Khalid25)
Limitations of the study
The study acknowledges a limitation in assessing dietary diversity, as it relied on participants’ recall. Additionally, the fluctuation of food availability in households across seasons may impact the measured dietary diversity. So, recall bias could not be ruled out completely, and the 24-hour dietary recall may not truly represent the usual intake. Since the study was conducted within the institution, generalising to the entire population is difficult. The MDD-W indicator used in this study was originally designed for women of reproductive age, and currently, no specific MDD indicator exists for pregnant women. Therefore, it is unknown whether they work for pregnant women or not.
Conclusion
This study found that only two in five pregnant women have adequate dietary diversity during antenatal care at Hiwot Fana Specialized University Hospital in Eastern Ethiopia. Factors such as the mother’s level of education, family size, place of residence, and eating habits all had significant effects on dietary diversity among pregnant women. Therefore, promoting women’s education, raising awareness of dietary diversity among rural residents, increasing meal frequency, and providing counselling on family planning utilisation during ANC services are all beneficial in promoting dietary diversity among pregnant women (Fig. 2).
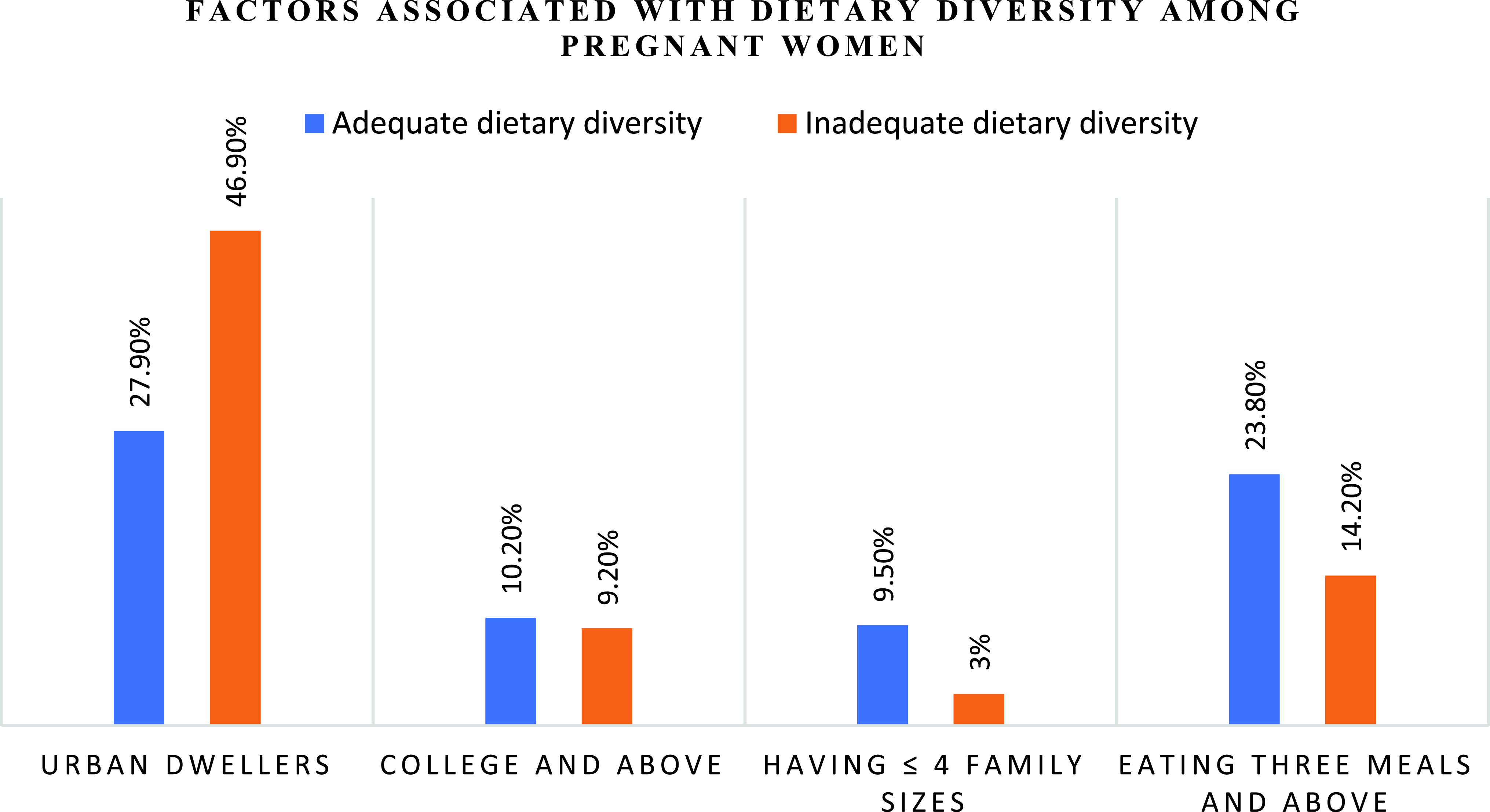
Fig. 2. Factors associated with dietary diversity among pregnant women attending antenatal care at Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021.
Abbreviations
AOR: Adjusted odds ratio; ANC: Antenatal care; CI: Confidence interval; COR: Crude odds ratio; FANTA: Food and Nutrition Technical Assistance Project; FAO: Food and Agriculture Organization; HFSUH: Hiwot Fana Specialized University Hospital; MDD: Minimum dietary diversity; WHO: World Health Organization
Acknowledgements
We thank Haramaya University College of Health and Medical Sciences for reviewing the proposal and providing us with ethical clearance. Our gratitude also goes to the hospital administrators, supervisors, data collectors, and respondents.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted, and agreed to be accountable for all aspects of the work.
The author(s) received no financial support for conducting this research, authorship, and/or publication of this article.
The authors declare that they have no conflicts of interest.









